Abstract
Background: Work in the hospital emergency department (ED) is characterized by a significant (and sometimes excessive) number of patients in relation to medical staff and space and high variability of clinical situations, all in conditions of time deficit. The concept of lean management (LM) may be helpful in solving some of the organizational problems at the ED. One of the tools derived from LM is the 5S method (sort, set in order, shine, standardize and sustain), which serves to organize the workflow, eliminate waste and increase patient safety.
Material and methods: In the ED of University Clinical Hospital in Opole (Poland) we used survey methods (questionnaires, direct interviews and group discussions with the participants) to identify the issues that caused the greatest difficulties in the work flow. 3 months after implementing changes, we conducted a survey among the participating ED nurses and paramedics to obtain opinions on the introduced changes.
Results: Majority of the participants found the implemented changes (e.g. equipment checklists, standardized equipment and supply placement in all ED areas) ”definitely necessary” and ”rather necessary.”
Conclusions: The implementation of LM, particularly the 5S method and checklists, seems to be useful in the organization of work in the ED and was positively assessed by the staff.
Citation
Lisowska A, Kleszczyński J, Wilczek A, Wolf G, Holecki T. Improving workflow at the Emergency Department – simple lessons from the lean management concepts. Eur J Transl Clin Med. 2024;7(2):50-58Introduction
The hospital emergency department (ED) operates 24-hours non-stop and is one of the key elements of the healthcare system. The literature from recent years shows that EDs fill the gaps in healthcare systems around the world by acting as a buffer for patients who do not have a health emergency and for various reasons do not use primary healthcare services at outpatient clinics [1-3].
Due to the above, overcrowding (an excessive number of patients in relation to the staff and space resources) is observed at many EDs around the world [4]. Admitting to the ED patients without severe illness significantly prolongs several processes (e.g. admission and initial stabilization of the patient, diagnostics), burdens the department’s resources and reduces the efficiency of the hospital staff [5]. The boarding of patients (i.e. hospitalizing in the ED patients who are de facto admitted to other hospital departments) significantly extends the ED patient’s length of stay (LOS), causes additional difficulties in the workflow of the ED staff and has been shown to increase in-hospital mortality [6-7].
Solving the above-mentioned problems undoubtedly would require joint effort of healthcare managers (hospital and outpatient clinic managers) together with regional and national health policymakers. In the meantime, it is reasonable to search for tools and solutions at the micro-level, one ED at a time. The literature suggests that some of the difficulties in the ED workflow may be reduced by implementing specific management concepts and tools. Lean healthcare (LH) is a branch of the lean management (LM) concept and together with the 5S method originates from the Japanese industrial sector [8-9]. 5S is an abbreviation of the processes aimed at optimizing the use of equipment and work space: seiri (sort), seiton (set in order), seiso (shine), seiketsu (standardize) and shitsuke (self-discipline). Sometimes a 6th element (safety) is added to the 5S method in the literature, i.e. ensuring the safety of the work environment by identifying potential places that threaten the safety of employees and eliminating them. The methods for this include employee training and using visual management tools, e.g. painting a trace/arc of an opening door on the floor of a busy corridor.
Another aim of the LH concept is the complete elimination of muda (waste), defined as all activities that are not related to patient care/treatment or ending the patient’s stay in the hospital [8-10]. Examples of waste in the ED include the extended LOS resulting from repeated activities (e.g. transporting the same patient several times between the ED and the radiology unit), defective (or missing) equipment and the so-called “bottlenecks” (e.g. waiting for medical triage, waiting for transport to the radiology unit) [11-12]. Authors point that eliminating such types of waste improves the efficiency of staff, increases the patient flow through the ED, thus reducing the overcrowding and costs, while improving the safety and quality of care [12]. However, the complexity of processes/ tasks, resistance to change and lack of standardization are barriers to the implementation of the LH concept in the ED [13]. Therefore, the implementation of LH requires full support of the management staff and medical staff in identifying and eliminating waste, e.g. using data analysis or value stream mapping (a graphic presentation of the stages of the particular process).
Besides 5S, another simple and low-cost tool for optimizing work in the ED are checklists. They can be used as part of the assessment of the availability and function of equipment at the particular area and identifying threats resulting from its deficiencies or defects [14-15]. Checklists allow the employee to quickly detect missing pieces of equipment of individual pieces of equipment through verification and identification by marking individual points [16]. However, it should be remembered that despite low financial costs and the ease of use, their implementation and effectiveness strongly depend on the awareness and motivation of the medical and management staff at every level [17].
Our goal was to implement several solutions derived from LH in the ED of a university hospital. We then analyzed the feedback of the ED nurses and paramedics regarding their satisfaction with the resulting changes in their tasks and in the functioning of their department.
Material and methods
This study was conducted in 2022-2023 in the ED of the University Clinical Hospital (UCH) in Opole (Poland) after obtaining the approval of the hospital Management staff. Bioethics Committee approval was not necessary because this study did not meet the criteria of a medical experiment. The UCH is a public, academic hospital, trauma center (pediatric and adult) as well as the largest hospital in the Opole voivodeship (province). The patient flow at the UCH ED is approximately 150-180 patients per day (approximately 3500-4000 patients per month), which is in the average among EDs in Poland. Nurses and paramedics work 12-hour shifts at the ED. A total of 17 nurses and 16 paramedics participated in this study and voluntarily completed the survey questionnaires. In this study we decided to analyze the workstations and workflow of ED nurses and paramedics only, therefore the ED physicians did not participate.
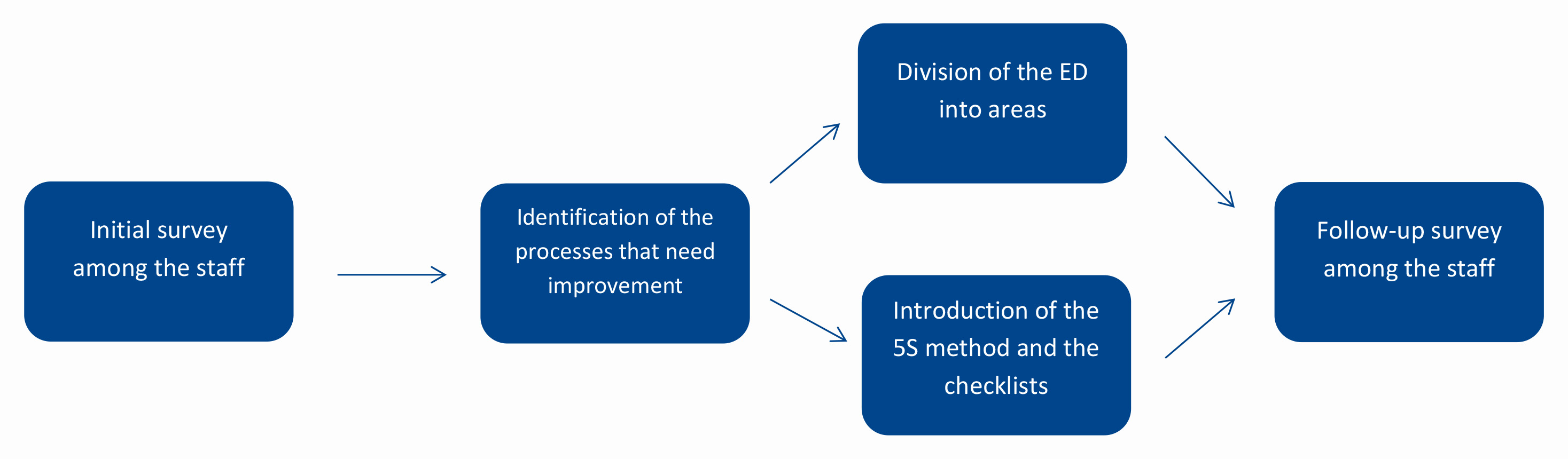
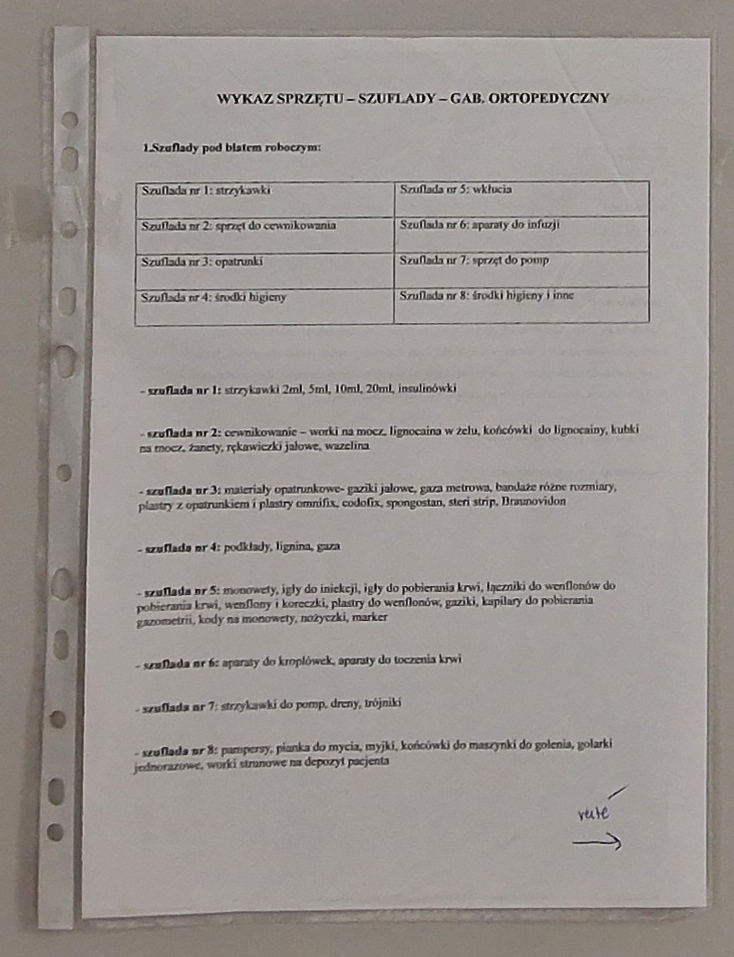
This study consisted of 3 stages. First, we used survey methods (questionnaires, direct interviews and group discussions with the participants) to identify the issues that caused the greatest difficulties in the work flow. The 2nd stage of the study included interventions: the use of the 5S method and checklists in cooperation with the participants. Three months later (3rd stage) we used an original survey questionnaire to collect feedback from the participants regarding the effectiveness of the introduced changes (Figure 1). This was a pilot study, therefore a 3-month observation was chosen.
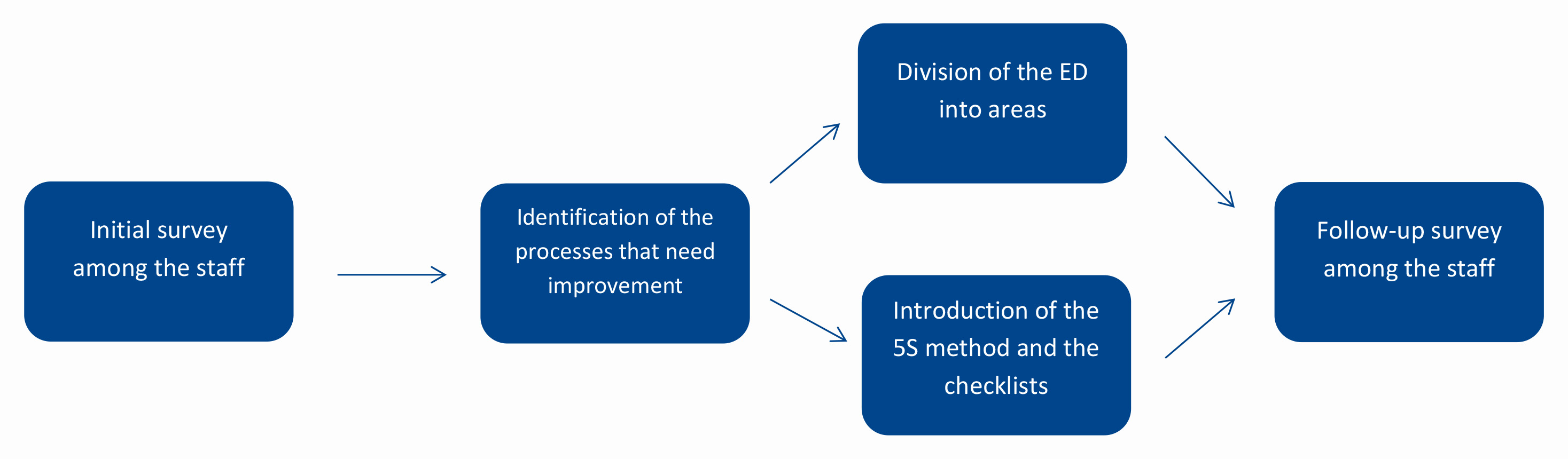
Figure 1. Implementation of LM methods at our Emergency Department
The ED was divided into 6 areas (registration, medical triage, surgical, resuscitation, observation and pediatric) and an “area supervisor” was selected for each area. In addition, 2 appointed “leaders of change” cooperated with the “area supervisors” and monitored the implementation of the 5S method during their shifts in the ED. Although every employee was responsible for implementing 5S in the areas, the “area supervisors” together with the “leaders of change” carried out rounds in accordance with the agreed-upon schedule and checklist of what to check.
The survey questionnaire (developed by the first author) consisted of 31 single-choice closed questions regarding sociodemographic data, job satisfaction, job involvement and organization of work. In this study we analyzed only questions regarding work organization. Returning a completed questionnaire was equivalent to expressing consent to participate in the study.
Data analysis from the survey was performed in R, version 4.2.1 (open-source). Analysis of quantitative variables was performed by calculating the mean, standard deviation, median and quartiles. Analysis of qualitative variables was performed by calculating the number and percentage of occurrences of each value. Comparison of qualitative variable values in groups was performed using the chi-square test (with Yates’ correction for 2 x 2 tables) or Fisher’s exact test where low expected frequencies appeared in the tables. Comparison of quantitative variable values in 2 groups was performed using the Mann-Whitney test. Comparison of quantitative variable values in ≥ 3 groups was performed using the Kruskal-Wallis test. After detecting statistically significant differences, post-hoc analysis was performed using Dunn’s test to identify groups that differed statistically significantly. All p values < 0.05 were interpreted as statistically significant.
Results
Interventions undertaken
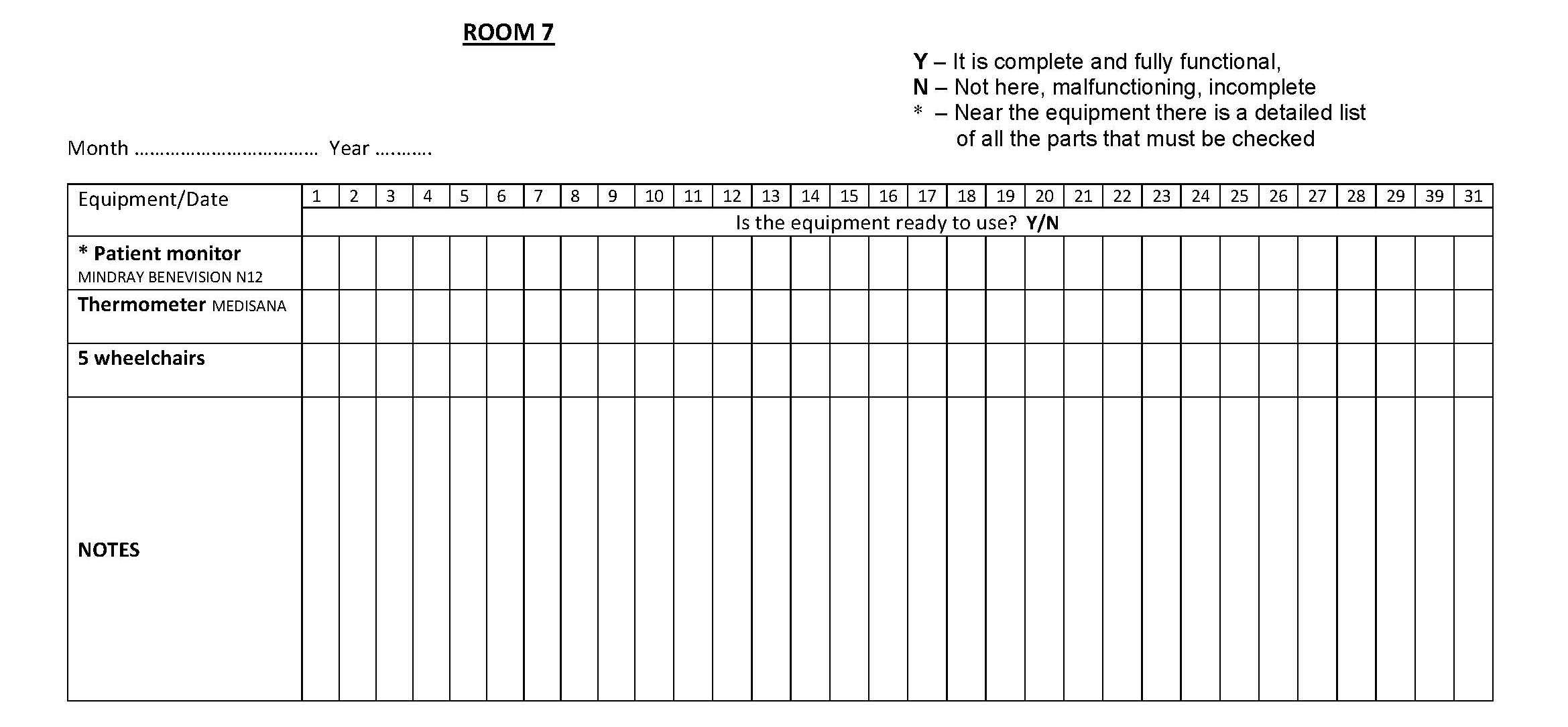
Based on direct interviews with staff, we compiled a list of problems that cause difficulties and waste in everyday work at the ED. The main problems included: shortages of equipment in particular areas and the lack of marking of faulty devices. Interventions were undertaken to eliminate or reduce the number of these problems, which consisted of using the 5S method, visual management, checklists and equipment lists in all areas of our ED (Table 1).
Table 1. Actions taken the ED of the UCH in Opole as part of the 5S method
At the registration desk, the countertops and document cabinets were decluttered using the 5S method. A key panel was installed to make access to keys (and searching for them) easier (Figure 2). Each key was attached to a color-coded key chain: red (keys to rooms in the resuscitation area), green (registration and medical segregation area), blue (isolation area), yellow (observation area), black (staff rooms). A paper list of rooms and their assigned key numbers was placed under the key panel to further ease searching for them.

Figure 2. Example of applying the 5S method at the registration desk
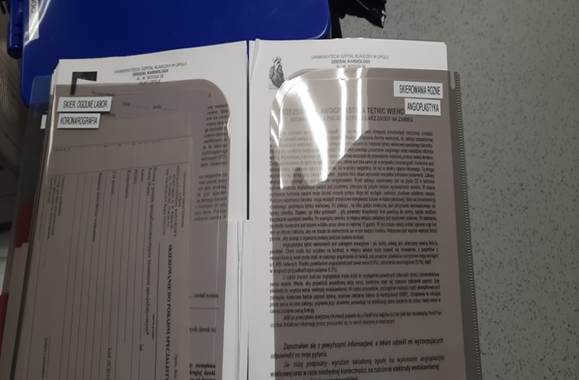
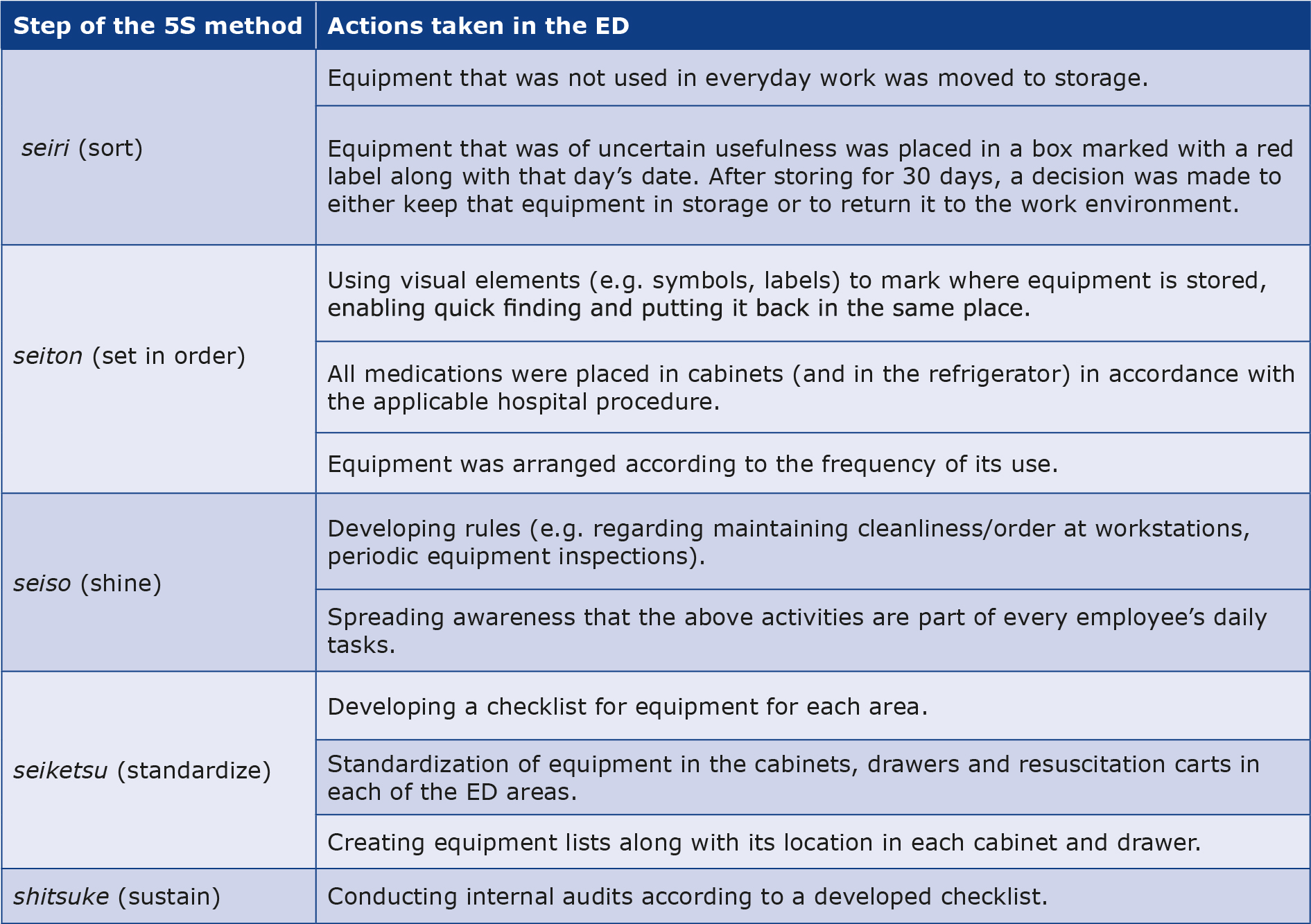
Paper checklists for each ED area were prepared in the form of a table with a list of equipment that should be found in that particular area (Figure 3). The staff recorded the following items: missing piece of equipment at the workstation, equipment malfunction, equipment sent to service, incomplete equipment. The aim was to increase control over the equipment and ensure its efficient function, which is crucial when treating acutely ill patients. After 1 month, the implementation of changes so far was summarized during a department-wide meeting and the staff was asked for verbal feed back and suggestions for further improvements. Duplicates of the same equipment in several rooms were eliminated and errors in the names of some equipment were removed. The checklists were not filled-out completely, which resulted in lower quality of care and less patient safety (e.g. due to not checking the defibrillator battery charge level). In order to solve the problem of incomplete checklists, we removed the detailed lists of parts each of each piece of equipment and left only the particular device name. As a result, the checklists were significantly shortened, use of paper was reduced and the checklist completion has increased.
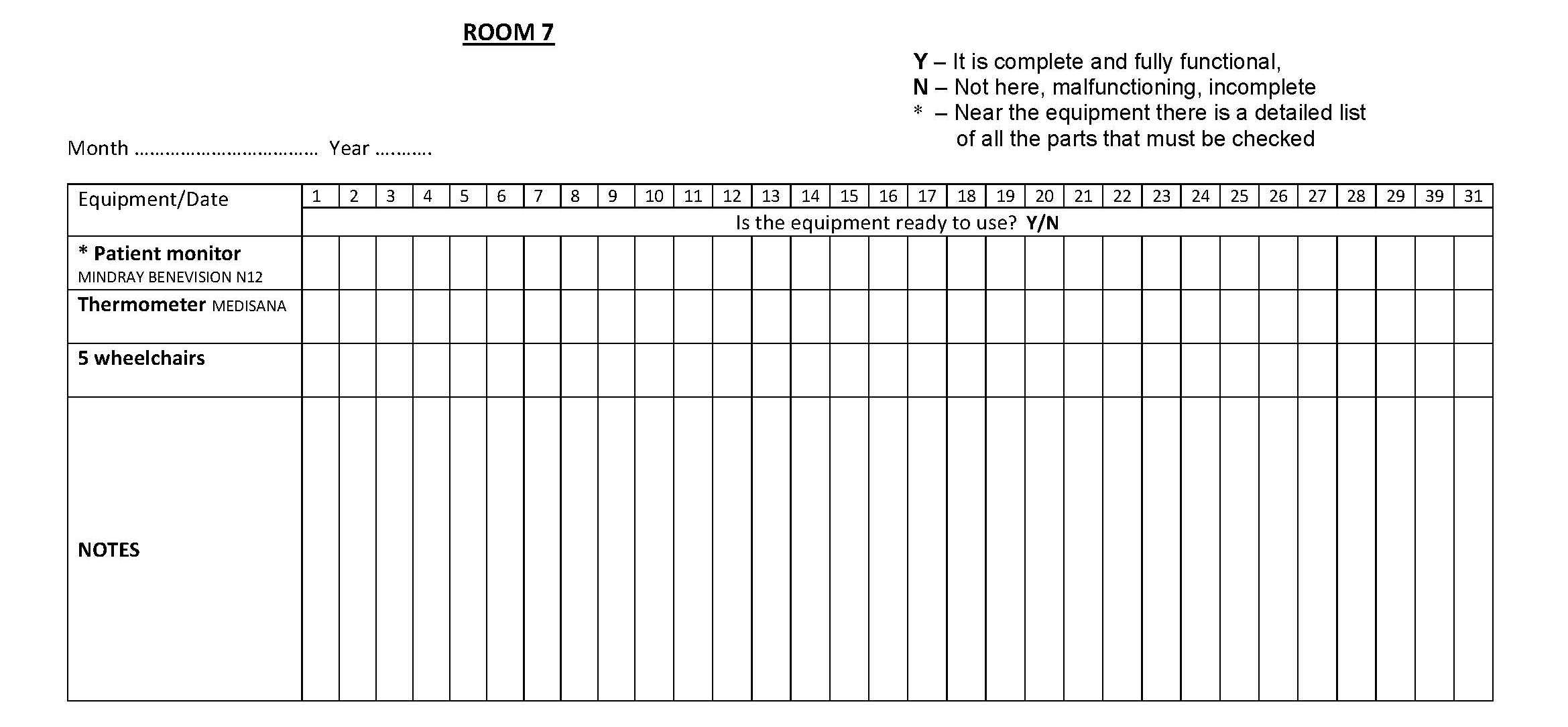
Figure 3. Example of a checklist
For each ED area we created lists of equipment, specifying its exact location in the cabinets and drawers (Figure 4). Such standardization of workstations made it easier to monitor the use of/shortages of supplies and to train new employees. These lists were located in the same place in each room: on the inside of the door to the cabinet where infusion fluids were stored.
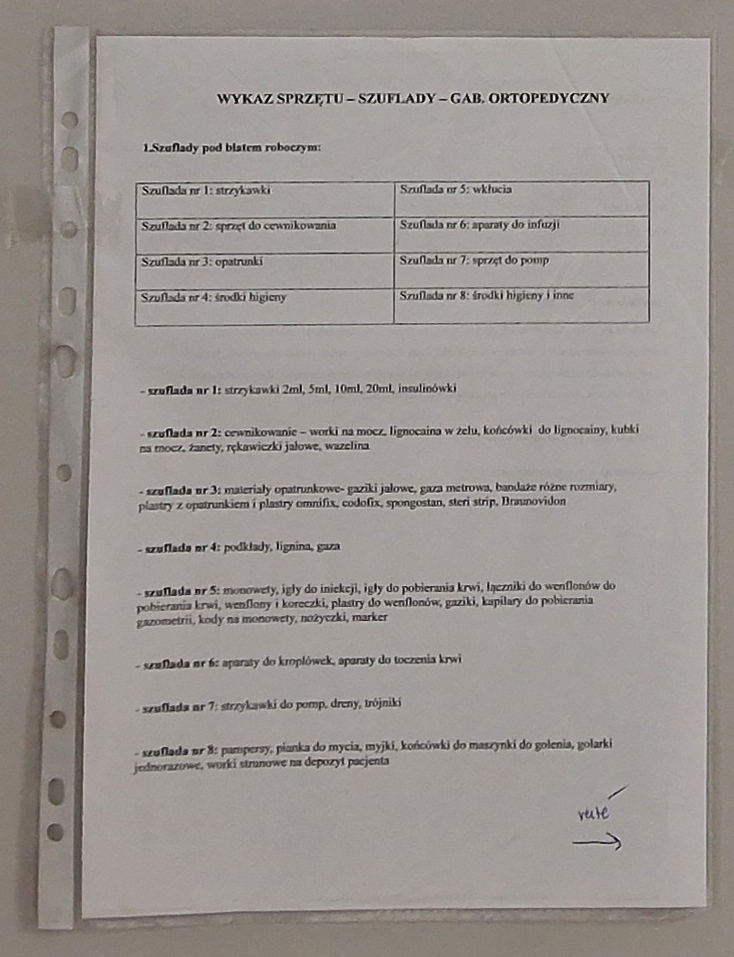
Figure 4. Equipment list
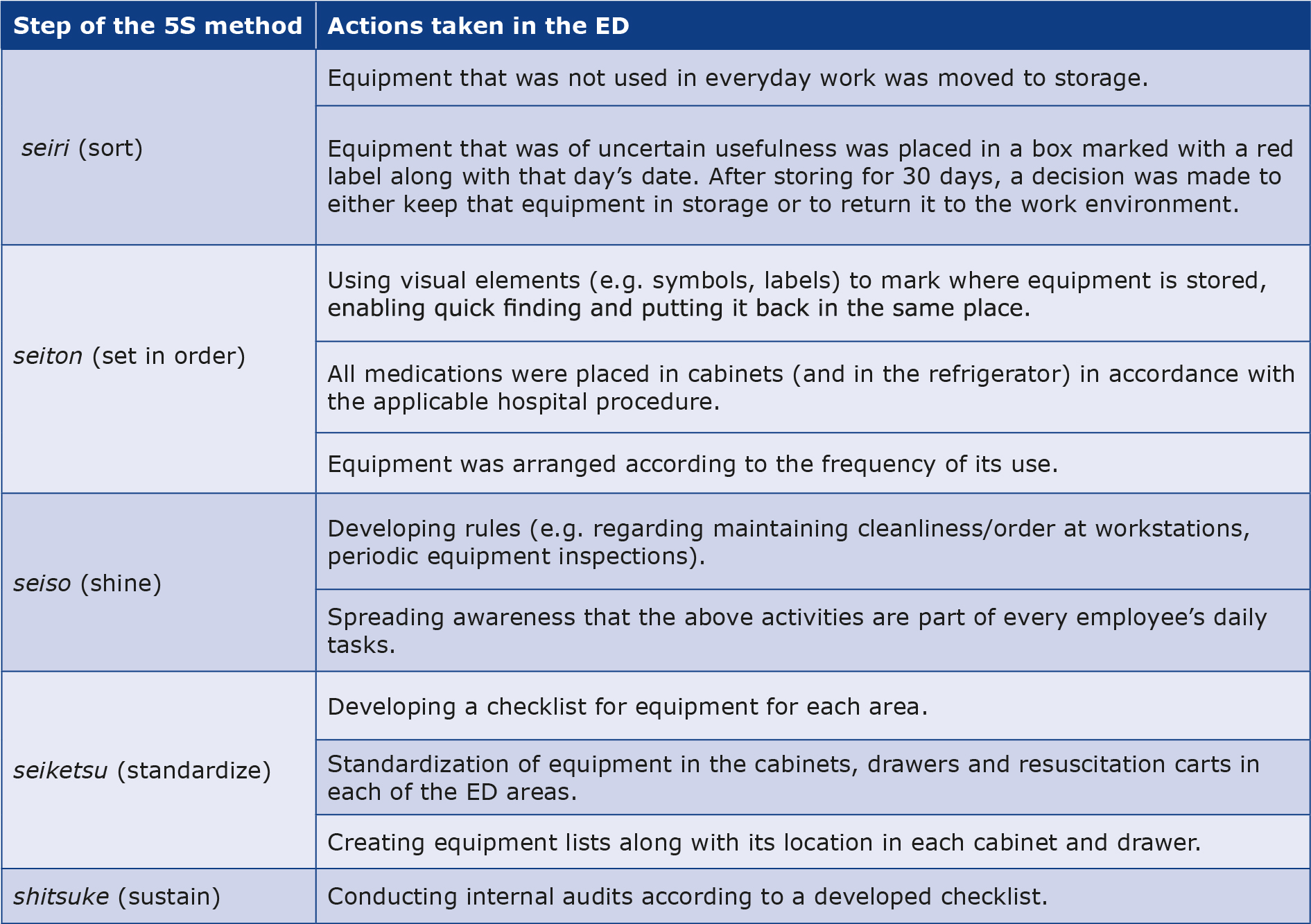
Using visual management, all equipment storage spaces (drawers, cabinets, resuscitation carts) were clearly labeled by placing stickers with a description of the content (Figure 5). Paper documentation was organized in such a way that all the most-frequently used document templates were in one place and were described in such a way that it was visible if any were missing (Figure 6).

Figure 5. Example of visual management
Figure 6. Organizing the paper documentation
Survey study
The assessment of the changes introduced by the nurses and paramedics of our ED was verified using surveys. Nurses constituted 51.51% (n = 17) of the respondents, and the paramedics 48.48% (n = 16). The most frequently marked suggestion regarding the functioning of the department by the staff was the “need for more training”, indicated by 88.24% (15) nurses and all paramedics. During the discussion in groups, the training needs were specified (e.g. medical triage according to the Emergency Severity Index algorithm, interpretation of ECG and management of selected arrhythmias, interpretation of arterial blood gas tests, LM concept and 5S method).
Providing/receiving information on the equipment in the room during each shift was considered “definitely necessary” by 35.29% (6) of nurses and 43.75% (7) of paramedics. It was considered “rather necessary” by 41.18% (7) of nursing staff and 43.75% (7). In both professional groups, nobody considered it “definitely unnecessary”. No significant differences were found between professional groups (p = 1).
Providing/receiving information on the status of disposable equipment and medicines in the particular ED area during each shift was considered “definitely necessary” by 35.29% (6) of nurses and 37.50% (6) of paramedics. It was considered “rather necessary” by 52.94% (9) of nursing staff and 43.75% (7) of paramedics. It was not described as “definitely unnecessary” in any of the groups. There were no significant differences between professional groups (p = 0.647).
Descriptions of the equipment arrangement in each drawer and cabinet were considered “definitely necessary” by 35.29% (6) of nurses and 62.50% (10) of paramedics, whereas 35.29% (6) of nurses and 25% (4) of paramedics considered them “rather necessary”. There descriptions were considered “rather unnecessary” by 17.65% (3) of nursing staff and 6.25% (1) of paramedics. None of the respondents considered them “definitely unnecessary”. No significant differences were found between professional groups (p > 0.499).
Discussion
The literature suggests that the organizational changes that are necessary to implement in the ED include, among others, medical triage training, proper allocation of staff in individual areas, designating a nurse- coordinator on each shift, improvements in the transfer of patients to other hospital departments. The above-mentioned changes increase the level of patient and staff safety [18]. Many management concepts implemented in healthcare facilities (quality management, risk management, process management and human resources management) can lead to increased efficiency, shortened waiting times for a particular service and improved quality of provided healthcare services [19-23]. The LM concept has gained considerable popularity in the recent years [24-27]. The implementation of LM seems to be necessary particularly in the ED, because its ineffective management may affect the functioning of other hospital units [28-29]. In our study, the majority of the participants considered the implemented changes beneficial and necessary.
The benefits of implementation of LM are described most broadly in the context of American hospitals, where it was demonstrated, among other things, that by changing the equipment setup and developing standard work methods, it is possible to shorten the average time of processing histopathological test results from 4 to 3 days, prepare 30% more results and reduce the number of errors in the results of processed diagnostic tests [10]. Verbano et al. indicated that thanks to the implementation of LM in the ED, it is possible to reduce the waiting time for radiological test results, which is valuable for both patients and doctors [30].
Thanks to the introduction of changes related to LM, the waiting time of patients at individual stages of their stay in the ED may be shortened, e.g. the waiting time for triage may be shortened from 3.18 minutes to 2.63 minutes; for the first contact with a doctor from 13.68 minutes to 11.65 minutes, and the total stay from 157.70 minutes to 117.71 minutes [31]. Even such minor changes seem significant, considering that the average LOS in the ED is about 258 minutes, of which 80% are spent on activities that do not provide value from the patient’s point of view (e.g. waiting for diagnostic test results, waiting for a specialist’s consultation, waiting for discharge report). The shortening of the total stay as a result of implementing LM is also noted the literature review by Tlapa et al., showing that it may be shortened by up to 142 minutes [32]. One of the changes may be the use of visual management to mark paths and rooms in the ED, which reduces the time triage staff must spend explaining the patient’s way to a given area [33]. Other researchers also point to the benefits of implementing LM in terms of speeding up the flow of patients through the ED [31, 34-35]. In our study, we also used visual management tools (stickers describing the contents of each cabinet and drawer, Figure 5).
The LM concept can help eliminate waste in the ED, such as the duplication of information in paper forms/record books and in the computer system. Another example is organizing the medicines by simply dividing them into 3 groups and marking them with colors (e.g. green – used in large quantities, yellow – used irregularly, red – used exceptionally rarely), adjusting their orders to the actual demand [36]. Similarly, in our study we standardized the way all medications were ordered in each cabinet and refrigerator), so that the staff spend less time searching for them or checking their quantities. Furthermore, we sorted all pieces of equipment and removed to storage those which were not used in daily work or were of uncertain usefulness (Table 1).
By combining the LeanSixSigma concept (a quality improvement method that identifies problems before they occur) in the EDs of 3 hospitals in Florida (USA), the overall LOS indicator was improved by 22-26%, which increased patient satisfaction from the 61st percentile to > 90th, with simultaneous savings of $4-7 million. This was achieved by streamlining the triage process, reorganizing the medical triage area, standardizing procedures by introducing clinical guidelines into everyday practice (mainly regarding the method of performing specific medical procedures) and eliminating the socalled “bottlenecks” [37]. Although we were not able to analyze specific time-related data, in our study we eliminated one potential bottleneck (time wasted on searching for keys) by creating a key panel and labeling each key with a color-coded key chain (Figure 2).
Alowad et al. presented a holistic approach to optimizing the work of the ED. The opinions of staff and patients were taken into account, patient flow maps were developed and the so-called “bottlenecks” were identified (e.g. waiting for registration or for imaging tests). The authors showed that the reasons for the overload of the ED are, among others, in the area of management (e.g. lack of standardized documentation, inefficient system for reporting problems), in the number and experience of nursing and medical staff, in the area of quality (e.g. lack of a developed training plan, lack of a quality improvement team in the ED), in the area of patients (lack of awareness of when to report to the ED) and in the area of the department’s resources. [38]. In our study we also noted lack of standardized paper documentation and organized it accordingly in all areas of our ED (Figure 6).
Barriers to implementing changes in the ED include ignoring the value that can be obtained thanks to motivated and energetic staff [37]. The feedback of medical staff on the changes being introduced may contribute, among other things, to greater motivation to undertake actions and identification with the unit. For the successful optimization of ED management, it is necessary to raise staff awareness of selected management concepts and tools through training and education, enabling employees to submit ideas for improvements and solve problems [39-41]. This correlates with our results that show that ED nurses and paramedics expect more training and is willing to participate in it.
Further research directions
There is a lack of current research on the effectiveness of management concepts (including LH) in optimizing the functioning of Polish healthcare facilities. While conducting such studies it would be important to take into account the impact of this implementation on the patient’s LOS at all stages and on the total stay in the ED. It would also be important to identify the processes taking place in the ED, visualize them and identify the so-called “bottlenecks”, which would directly affect their improvement, which is crucial in the conditions prevailing in the ED.
Limitations
The main limitation of this study is the lack of data on the patient’s LOS in the ED at its individual stages (e.g. time to triage, time to first contact with a doctor, time from ordering tests to results, etc.) and the overall LOS. Unfortunately we were not able to complete that dataset. That information would allow precise identification of the previously mentioned “bottlenecks,” analysis of the reasons for their occurrence and development of solutions. Another limitation is the lack of a “before and after” analysis using a similar observation period prior to the LH-related interventions, which could have provided more information on their influence on the workflow at our ED. In addition, a longer observation period (6 months or 1 year) would allow for a more thorough analysis. Furthermore, extending our study to other EDs would allow for generalization of the results and development of good practices regarding optimization of the work of these departments.
Conclusions
Although the LM methodology derives from the manufacturing sector, its tools are easily available and can be successfully implemented by healthcare staff in their daily work. Changes in the organization of work resulting from the use of LM (particularly the 5S and checklist techniques) at our ED/ study site were positively assessed by the medical staff.
Conflict of interest
None.
Funding
None.
-------
Image – Arkadiusz Kuźmiński / "Chose-Fotografia"
References
| 1. |
Lindner G, Woitok BK. Emergency department overcrowding. Wien Klin Wochenschr [Internet]. 2021 Mar 13;133(5–6):229–33. Available from: http://link.springer.com/10.1007/s00508-019-01596-7.
|
| 2. |
Butun A, Kafdag EE, Gunduz H, Zincir V, Batibay M, Ciftci K, et al. Emergency department overcrowding: causes and solutions. Emerg Crit Care Med [Internet]. 2023 Dec;3(4):171–6. Available from: https://journals.lww.com/10.1097/EC9.0000000000000078.
|
| 3. |
Informacja o wynikach kontroli. Funkcjonowanie systemu ratownictwa medycznego. Nr ewid. 176/2020/P/19/105/LWA [in Polish] [Internet]. Warszawa; 2020. Available from: https://www.nik.gov.pl/plik/id,23528,vp,26262.pdf.
|
| 4. |
Velt KB, Cnossen M, Rood PPM, Steyerberg EW, Polinder S, Lingsma HF. Emergency department overcrowding: a survey among European neurotrauma centres. Emerg Med J [Internet]. 2018 Jul;35(7):447–8. Available from: https://emj.bmj.com/lookup/doi/10.1136/emermed-2017-206796.
|
| 5. |
Sartini M, Carbone A, Demartini A, Giribone L, Oliva M, Spagnolo AM, et al. Overcrowding in Emergency Department: Causes, Consequences, and Solutions—A Narrative Review. Healthcare [Internet]. 2022 Aug 25;10(9):1625. Available from: https://www.mdpi.com/2227-9032/10/9/1625.
|
| 6. |
Laam LA, Wary AA, Strony RS, Fitzpatrick MH, Kraus CK. Quantifying the impact of patient boarding on emergency department length of stay: All admitted patients are negatively affected by boarding. J Am Coll Emerg Physicians Open [Internet]. 2021 Apr 2;2(2). Available from: https://onlinelibrary.wiley.com/doi/10.1002/emp2.12401.
|
| 7. |
Gaddis GM. Emergency Medicine: a specialty that deserves “re-branding,” because it enables large financial savings! Eur J Transl Clin Med [Internet]. 2023 Sep 19;6(2):5–9. Available from: https://ejtcm.gumed.edu.pl/articles/171885.
|
| 8. |
Shingo S. A Revolution in Manufacturing: The SMED System. The Japan Management Association; 1983.
|
| 9. |
Ohno T, Bodek N. Toyota Production System: Beyond Large-Scale Production. 1st ed. Productivity Press; 1988.
|
| 10. |
Graban M. Lean Hospitals - improving hospitals. Improving quality, patient safety and staff satisfaction. ProdPublishing; 2010.
|
| 11. |
Lisiecka-Biełanowicz M, Lisiecka K. Lean healthcare in hospital emergency department. Case study. Sci Pap Silesian Univ Technol Organ Manag Ser [Internet]. 2020;2020(143). Available from: http://managementpapers.polsl.pl/wp-content/uploads/2020/05/143-Lisiecka-Biełanowicz-Lisiecka.pdf.
|
| 12. |
Tiso A, Crema M, Verbano C. A framework to guide the implementation of lean management in emergency department. J Health Organ Manag [Internet]. 2021 Dec 17;35(9):315–37. Available from: https://www.emerald.com/insight/content/doi/10.1108/JHOM-01-2021-0035/full/html.
|
| 13. |
Kautsch M. Characteristics of healthcare facility management. In: Healthcare Management New Challenges. 2nd ed. Wolters Kluwer; 2015. p. 96–9.
|
| 14. |
Kautsch M. Zarządzanie w opiece zdrowotnej. Nowe wyzwania [in Polish] [Internet]. Warszawa: Wolters Kluwer; 2015. Available from: https://www.ibuk.pl/fiszka/209781/zarzadzanie-w-opiece-zdrowotnej-nowe-wyzwania.html?srsltid=AfmBOoqIexyOsObU5ZS-wuP7vO4SCevOjCl34KhLO78FA6ezKD4tRid8.
|
| 15. |
Ingaldi M, Grodecki A. Identyfikacja zagrożeń w środowisku pracy za pomocą list kontrolnych. Arch Wiedzy Inżynierskiej [Internet]. 2023;8(1). Available from: https://bibliotekanauki.pl/articles/24085332.pdf.
|
| 16. |
Machtyl A. Optimization of work time and management in a radiotherapy department in the light of reports presented at the ESTRO 35 conference in Turin. Lett Oncol Sci [Internet]. 2018;15(1):6–10. Available from: https://journals.wco.pl/index.php/los/article/view/52/60.
|
| 17. |
Preś I, Dudek M. Lean Management solutions in healthcare facilities worldwide. Case study: implementation of Lean Management methods in the Regional Nephrology Center in Szczecinek. In Different faces of logistics. Collection of students’ works [in Polish]. In: Różne oblicza logistyki Zbiór prac studentów [Internet]. Wydawnictwo Uniwersytetu Łódzkiego; 2018. Available from: http://hdl.handle.net/11089/26049.
|
| 18. |
Milton J, Chaboyer W, Åberg ND, Erichsen Andersson A, Oxelmark L. Safety attitudes and working climate after organizational change in a major emergency department in Sweden. Int Emerg Nurs [Internet]. 2020 Nov;53:100830. Available from: http://www.crossref.org/deleted_DOI.html.
|
| 19. |
Wruk-Złotowska A. Safety of clinical processes for patient nephrology care. Ren Dis Transplant Forum [Internet]. 2014;7(4):274–80. Available from: https://journals.viamedica.pl/renal_disease_and_transplant/article/view/40870.
|
| 20. |
Sasak J. Zarządzanie ryzykiem w placówkach ochrony zdrowia [in Polish] [Internet]. Wolters Kluwer; 2020. (Poradniki ABC Zdrowie). Available from: https://books.google.pl/books?id=F_dPEAAAQBAJ.
|
| 21. |
Zł☼otowska K. Praktyczny przewodnik po lean healthcare [in Polish]. Toruń•: Lean Hospitals Publishing House; 2020. 66–67 p.
|
| 22. |
Złotowska K. Lean healthcare w ochronie zdrowia – pierwszy projekt w Polsce [in Polish] [Internet]. Lean Hospitals. 2016 [cited 2024 Dec 20]. Available from: https://leanhospitals.pl/lean-healthcare-w-ochronie-zdrowia-pierwszy-projekt-w-polsce/.
|
| 23. |
Ksykiewicz-Dorota A. Zarzdzanie zasobami ludzkimi [in Polish]. In: Zarządzanie w pielęgniarstwie Podręcznik dla studentów studiów magisterskich Wydziałów Pielęgniarstwa oraz Wydziałów Nauk o Zdrowi [Internet]. Warsaw: PZWL Wydawnictwo Lekarskie; 2022. p. 177. Available from: https://www.ibuk.pl/fiszka/146555/zarzadzanie-w-pielegniarstwie.html?srsltid=AfmBOoqvEXAFzEj54HJkfoJaK2t0x8F042aNFaz0eIJYa6_K3M4EmYhO.
|
| 24. |
Ferreira GSA, Silva UR, Costa AL, Pádua SID de D. The promotion of BPM and lean in the health sector: main results. Bus Process Manag J [Internet]. 2018;24(2):400–24. Available from: https://www.emerald.com/insight/content/doi/10.1108/BPMJ-06-2016-0115/full/html.
|
| 25. |
Mahmoud Z, Angelé-Halgand N. L’industrialisation des blocs opératoires : Lean Management et réification. Manag Avenir Santé [Internet]. 2018;N° 3(1):73–88. Available from: https://www.cairn.info/revue-management-et-avenir-sante-2018-1-page-73.htm?ref=doi.
|
| 26. |
Rotter T, Plishka C, Lawal A, Harrison L, Sari N, Goodridge D, et al. What Is Lean Management in Health Care? Development of an Operational Definition for a Cochrane Systematic Review. Eval Health Prof [Internet]. 2019;42(3):366–90. Available from: http://journals.sagepub.com/doi/10.1177/0163278718756992.
|
| 27. |
Tay HL. Lean Improvement Practices: Lessons from Healthcare Service Delivery Chains. IFAC-PapersOnLine [Internet]. 2016;49(12):1158–63. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2405896316309363.
|
| 28. |
Cegłowska U, Brzozowski S, Hermanowski T, Chmielewska M. Zastosowanie koncepcji lean management w Szpitalnych Oddziałach Ratunkowych. Przegląd Organ [Internet]. 2019 Dec 31;46–52. Available from: http://www.przegladorganizacji.pl/artykul/2019/10.33141po.2019.12.06.
|
| 29. |
Breen LM, Trepp R, Gavin N. Lean Process Improvement in the Emergency Department. Emerg Med Clin North Am [Internet]. 2020 Aug;38(3):633–46. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0733862720300432.
|
| 30. |
Verbano C, Crema M. Applying lean management to reduce radiology turnaround times for emergency department. Int J Health Plann Manage [Internet]. 2019 Oct 8;34(4). Available from: https://onlinelibrary.wiley.com/doi/10.1002/hpm.2884.
|
| 31. |
Chan H, Lo S, Lee L, Lo W, Yu W, Wu Y, et al. Lean techniques for the improvement of patients’ flow in emergency department. World J Emerg Med [Internet]. 2014;5(1):24. Available from: http://wjem.com.cn/EN/10.5847/wjem.j.issn.1920-8642.2014.01.004.
|
| 32. |
Tlapa D, Zepeda-Lugo CA, Tortorella GL, Baez-Lopez YA, Limon-Romero J, Alvarado-Iniesta A, et al. Effects of Lean Healthcare on Patient Flow: A Systematic Review. Value Heal [Internet]. 2020 Feb;23(2):260–73. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1098301519352179.
|
| 33. |
Zamani Z. Effects of Emergency Department Physical Design Elements on Security, Wayfinding, Visibility, Privacy, and Efficiency and Its Implications on Staff Satisfaction and Performance. HERD Heal Environ Res Des J [Internet]. 2019 Jul 19;12(3):72–88. Available from: https://journals.sagepub.com/doi/10.1177/1937586718800482.
|
| 34. |
Hogan B, Rasche C, von Reinersdorff AB. The First View Concept. Eur J Emerg Med [Internet]. 2012 Jun;19(3):136–9. Available from: http://journals.lww.com/00063110-201206000-00002.
|
| 35. |
Le DX, Do HT, Bui KT, Hoang TQ, Nguyen GH, Nguyen A V., et al. Lean management for improving hospital waiting times—Case study of a Vietnamese public/general hospital emergency department. Int J Health Plann Manage [Internet]. 2022 Jan 6;37(1):156–70. Available from: https://onlinelibrary.wiley.com/doi/10.1002/hpm.3310.
|
| 36. |
Owczarczak K, Hermanowski T, Chmielewska M. Lean management methods in managing medication in Polish hospitals [in Polish]. Farm współczesna [Internet]. 2018;(11). Available from: https://www.akademiamedycyny.pl/wp-content/uploads/2018/07/Farmacja_1_2018_04.pdf.
|
| 37. |
Eitel D, Shiver JM, Guła P, Korona M. Szpitalny oddział ratunkowy: zarządzanie operacyjne i optymalizacja [in Polish] [Internet]. Wolters Kluwer Polska; 2012. Available from: https://www.profinfo.pl/sklep/szpitalny-oddzial-ratunkowy-zarzadzanie-operacyjne-i-optymalizacja,128101.html#opis.
|
| 38. |
Alowad A, Samaranayake P, Ahsan K, Alidrisi H, Karim A. Enhancing patient flow in emergency department (ED) using lean strategies–an integrated voice of customer and voice of process perspective. Bus Process Manag J [Internet]. 2021 Jan 25;27(1):75–105. Available from: https://www.emerald.com/insight/content/doi/10.1108/BPMJ-11-2019-0457/full/html.
|
| 39. |
Improta G, Romano M, Di Cicco MV, Ferraro A, Borrelli A, Verdoliva C, et al. Lean thinking to improve emergency department throughput at AORN Cardarelli hospital. BMC Health Serv Res [Internet]. 2018 Dec 3;18(1):914. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3654-0.
|
| 40. |
Mazzocato P, Holden RJ, Brommels M, Aronsson H, Bäckman U, Elg M, et al. How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children’s hospital, Stockholm, Sweden. BMC Health Serv Res [Internet]. 2012 Dec 1;12(1):28. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-12-28.
|
| 41. |
Dekier ukasz, Grycuk A. Employee Suggestion Schemes: Experiences of Polish Companies. SSRN Electron J [Internet]. 2014; Available from: http://www.ssrn.com/abstract=2632825.
|