Emergency Medicine: A specialty that deserves ”re-branding”, because it enables large financial savings! (This may seem counter-intuitive, but it’s true)
Abstract
Emergency departments are costly to maintain. They remain open every hour of the year to provide care for those who need it, when they need it. Therefore, emergency departments are a crucial resource for any modern society, and no sensible person would want to close them, despite their cost. However, the view held by many, that the care provided in an emergency department is excessively costly, is just plain wrong. When our doctors’ and our specialty’s performance is viewed objectively, it becomes clear that emergency physicians have become crucial agents of cost savings. Therefore, EPs have earned the right to proudly “re-brand” themselves not as high-cost care providers, but as indispensable, money-savers in any nation’s health care enterprise. If you don’t believe that, continue reading this commentary.
Citation
Gaddis G M. Emergency Medicine: A specialty that deserves ”re-branding”, because it enables large financial savings! (This may seem counter-intuitive, but it’s true). Eur J Transl Clin Med. 2023;6(2):5-9Roles and availability of Emergency Departments
As “background information,” those who allege that emergency care is too costly and should in most cases be provided in outpatient clinics overlook at least four critical facts:
First, much of the emergency care we provide could not be provided in an outpatient clinic or a doctor’s office. Could you imagine treating a polytrauma patient, a cerebrovascular accident (“stroke”) patient or acute S-T elevation myocardial infarction (STEMI) patient in an outpatient clinic? Of course not!
Second, most urgent and emergent medical problems don’t happen just on weekdays, while the sun is in the sky. Patients often need to be able to access medical care when doctors’ offices are closed. If an outpatient clinic remains open from 09:00 until 17:00 on weekdays, even if these clinicians in that facility are able to accommodate a few “urgent” appointment requests, they are available for only 40 hours, or 23.8%, of a 168-hour week.
Third, we have implemented research findings to safely decrease costs of care via processes which did not exist when I entered emergency medicine (EM) residency training in 1986. This implementation of research findings saves considerable sums of money.
Fourth, the public’s need for inpatient care ebbs and flows, and when a hospital is operating “above capacity”, the emergency department is typically where that care is provided. Provision of inpatient-level care in an emergency department is less expensive than would be the case if a hospital spent money to add sufficient bed capacity to enable that happy day when ED boarding of patients never had to occur.
Points number 1 and 2, and especially point 4, should all be obvious, yet are sometimes not overtly acknowledged. They will not be further discussed, except for asking you, the readers, to imagine the cost to a hospital system, if it expanded its inpatient capacity sufficiently such that ED boarding of to-be-admitted patients was rarely required!
We leverage research findings to save money
Regarding the third point, the leveraging of research findings, an important development that can easily be taken for granted, here are some illustrative examples demonstrating how EPs save health care systems money every day, when 1986 is compared to 2023:
- In 1986, all patients with acute pyelonephritis were admitted for several days of inpatient intravenous (IV) antibiotic therapy. Now, many of these patients receive one dose of an IV antibiotic, plus analgesia and an antiemetic, in the ED. Once they demonstrate that their nausea and vomiting is controlled, most of these patients are then prescribed oral antibiotics, analgesics and antiemetics, and discharged. Acute pyelonephritis has become a disease for which emergency physicians can contribute cost savings, because less expensive outpatient management is often feasible and appropriate [1].
- In 1986, most patients with pelvic inflammatory disease (PID) were admitted for several days of IV antibiotics, under the now-disproven dogma that IV antibiotics decreased the scarring of the Fallopian tubes and enhanced the patient’s future fertility. Now, many patients with PID are treated and released after ED administration of appropriate antibiotics to eradicate possible infection by Neisseria gonorrhea and Chlamydia trachomatis, often with added treatment for anaerobic microbes, and an oral antibiotic upon home-going. Female upper genital tract disease has been transformed to another disease for which emergency physicians can contribute cost savings, because less expensive outpatient management is often feasible and appropriate [2].
- In 1986 all patients diagnosed with the venous thromboembolic (VTE) diseases of deep venous thrombosis (DVT) or acute pulmonary embolism (PE) were admitted for several days of inpatient care to enable therapy with intravenous heparin as a bridge to oral warfarin. Warfarin pills are inexpensive, but the associated care is not. Warfarin is a drug highly prone to drug-drug and drug-food interactions [3]. Further, warfarin dosing requires regular monitoring of the International Normalized Ratio (INR), both a cost and an inconvenience to patients. Fortunately, we first learned we could safely treat most patients with DVT as outpatients by prescribing direct oral anticoagulants (DOACs) such as Factor Xa Inhibitors. Subsequently, we also learned that patients with PE without hypoxia or evidence of right heart failure can safely be discharged home with DOAC prescriptions. DVT and PE have been transformed to diseases for which emergency physicians can contribute cost savings, because they usually can implement feasible and appropriate outpatient management [4].
- In 1986, chest pain patients without an S-T Elevation Acute Myocardial Infarction (STEMI), whose pain was suspected to be cardiac in nature, became inpatients for sequential monitoring of their Lactate Dehydrogenase (LDH) and Creatine Kinase (CK) isozyme profiles. This process required at least a full day and an overnight inpatient stay. Now, for selected patients, EPs can leverage low and non-rising high sensitivity troponin values and a low “HEART score” to safely implement outpatient follow-up plans, within hours, sparing an inpatient admission. Chest pain has been transformed to a chief complaint for which emergency physicians can contribute cost savings, because outpatient management can be feasible and appropriate [5].
- In 1986, a complete workup of many other diseases also required several days of inpatient care. Thanks to improved systems of care and better implementation of medical evidence, patients who used to be admitted for their multi-day “workup” can occasionally be “treated and released”. For example, a hospital at which I had worked in the past had a dedicated fast track pathway for patients diagnosed with transient ischemic attacks (TIA). Most of our patients with TIA who did not need an urgent vascular procedure to protect them against a near-term stroke were treated and released from the ED observation area within 12 hours of their arrival. This expedites hospital throughput and saves significant sums of money.
- A further benefit of all of these examples is that patients with these diseases can be returned to work much more quickly than in past years, enhancing overall workforce productivity in a nation’s economy.
Further improvements are possible
We could do even better at implementing cost savings, if only our patients would permit it. We already know how to apply validated and highly reliable clinical decision rules (CDRs) such as the Ottawa Ankle Rules, the Ottawa Knee Rules, the NEXUS and Canadian C Spine Rules, and the PECARN (for children) and Canadian Head CT (for adults) Rules [6-11]. All perform with high accuracy and validity. However, we know that patients often expect radiographs that these CDRs would establish as contraindicated.
Our collective experience is that there is a significantly long time required to explain these CDRs to patients, so it becomes more costand time-effective to simply obtain the non-indicated imaging. Consider this idea for the future: create educational modules that present advocacy to patients to allow doctors to implement these CDRs. This education could be efficiently accomplished if patients were enabled to view effective bedside “plug and play” teaching tools, explaining those CDRs. Such resources could dissuade patients of their false beliefs and persuade them to agree that omission of the contraindicated radiographs, tests which they believed they needed upon their ED arrival, represents appropriate care. This would both save money and shorten the patient’s ED stay. Added benefit would accrue when a pediatric patient avoids a head CT by decreasing their risk for a subsequent cancer [12].
To enable this vision and further enhance our role toward cost savings will require emergency medicine researchers to complement validated CDRs with the creation, testing and validation of accurate and persuasive patient education tools, sufficient to dissuade most patients of their dogmatic and erroneous beliefs regarding radiographs. EPs have abolished incorrect dogmas before. For instance, consider the well-deserved death at the hands of academic EPs of the previous dogmatic belief that no abdominal pain patient can be administered an opiate until they have been examined by a surgeon [13]. Hopefully, patients’ dogmatic beliefs regarding radiographs can also become consigned to the dustbin of history.
Certain myths need to die
In re-branding ourselves, we should also work to abolish other dogmatic myths that plague us, by refuting certain misleading beliefs that cause the public to wrongly conclude that ED care is a larger source of health care expenditures than is the case.
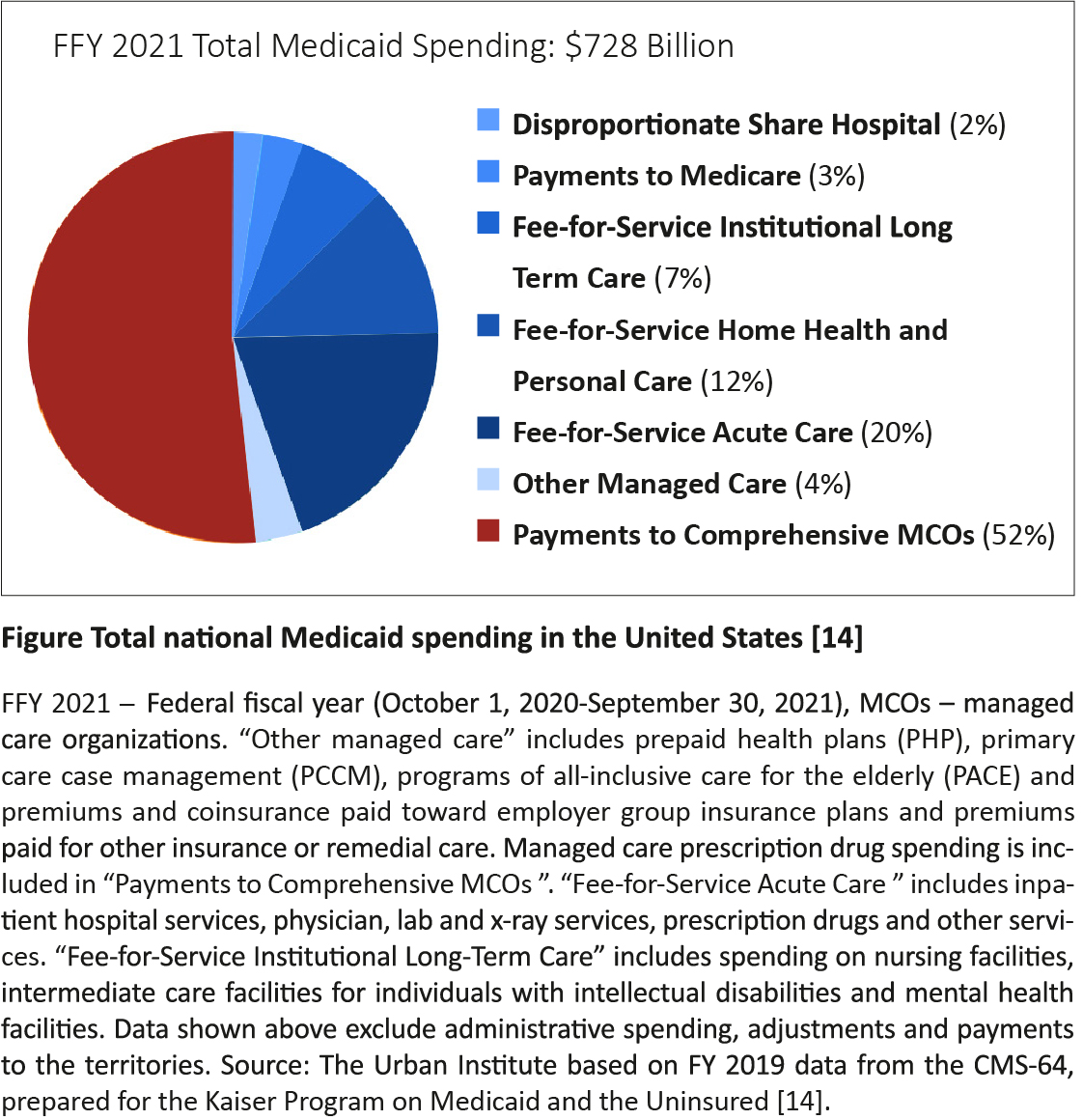
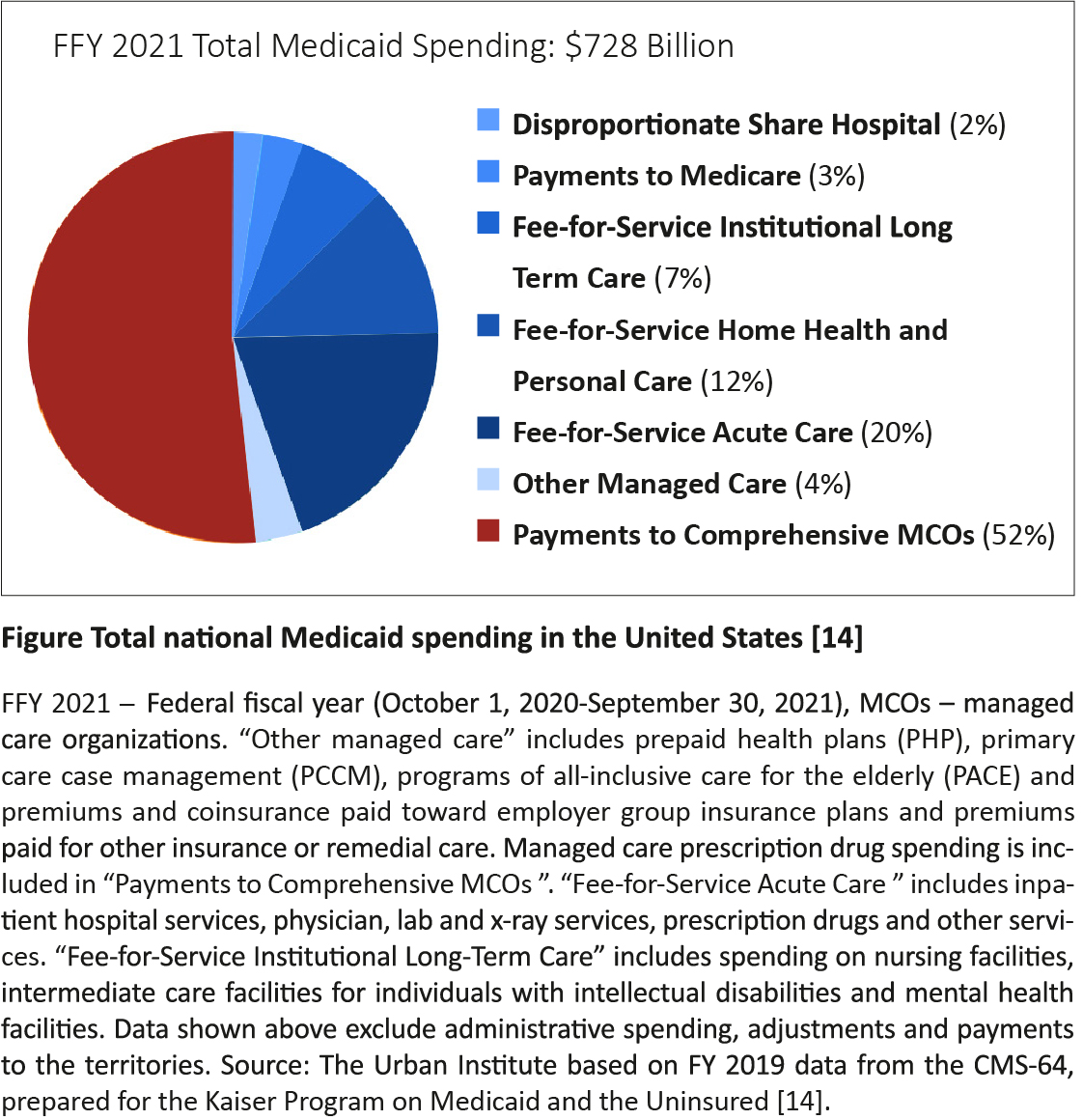
Consider the myth of Medicaid expenditures in the United States. Medicaid, contrary to popular belief, is not health insurance. It is a government welfare program. It provides a payment mechanism for low-income individuals to obtain health care, while shielding them from the costs and charges for that care. When I ask my friends and neighbors what percentage of a state’s Medicaid budget is spent for emergency department care of persons living in poverty, most of them estimate that number to be about 50%. In truth, 52% of Medicaid spending goes for managed care organizations (MCOs) and health plans, 20% pays for fee-for-service acute care and 19% is spent for long term care (e.g. “nursing homes”) [14]. The Figure parses the spending by MCOs. Spending for ED care is not large enough to merit its own “share” of that “pie”! [14]. I’d bet that a similar misconception about how much of the nation’s health care budget is spent for emergency department care exists in every voivodeship in Poland!
In the United States, patients who ideally would be receiving their medical care in an inpatient department often receive much of that care in an emergency department, when surges in patient demand occur. By pitching in and providing inpatient-type care to “boarders” in the emergency department, we help the hospital system avoid the considerable expense of expanding their inpatient capacity in such a manner that the hospital’s “percent occupancy” would fall, while enabling them to better accommodate occasional surges in demand for inpatient medical care.
The ”take-home message”
In summary, rather than repeatedly serving as the “whipping boy” in the “court of public opinion” for our provision of what is incorrectly perceived to be high-cost medical care, EPs should proudly call attention to the numerous ways by which EPs and EDs in which they work help save their nations and patients significant sums of money.
Hopefully, you are now convinced that as EPs, we deserve to be valued not only for being available 24 x 7 x 365, but also for the numerous cost savings that our training permits us to enable.
Brian Zink captured a wonderful initial “vision statement” for EM with the title of his book documenting the history of our specialty, “Anyone, Anything, Anytime”. That book was first published in 2006. However, in 2023, it is time to move beyond that title. We need a new “vision statement” to “re-brand” EM in a manner that captures how EPs help not only save lives, but also save significant sums of money, 24 x 7 x 365.
I offer for consideration: “Emergency Medicine: Saving not only lives, money, by delivering life-saving, life-enhancing evidence-based medical care quickly, efficiently and effectively”.
Emergency physicians should deservedly take pride in the numerous ways that they help save their nations’ money, via application of their tools and their training, as they accurately and expeditiously work up patients and implement therapy plans that were unthinkable when I entered my emergency medicine residency in 1986. As the citizens of your nation learn of this story, perhaps a few words of their words of praise could usefully offset the “burnout” that plagues many physicians of our specialty.
Now that you know the story that justifies the claim that emergency medicine should be “re-branded” as a cost-saving specialty, it is up to all of us to adopt and spread this message.
Conflicts of interest
None.
Funding
None.
References
| 1. |
Herness J, Buttolph A, Hammer NC. Acute pyelonephritis in adults: rapid evidence review. Am Fam Physician [Internet]. 2020;102(3):173-80. Available from: https://www.aafp.org/pubs/afp/issues/2020/0801/p173.html.
|
| 2. |
CDC sexually transmitted disease guidelines 2021. Pelvic Inflammatory Disease (PID) [Internet]. Centers for Disease Control and Prevention. 2021 [cited 2023 Sep 4]. Available from: https://www.cdc.gov/std/treatment-guidelines/pid.html.
|
| 3. |
Warfarin side effects: watch for interactions print [Internet]. Mayo Clinic. 2022 [cited 2023 Sep 4]. Available from: https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/in-depth/warfarin-side-effects/art-20047592.
|
| 4. |
Stubblefield WB, Kline JA. Outpatient treatment of emergency department patients diagnosed with venous thromboembolism. Postgrad Med [Internet]. 2021 Aug 6;133(sup1):11-9. Available from: https://www.tandfonline.com/doi/full/10.1080/00325481.2021.1916299.
|
| 5. |
Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain. J Am Coll Cardiol [Internet]. 2021 Nov;78(22):e187-285. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0735109721057958.
|
| 6. |
Shell IG. Decision rules for the use of radiography in acute ankle injuries. JAMA [Internet]. 1993 Mar 3;269(9):1127. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.1993.03500090063034.
|
| 7. |
Stiell IG. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA J Am Med Assoc [Internet]. 1996 Feb 28;275(8):611. Available from: http://jama.jamanetwork.com/article.aspxdoi=10.1001/jama.1996.03530320035031.
|
| 8. |
Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med [Internet]. 2000 Jul 13;343(2):94-9. Available from: http://www.nejm.org/doi/abs/10.1056/NEJM200007133430203.
|
| 9. |
Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, et al. The Canadian C-Spine Rule versus the NEXUS Low-Risk Criteria in Patients with Trauma. N Engl J Med [Internet]. 2003 Dec 25;349(26):2510-8. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa031375.
|
| 10. |
Schonfeld D, Bressan S, Da Dalt L, Henien MN, Winnett JA, Nigrovic LE. Pediatric Emergency Care Applied Research Network head injury clinical prediction rules are reliable in practice. Arch Dis Child [Internet]. 2014 May 1;99(5):427-31. Available from: https://adc.bmj.com/lookup/doi/10.1136/archdischild-2013-305004.
|
| 11. |
Stiell IG. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in Patients With Minor Head Injury. JAMA [Internet]. 2005 Sep 28;294(12):1511. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.294.12.1511.
|
| 12. |
Sheppard JP, Nguyen T, Alkhalid Y, Beckett JS, Salamon N, Yang I. Risk of brain tumor induction from pediatric head CT procedures: a systematic literature review. Brain Tumor Res Treat [Internet]. 2018;6(1):1. Available from: https://btrt.org/DOIx.php?id=10.14791/btrt.2018.6.e4.
|
| 13. |
Brewster GS, Herbert ME, Hoffman JR. Medical myth: analgesia should not be given to patients with an acute abdomen because it obscures the diagnosis. West J Med [Internet]. 2000 Mar;172(3):209-10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10734818.
|
| 14. |
Williams E, Rudowitz R, Burns A. Medicaid financing: the basics [Internet]. KFF. 2023. Available from: https://www.kff.org/medicaid/issue-brief/medicaid-financing-the-basics/.
|