Abstract
Postoperative nausea and vomiting (PONV) are significant clinical problems associated with patients’ unpleasant experiences and potential complications such as dehydration and electrolyte imbalances. In the search for effective methods of alleviating PONV, increasing attention is paid to the therapeutic properties of ginger. This review aims to summarize the current state of knowledge regarding the effect of ginger on reducing PONV. Analysis of conducted clinical studies suggests that ginger may be an effective agent in alleviating PONV after surgeries. Many of these studies indicate the beneficial effects of ginger, particularly when used in combination with conventional antiemetic drugs. Due to differences in methodology and inconclusive results in some studies, more research is needed to confirm these results and establish optimal doses and routes of administering ginger in clinical practice.
Citation
Gniado W, Mądry D S, Krych G, Rusak A, Oklińska J, Skóra M, Jadczak K, Kazimierski B. Ginger as a non-pharmacological prevention of postoperative nausea and vomiting (PONV): a review. Eur J Transl Clin Med. 2024;7(2):92-99Introduction
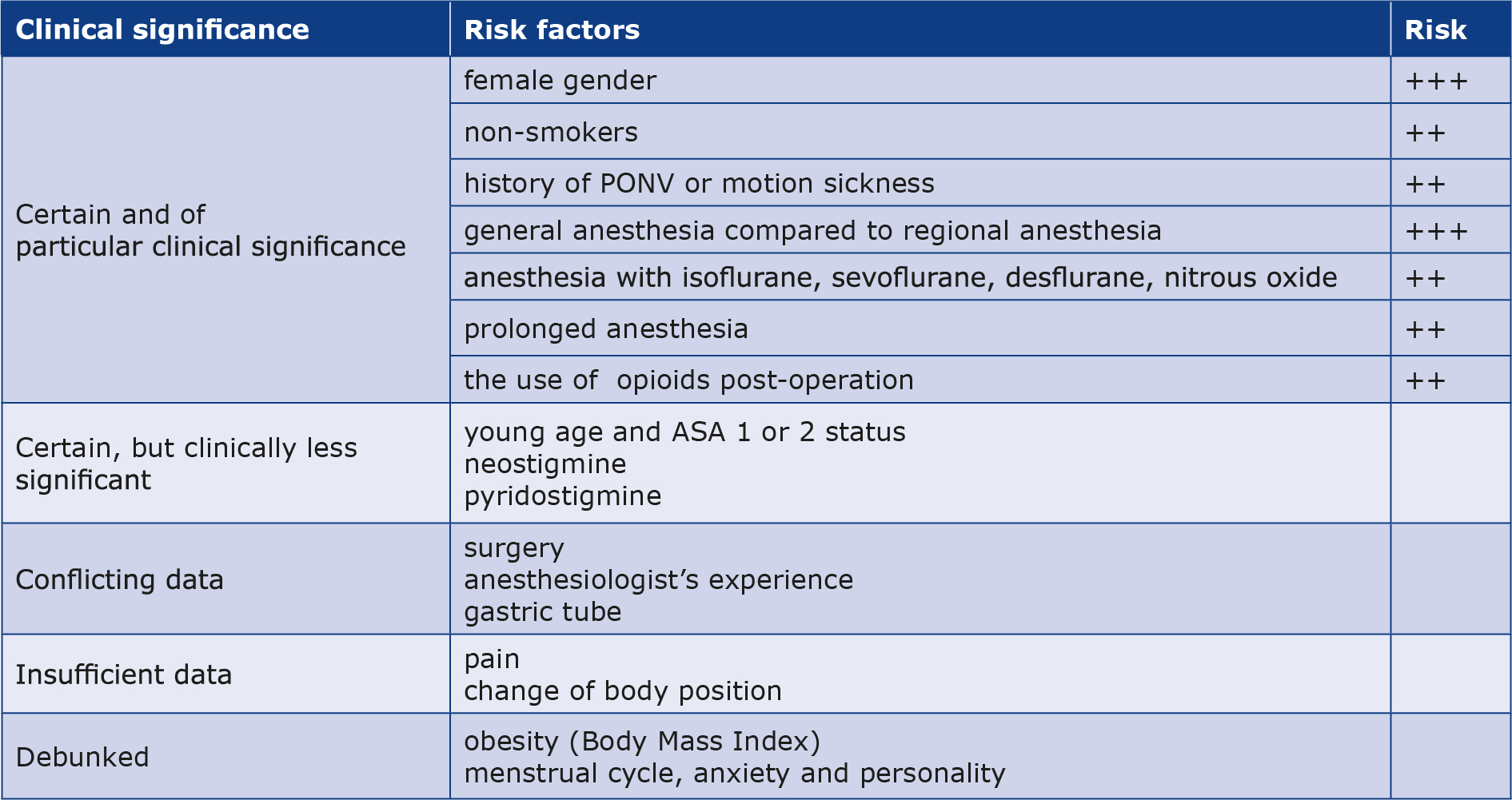
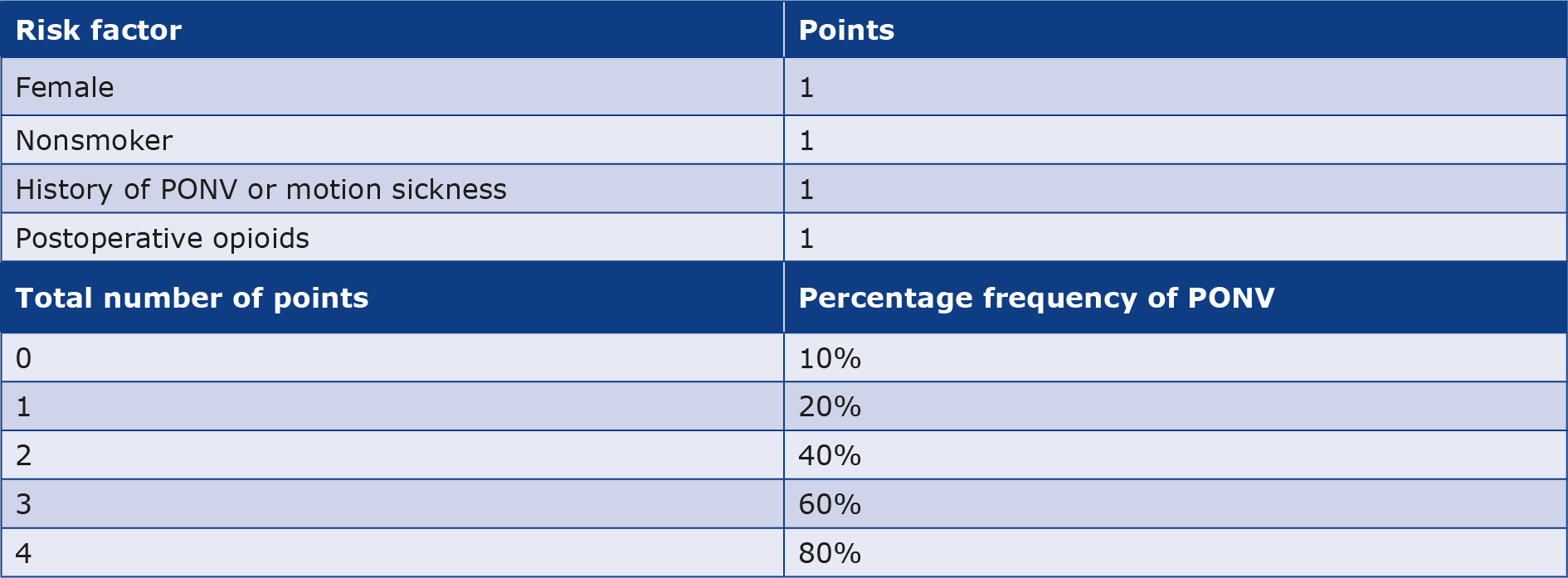
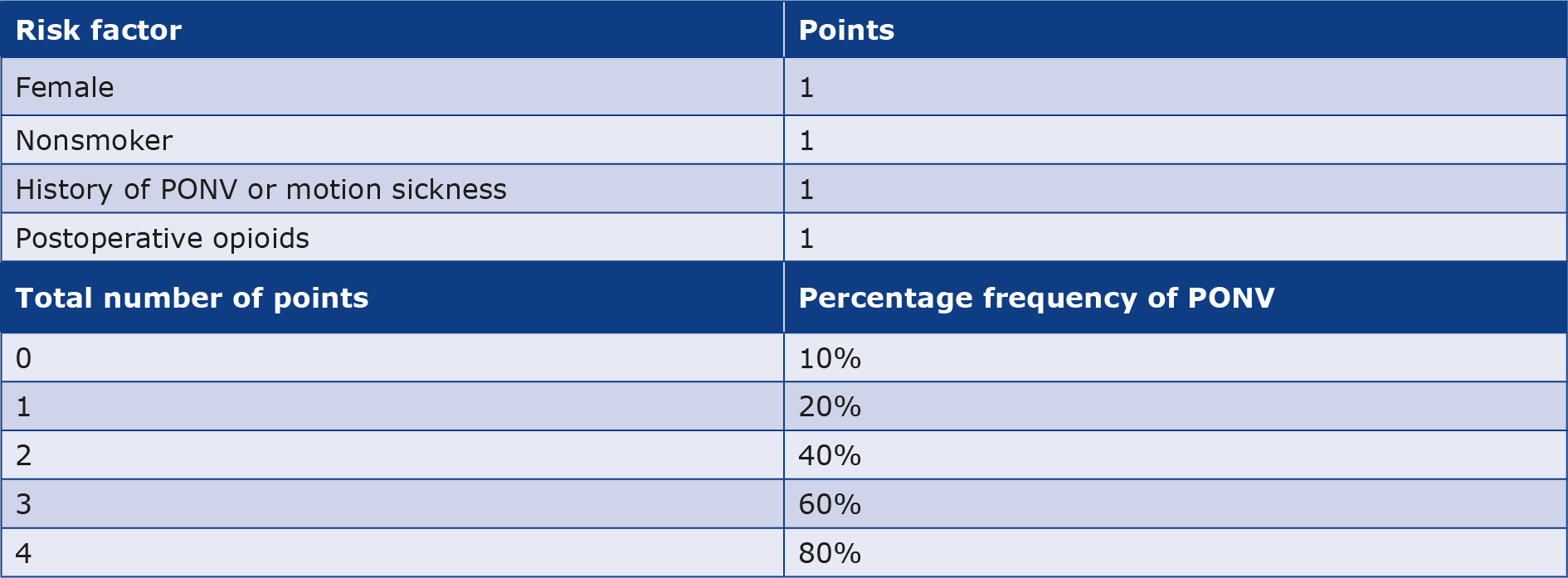
Postoperative nausea and vomiting (PONV) is a clinically significant complication that manifests within the first 24 hours post-surgery performed under general anesthesia and can last for more than 3 days. While considered an adverse effect of general anesthesia and a complication of surgical procedures, the exact causes of PONV are still not fully understood. It is known that the frequency of PONV is influenced not only by general anesthesia itself, but also by comprehensive perioperative patient care and various risk factors. PONV risk factors include female gender, history of motion sickness, history of PONV, non-smoking, prolonged anesthesia and the post-operative use of opioids [1]. PONV can occur in 20-30% of patients after surgeries [1-3]. The type of procedure also influences the frequency of PONV, e.g. after laparoscopic surgery it varies between 40% and 70% of patients [2, 4-5]. The use of volatile anesthetics during anesthesia and patient’s age (< 50 years) can also increase PONV frequency. Apfel classified risk factors according to their association with the severity of PONV frequency (Table 1) and estimated the risk of PONV occurrence in patients with specific risk factors (Table 2) [6]. Although it can be helpful, the Apfel scale does not include many other PONV risk factors. Due to the complexity of the issue, anesthesiologists are unable to predict the occurence of PONV in any patient group. Nevertheless, the role of medical staff should not be underestimated because consideration of risk factors during selection of anesthetic drugs can reduce PONV episodes [6].
Table 1. PONV risk factors classified based on EbM and clinical significance (Apfel scale) [6]
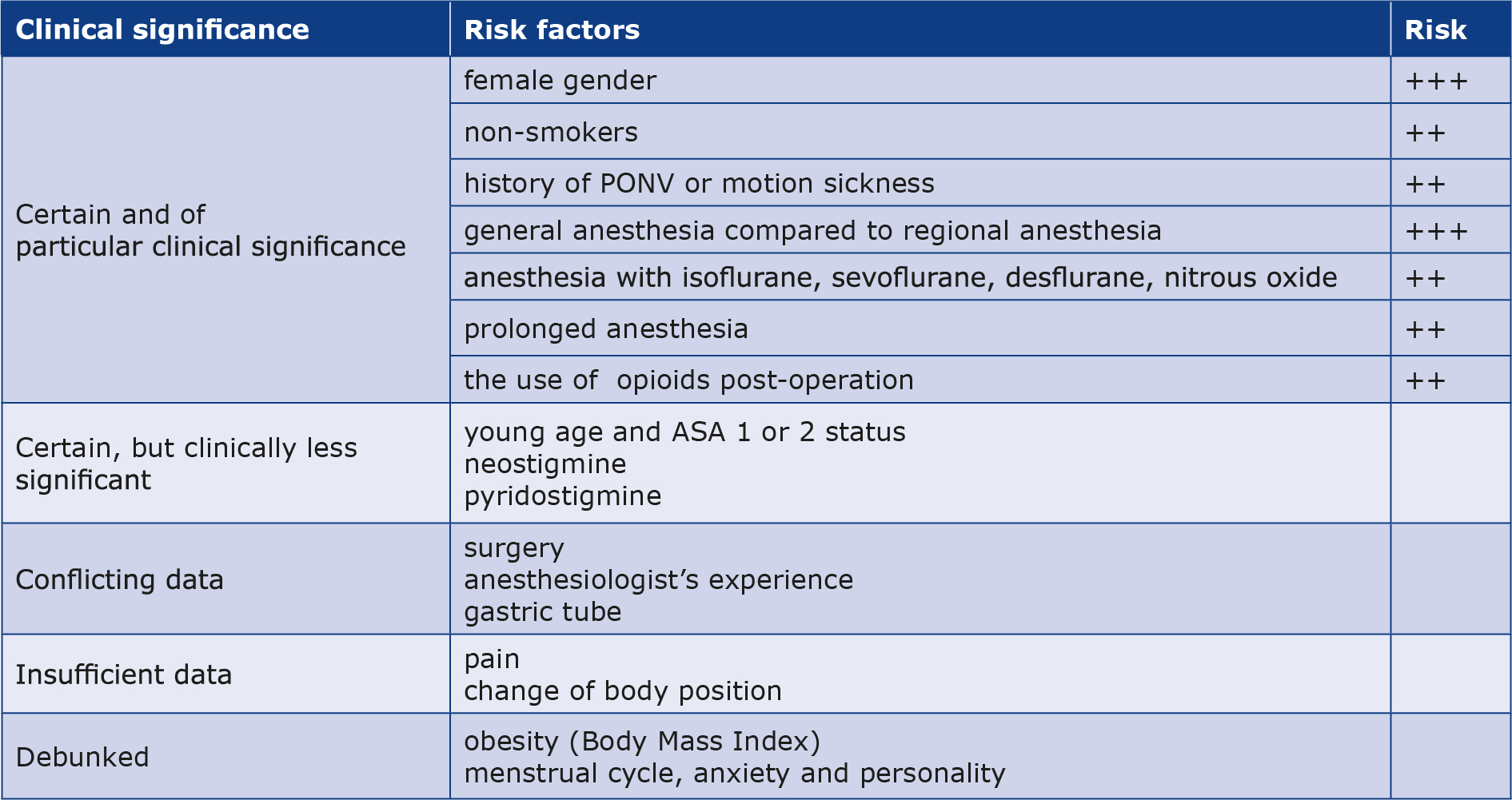
Table 2. Simplified PONV risk scale [6]
The consequences of PONV include dehydration, electrolyte imbalance, cardiac arrhythmias, bleeding, hematomas, delayed wound healing, wound dehiscence, gastric content aspiration, esophageal rupture, subcutaneous emphysema or bilateral pneumothorax [1]. These complications reduce patients’ quality of life, delay recovery and prolong the hospital stay [1-2]. Delayed hospital discharge also generates additional duties for medical staff and increases healthcare costs. Additionally, it was been estimated that PONV prolongs the stay in the post-anesthesia care unit by approximately 25 minutes [1].
Materials and methods
This review was based on literature available online in the PubMed database. Emphasis was placed on articles written in English and published from the year 2000 onward. The literature was selected to provide the broadest perspective on the topic and draw consistent conclusions. We used keywords “ginger”, “PONV”, “postoperative nausea and vomiting”, “general anesthesia” and “antiemetic drugs”.
Results and discussion
We found 66 studies and excluded 35 for the following reasons: lack of full text (n = 1), unrelated topic (n = 22), not in English language (n = 2), lack of placebo group (n = 4), summary of a study already included in our review (n = 2), published before 2000 (n = 4). Following the initial search, we selected 31 studies that met our criteria.
Are antiemetic drugs the best option we can offer?
The most common methods to reduce the risk of PONV include regional anesthesia, the use of propofol, and antiemetic drugs e.g. 5-HT3 receptor antagonists, antihistamines, antiparkinsonian drugs, anticholinergic drugs, promethazine and butyrophenones [2-3, 7]. To increase the effectiveness of therapy it is common clinical practice to combine antiemetic drugs that have different mechanisms of action [7]. Unfortunately, the above-mentioned drugs are associated with adverse effects e.g. excessive drowsiness, hypotension, dry mouth, dysphoria, hallucinations and extrapyramidal symptoms (e.g. dystonia, akathisia) [3]. Additionally, metoclopramide may cause headaches and diarrhea, while ondansetron may lead to transient elevation of liver transaminases [2]. Another disadvantage of synthetic antiemetic drugs is the necessity to use additional medications to alleviate adverse effects, leading to prolonged hospital stays and increased costs of care [4]. 5-HT3 antagonists (e.g. ondansetron) are most commonly used as prophylaxis on account of their higher efficacy in reducing the frequency of PONV compared to traditional antiemetic drugs like droperidol or metoclopramide. Due to numerous adverse effects the routine use of antiemetic drugs is not recommended, particularly in patients without PONV risk factors [7]. Additionally, the use of 5-HT3 antagonists is associated with higher treatment costs, prompting the search for relatively cheaper, widely available solutions with minimal adverse effects and drug interactions. Therefore, there is growing interest in herbal medicines and non-pharmacological methods [4].
Biological properties of ginger Ginger
(Zingiber officinale) has been used in Chinese and Iranian medicine for over 2000 years. Its unique properties allow for various applications, including the alleviation of gastrointestinal discomfort (primarily nausea and vomiting) as well as of symptoms caused by motion sickness, chemotherapy or gynecological interventions [3, 8-9]. One study has shown that compounds found in ginger root have antioxidant effects on free radicals that cause vomiting [4]. Additionally, ginger exhibits antagonistic effects on cholinergic (M3) and serotonergic (5-HT3 and 5-HT4) receptors, which is important in preventing PONV [10]. The main antiemetic substances found in ginger are gingerols and shogaols. Experimental studies revealed that 6-shogaol, 6-gingerol and zingerone inhibit the vomiting-inducing signal pathway in the afferent neurons of the vagus nerve through the suppression of 5-HT receptors, with 6-shogaol being the most potent inhibitor. The relative proportions of gingerols and shogaols are also important for ginger’s effectiveness [11]. 8-gingerol is a 5-HT3 receptor antagonist in the ileum and 6-gingerol has been shown to enhance gastrointestinal transport [7]. Another mechanism includes the action of 6-, 8-, and 10-gingerols and 6-shogaol on the 5-HT3 receptor ion channel complex by binding to its modulatory site [9]. Galanolactone exhibits antiemetic effects through competitive antagonistic action on 5-HT3 receptors in the ileum [2, 7]. Besides its proven biological effects, it is important to emphasize that ginger is relatively inexpensive, widely available and its use is not associated with adverse effects [4, 7, 11].
Oral ginger
Montazeri et al. investigated the impact of ginger on PONV intensity. Authors divided patients randomly into an experimental group (received 4 capsules containing 250 mg of ginger 1 hour before surgery) and a control group (received 4 placebo capsules 1 hour before surgery). They reported that the frequency of nausea in the experimental group was lower at 2 and 6 hours post-operation compared to the placebo group [12]. However, the difference at 2 hours post-operation was only slightly significant (p = 0.05). There were no distinct differences between both groups in the intensity of vomiting at any time point.
Albooghobeish et al. demonstrated the difference in the presence of PONV (p = 0.001) between two groups after laparoscopic cholecystectomy [4]. The intervention group received two 500 mg and one 250 mg capsules containing dried Ginger rhizome extract and the control group received 3 placebo capsules. The mean severity of nausea (measured using the Visual Analog Scale) in the intervention group changed from 7.92 ± 1.28 to 0.33 ± 0.67, while in the control group they changed from 8.00 ± 1.20 to 2.11 ± 1.55. Additionally, patients in the group receiving ginger capsules vomited less frequently and the use of antiemetic drugs was significantly lower than in the placebo group (p = 0.001).
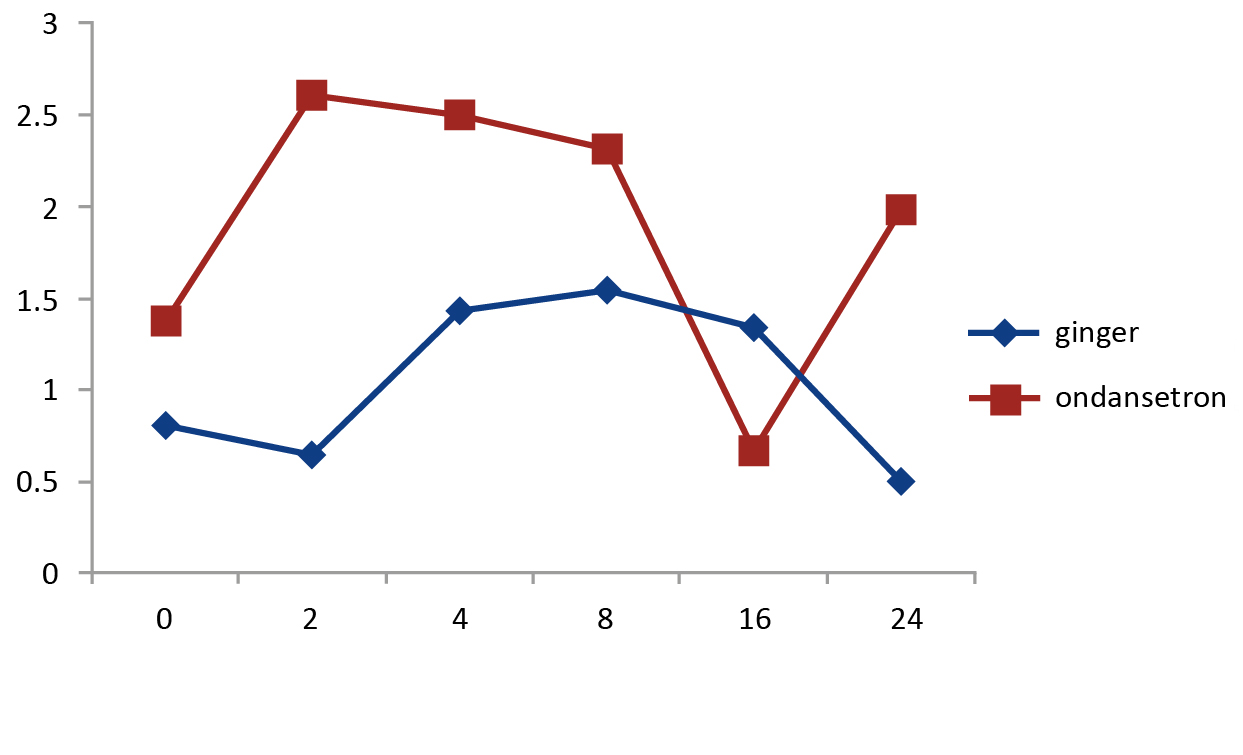
Soltani et al. investigated nausea intensity and vomiting frequency at 0, 4, 8, 16 and 24 hours after laparoscopic cholecystectomy [10]. One group of patients received 500 mg of ginger orally 1 hour before surgery, while another group received 4 mg of ondansetron i.v. before the operation ended. Nausea intensity was significantly lower in the ginger group (except at 16 hours post-operation, Figure 1). However, the vomiting frequency did not differ between the groups.
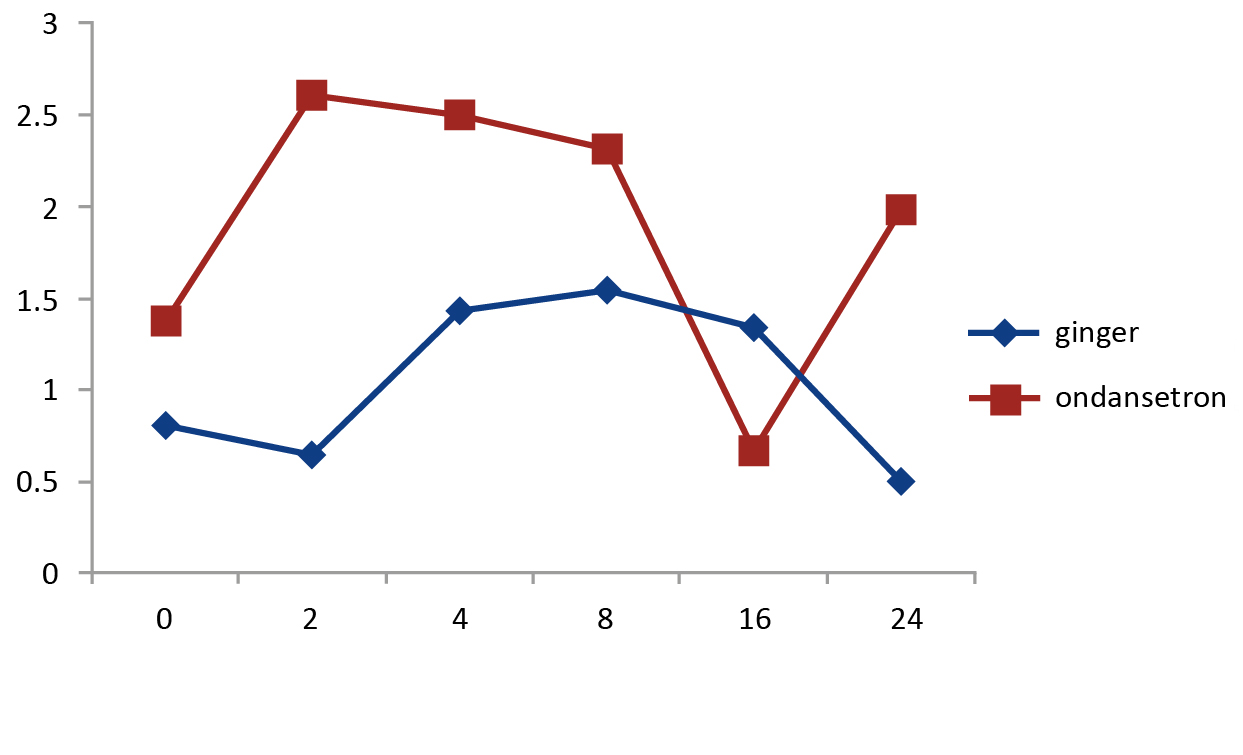
Figure 1. The differences in nausea severity between the groups studied by Soltani et al. [10]
Vertical axis – nausea severity measured using the Visual Analogue Scale (average scores); horizontal axis – hours after surgery
Bameshki et al. demonstrated that oral ginger is effective in decreasing the severity of PONV after laparoscopic cholecystectomy [13]. One hour before surgery, the intervention group received 2 capsules containing 250 mg of ginger, while the control group received 2 placebo capsules. The severity of nausea distinctly changed in both groups (p = 0.001), however was lower in the ginger group (p = 0.078), with statistically relevant differences at 2 hours (p = 0.034) and 12 hours (p = 0.043). Although the incidence of vomiting was higher in the placebo group at 2 and 12 hours post-surgery, the number of vomiting episodes was statistically almost equal between both groups (p > 0.05).
Sedigh et al. investigated the effectiveness of ginger in preventing PONV after eye surgery [14]. The severity of nausea was lower in Group A (received 1 g of ginger 1 hour before the procedure) compared to Group B (received a placebo one hour before the procedure) immediately after recovery from anesthesia, as well as 15 minutes, 30 minutes and 2 hours after recovery (p < 0.05). Additionally, the incidence of vomiting also was significantly lower in the ginger group B (p < 0.05).
Beiranvand et al. administered ginger to reduce PONV among patients undergoing upper and lower limb surgery [15]. The intervention group received 4 ginger capsules 250 mg each, while the control group received 4 placebo capsules 2 hours before surgery. The intervention group had significantly lower incidence and severity of PONV at various time points after surgery compared to the placebo group (p < 0.05).
Sihombing et al. demonstrated that although adding ginger extract to beverages during the perioperative period significantly reduced the frequency of postoperative nausea (PON), it did not influence the frequency of postoperative vomiting [11]. Hewitt and Watts compared 6 trials measuring the effectiveness of varying doses of ginger powder in reducing PONV [5]. Evidence supporting the efficacy of 1-1.5 g doses is limited. Additionally, they suggested that there is no strong evidence supporting the use of either lower (< 1 g) or higher (> 1.5 g) doses of ginger powder. The authors noted that analysed studies had methodological flaws, thus their findings should be interpreted cautiously.
Aromatherapy with ginger oil
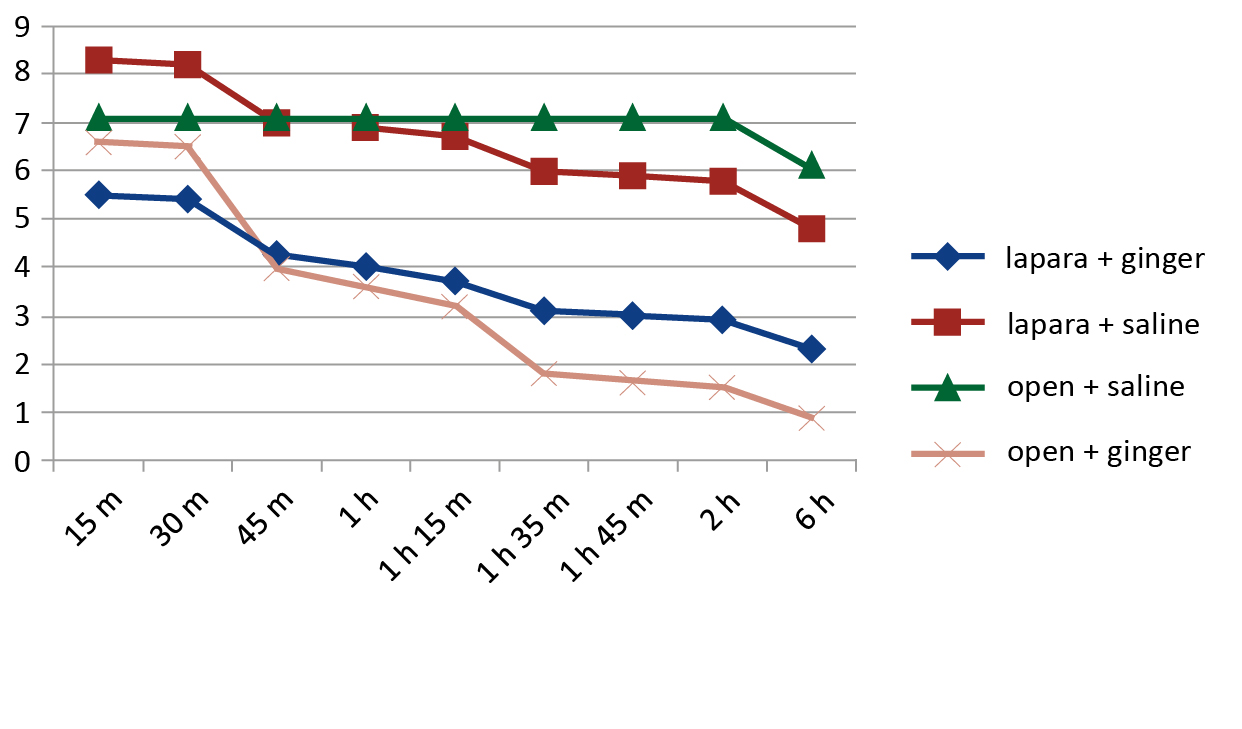
Hosseini and Adib-Hajbaghery [2] showed that the severity of nausea highly depends on the type of surgery and the presence of antiemetic intervention (p < 0.001). Authors compared open versus laparoscopic nephrectomy and also ginger essence versus placebo. Patients were divided into 4 groups (open surgery + ginger essence; laparoscopy + ginger essence; open surgery + placebo; laparoscopy + placebo), with two groups receiving ginger essence (two drops of ginger essence applied on gauze attached to the patients’ collars) reapplied every 30 minutes for two subsequent hours. The mean nausea severity was reduced in both groups receiving ginger essence versus groups with placebo, but also ginger essence showed higher effectiveness in patients after open nephrectomy than laparoscopic. The vomiting episodes were 2.92 ± 0.70 (open nephrectomy + placebo) versus 0.16 ± 0.37 (open nephrectomy + ginger essence). Additionally, the vomiting episodes were 6.0 ± 1.33 (laparoscopic nephrectomy + placebo) versus 1.39 ± 0.78 (laparoscopic nephrectomy + ginger essence) (Figure 2).
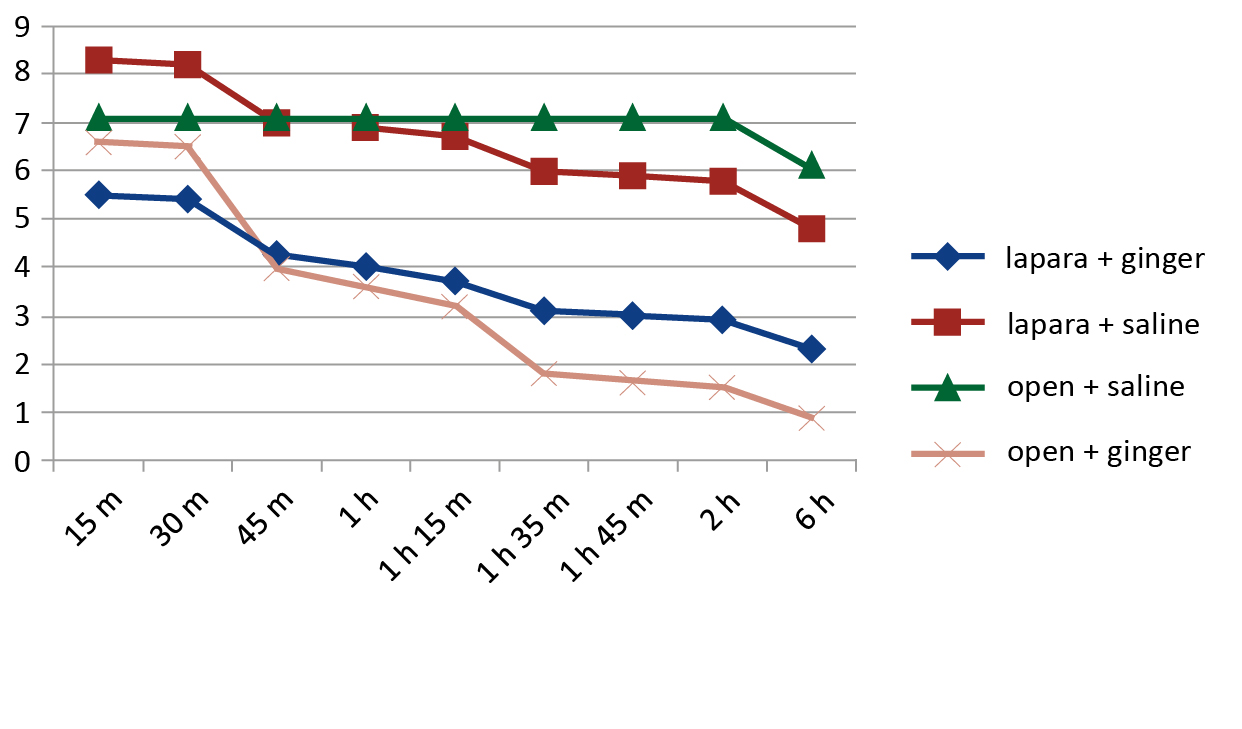
Figure 2. Changes in nausea mean scores in the groups studied by Hosseini et al. [2]
Vertical axis – nausea mean scores, horizontal axis – hours after surgery
Adib-Hajbaghery and Hosseini [16] demonstrated that inhaling ginger essence has a positive effect on PONV after nephrectomy. The mean nausea intensity in the treatment group at the four subsequent time points was distinctly lower than in the control group (p < 0.001). Additionally, the differences regarding the number of vomiting episodes experienced by the treatment and control groups were statistically significant (p < 0.001). Sforza et al. [17] used ginger oil to treat nausea and vomiting after breast augmentation surgery. Participants received three drops of ginger oil (110 mg Z. officinale) or 3 drops of a placebo oil placed on their laryngeal mask before insertion in the larynx. The results showed that using ginger oil had a significant influence on PONV (F(1, 18) = 73.05, p < 0.001). The mean PONV score was 1.70 ± 0.48 and 4.20 ± 0.79 and the mean VAS score was 5.0 ± 1.63 and 5.9 ± 2.33 for the experimental group and control group, respectively. In their systematic review.
Arslan and Çelik compared the effectiveness of ginger aromatherapy versus placebo in PONV prevention. One study revealed that an oil mixture (containing ginger essential oil) and pure ginger oil reduced antiemetic consumption and the frequency of PONV [1]. Additionally, they reported that 7 out of 8 studies confirmed the antiemetic properties of orally administered ginger, while in 1 study no significant difference was found. In a study by Lee and Shin the experimental group received 0.3 ml of pure ginger essential oil inhalation after abdominal surgery, while the control group received a saline inhalation [18]. Nausea and vomiting scores were significantly lower in the experimental group. Additionally, the nausea and vomiting scores decreased distinctly in the first 6 hours after ginger essential oil inhalation.
Karaman et al. found a statistically significant difference in the nausea scores at 15 minutes (p = 0.00), with 2 drops of ginger and lavender essential oils outperforming rose oil and pure water [19]. Marsh et al. administered a custom blend of essential oils (including ginger) to the intervention group, which exhibited a statistically significant decrease in the need for antiemetics (by 22%; p = 0.05) [20]. Additionally, the total doses of antiemetics administered during the study period were significantly diminished (21%; p ≤ 0.05).
Kiberd et al. reported that a blend of ginger, lavender, mint and spearmint aromatherapy had a non-significant effect on PONV in children compared with the control group [21]. However, the authors acknowledged that their pilot study had methodological flaws, which should be addressed.
Ginger combined with other drugs
Mandal et al. reported that the ginger-ondansetron combination (2 capsules with 0.5 mg ginger powder + 4 mg ondansetron i.v.) was significantly more effective than ondansetron alone (2 placebo capsules + 4 mg ondansetron i.v.) in preventing PONV [3]. Tavlan et al. concluded that a ginger-dexamethasone combination was not more effective than dexamethasone alone in preventing PONV among patients undergoing thyroidectomy [7].
Gynecological surgeries
Eberhart et al. found no notable differences between the 1st ginger group (300 mg of ginger powder), the 2nd ginger group (600 mg of ginger powder) and placebo group in terms of nausea, vomiting or the need for antiemetic medication following gynecological laparoscopy [22]. Apariman et al. administered 3 capsules of ginger to patients 1 hour prior to gynecological laparoscopy, while the control group B received 3 capsules of placebo. Ginger was effective in preventing nausea and it reduced vomiting within 6 hours post- -operation (close to statistical significance) [23]. The effect of ginger powder on PONV was measured following major open gynecologic surgery and gynecological laparoscopy [24-25]. The authors observed statistically significant differences in nausea between both the ginger (1 g of ginger powder) and placebo groups. Nausea incidents and intensity were reduced in the ginger group. Additionally, the incidence and frequency of vomiting were lower in the ginger group, although the authors noted that these differences were not statistically significant [25].
Meta-analyses
In their systematic review and meta-analysis, Wang et al. reported that aromatherapy decreased the intensity of PON (standardized mean difference (SMD): -0.93, 95% CI: -1.64 to -0.22; p = 0.010) [26]. However, the reduction in episodes of vomiting was not statistically significant (SMD: -0.81, 95% CI: -1.98 to 0.37; p = 0.180). Although the subgroup analysis confirmed the effectiveness of ginger essence in PON management, due to considerable statistical heterogeneity and potential biases within studies, these findings should be interpreted cautiously. Arruda et al. explored the role of herbal medications, including ginger, in reducing PONV after laparoscopic or open obstetric/gynecological surgeries [27]. They reported a statistically distinct reduction in vomiting (relative risk [RR] 0.57; 95% confidence interval [CI] 0.38 to 0.86) and nausea (RR 0.69; 95% CI 0.50 to 0.96) with ginger compared to placebo. Additionally, the results suggested a statistically not significant reduction in the need for rescue pain medication in the ginger group compared to placebo.
According to Griffiths et al. it is doubtful whether ginger has any influence on the number of women experiencing intraoperative nausea during cesarean section under regional anesthesia [28]. Lu et al. reported that ginger reduces PON but does not cause any statistically significant difference in postoperative vomiting, combined rate of PONV and antiemetic drug use [28]. Therefore, the authors concluded that well-designed and rigorously conducted trials are needed to confirm the association between ginger intake and the risk of PONV.
Zhao et al. demonstrated that both ginger powder and ginger oil supplementation were effective in reducing the use of antiemetics and the intensity of nausea [29]. Ginger oil was superior to other forms of ginger treatment for the prophylaxis of postoperative vomiting (POV). Despite reducing the intensity of PON, ginger preparations did not show any obvious advantages in reducing the frequency of PON incidents.
Tóth et al. reported that ginger had a significant effect on reducing the severity of PONV (p = 0.019) and the results suggest that ginger reduces both the incidence of PONV and the demand for antiemetic medications [30]. Zhu et al. reported that ginger significantly outperformed placebo in terms of nausea severity, the percentage of rescue antiemetic use and the incidence of nausea and vomiting during the 6-hour postoperative period (for nausea severity: RR = 0.68, 95% CI = 0.55-0.85, p < 0.001; for rescue antiemetic use: RR = 0.78, 95% CI = 0.42-1.44, p = 0.43) [31]. The ginger group had a significantly decreased incidence of nausea in comparison to the preventive antiemetic group. Neither the frequency of vomiting nor the percentage of rescue antiemetic drug usage showed any appreciable variations.
Chaiyakunapruk et al. concluded that a fixed dose of > 1 g of ginger powder is more effective than placebo in preventing PONV [32].
Conclusions
Not all published studies confirm the effectiveness of ginger in reducing PONV. Further clinical research is needed to validate ginger’s effectiveness, establish its optimal dose and route, and to develop precise recommendations for its use in clinical practice.
Conflict of interest
None.
Funding
None.
---------------
Image – pexels.com
References
| 1. |
Arslan HN, Çelik SŞ. Nonpharmacological Nursing Interventions in Postoperative Nausea and Vomiting: A Systematic Review. J PeriAnesthesia Nurs [Internet]. 2024;39(1):142–54. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1089947223008663.
|
| 2. |
Hosseini FS, Adib-Hajbaghery M. Ginger Essence Effect on Nausea and Vomiting After Open and Laparoscopic Nephrectomies. Nurs Midwifery Stud [Internet]. 2015;4(2). Available from: http://www.nmsjournal.com/?page=article&article_id=28625.
|
| 3. |
Mandal P, Das A, Majumdar S, Bhattacharyya T, Mitra T, Kundu R. The efficacy of ginger added to ondansetron for preventing postoperative nausea and vomiting in ambulatory surgery. Pharmacognosy Res [Internet]. 2014;6(1):52–7. Available from: http://www.phcogres.com/text.asp?2014/6/1/52/122918.
|
| 4. |
Alboghobeish M, Ghomeishi A, Adarvishi S, Neisi A, Mahmoodi K, Asadi M, et al. The Effect of Preoperative Zintoma Capsule on Postoperative Nausea and Vomiting After Laparoscopic Cholecystectomy. Anesthesiol Pain Med [Internet]. 2018;In Press(In Press). Available from: https://brieflands.com/articles/aapm-67132.html.
|
| 5. |
Hewitt V, Watts R. The effectiveness of non-invasive complementary therapies in reducing postoperative nausea and vomiting following abdominal laparoscopic surgery in women: a systematic review. JBI Database Syst Rev Implement Reports [Internet]. 2009;7(19):850–907. Available from: http://journals.lww.com/01938924-200907190-00001.
|
| 6. |
Apfel CC, Läärä E, Koivuranta M, Greim C-A, Roewer N. A Simplified Risk Score for Predicting Postoperative Nausea and Vomiting. Anesthesiology [Internet]. 1999;91(3):693–693. Available from: https://pubs.asahq.org/anesthesiology/article/91/3/693/37359/A-Simplified-Risk-Score-for-Predicting.
|
| 7. |
Tavlan A, Tuncer S, Erol A, Reisli R, Aysolmaz G, Otelcioglu S. Prevention of Postoperative Nausea and Vomiting after Thyroidectomy. Clin Drug Investig [Internet]. 2006;26(4):209–14. Available from: http://link.springer.com/10.2165/00044011-200626040-00005.
|
| 8. |
Mamaril ME, Windle PE, Burkard JF. Prevention and Management of Postoperative Nausea and Vomiting: A Look at Complementary Techniques. J PeriAnesthesia Nurs [Internet]. 2006;21(6):404–10. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1089947206004345.
|
| 9. |
Taha A, Ashour HK, Reffat M, Elkhawaga OY. The impact of ginger and curcumin on diabetic nephropathy induced by streptozotocin in rats. Eur J Transl Clin Med [Internet]. 2023;6(2):51–65. Available from: https://ejtcm.gumed.edu.pl/articles/172884.
|
| 10. |
Soltani E, Jangjoo A, Afzal Aghaei M, Dalili A. Effects of preoperative administration of ginger (Zingiber officinale Roscoe) on postoperative nausea and vomiting after laparoscopic cholecystectomy. J Tradit Complement Med [Internet]. 2018;8(3):387–90. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2225411017300706.
|
| 11. |
Sihombing AT, Prabharani D, Lukman K, Sudjud RW. The effectiveness of ginger extract addition in calorified drinks during perioperative period to nausea severity, vomitus, post-operative anxiety, and metabolic disorder: A randomized control trial. Ann Med Surg [Internet]. 2022;84. Available from: https://journals.lww.com/10.1016/j.amsu.2022.104865.
|
| 12. |
Montazeri AS, Hamidzadeh A, Raei M, Mohammadiun M, Montazeri AS, Mirshahi R, et al. Evaluation of Oral Ginger Efficacy against Postoperative Nausea and Vomiting: A Randomized, Double - Blinded Clinical Trial. Iran Red Crescent Med J [Internet]. 2013;15(12). Available from: https://archive.ircmj.com/article/15/12/56141-pdf.pdf.
|
| 13. |
Bameshki A, Namaiee MH, Jangjoo A, Dadgarmoghaddam M, Eshaghi Ghalibaf MH, Ghorbanzadeh A, et al. Effect of oral ginger on prevention of nausea and vomiting after laparoscopic cholecystectomy: a double-blind, randomized, placebo-controlled trial. Electron Physician [Internet]. 2018;10(2):6354–62. Available from: http://www.ephysician.ir/index.php/browse-issues/10/2/964-6354.
|
| 14. |
Sedigh Maroufi S, Moradimajd P, Moosavi SAA, Imani F, Samaee H, Oguz M. Dose Ginger Have Preventative Effects on PONV-Related Eye Surgery? A Clinical Trial. Anesthesiol Pain Med [Internet]. 2019;9(5). Available from: https://brieflands.com/articles/aapm-92072.html.
|
| 15. |
Beiranvand S, Alvani M, Sorori M masud. The Effect of Ginger on Postoperative Nausea and Vomiting Among Patients Undergoing Upper and Lower Limb Surgery: A Randomized Controlled Trial. J PeriAnesthesia Nurs [Internet]. 2022;37(3):365–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1089947221001271.
|
| 16. |
Adib-Hajbaghery M, Hosseini FS. Investigating the effects of inhaling ginger essence on post-nephrectomy nausea and vomiting. Complement Ther Med [Internet]. 2015;23(6):827–31. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0965229915300108.
|
| 17. |
Sforza M, Sidhu M, Okhiria R, Okhiria T, Saghir R, Saghir N, et al. Using Ginger Oil to Treat Nausea and Vomiting Following Breast Augmentation Surgery. Plast Aesthetic Nurs [Internet]. 2023;43(4):225–30. Available from: https://journals.lww.com/10.1097/PSN.0000000000000534.
|
| 18. |
Lee YR, Shin HS. Effectiveness of Ginger Essential Oil on Postoperative Nausea and Vomiting in Abdominal Surgery Patients. J Altern Complement Med [Internet]. 2017;23(3):196–200. Available from: http://www.liebertpub.com/doi/10.1089/acm.2015.0328.
|
| 19. |
Karaman S, Karaman T, Tapar H, Dogru S, Suren M. A randomized placebo-controlled study of aromatherapy for the treatment of postoperative nausea and vomiting. Complement Ther Med [Internet]. 2019;42:417–21. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0965229918312330.
|
| 20. |
Marsh E, Millette D, Wolfe A. Complementary Intervention in Postoperative Care: Aromatherapy’s Role in Decreasing Postoperative Nausea and Vomiting. J Holist Nurs [Internet]. 2022;40(4):351–8. Available from: https://journals.sagepub.com/doi/10.1177/08980101211065555.
|
| 21. |
Kiberd MB, Clarke SK, Chorney J, D’Eon B, Wright S. Aromatherapy for the treatment of PONV in children: a pilot RCT. BMC Complement Altern Med [Internet]. 2016;16(1):450. Available from: http://journals.lww.com/01938924-200907190-00001.
|
| 22. |
Eberhart LHJ, Mayer R, Betz O, Tsolakidis S, Hilpert W, Morin AM, et al. Ginger Does Not Prevent Postoperative Nausea and Vomiting After Laparoscopic Surgery. Anesth Analg [Internet]. 2003;995–8. Available from: http://journals.lww.com/00000539-200304000-00016.
|
| 23. |
Apariman S, Ratchanon S, Wiriyasirivej B. Effectiveness of ginger for prevention of nausea and vomiting after gynecological laparoscopy. Journal-Medical Assoc Thail. 2006;89(12):2003.
|
| 24. |
Nanthakomon T, Pongrojpaw D. The efficacy of ginger in prevention of postoperative nausea and vomiting after major gynecologic surgery. J Med Assoc Thai [Internet]. 2006;89(Suppl 4):S130-6. Available from: https://www.thaiscience.info/journals/Article/JMAT/10401687.pdf.
|
| 25. |
Pongrojpaw D, Chiamchanya C. The efficacy of ginger in prevention of post-operative nausea and vomiting after outpatient gynecological laparoscopy. J Med Assoc Thai [Internet]. 2003;86(3):244–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12757064.
|
| 26. |
Wang J-Y, Huang H-Y, Chu W-O, Peng T-R, Lee M-C, Chen S-M, et al. Aromatherapy for the prevention of postoperative nausea and vomiting: A systematic review and meta-analysis. Tzu Chi Med J [Internet]. 2024;36(3):330–9. Available from: https://journals.lww.com/10.4103/tcmj.tcmj_240_23.
|
| 27. |
Arruda APN, Zhang Y, Gomaa H, Bergamaschi C de C, Guimaraes CC, Righesso LAR, et al. Herbal medications for anxiety, depression, pain, nausea and vomiting related to preoperative surgical patients: a systematic review and meta-analysis of randomised controlled trials. BMJ Open [Internet]. 2019;9(5):e023729. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2018-023729.
|
| 28. |
Lu C, Chen X, Yan X, He J, Nie Z. The preventive and relieving effects of ginger on postoperative nausea and vomiting: A systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud [Internet]. 2022;125:104094. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0020748921002418.
|
| 29. |
Zhao C, Chen W, Wang D, Cong X, Zhu M, Zhu C, et al. Ginger (Zingiber officinale Roscoe) preparations for prophylaxis of postoperative nausea and vomiting: A Bayesian network meta-analysis. J Ethnopharmacol [Internet]. 2023;317:116791. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0378874123006591.
|
| 30. |
Tóth B, Lantos T, Hegyi P, Viola R, Vasas A, Benkő R, et al. Ginger (Zingiber officinale): An alternative for the prevention of postoperative nausea and vomiting. A meta-analysis. Phytomedicine [Internet]. 2018;50:8–18. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0944711318302885.
|
| 31. |
Zhu W, Dai Y, Huang M, Li J. Efficacy of Ginger in Preventing Postoperative Nausea and Vomiting: A Systematic Review and Meta‐Analysis. J Nurs Scholarsh [Internet]. 2021;53(6):671–9. Available from: https://sigmapubs.onlinelibrary.wiley.com/doi/10.1111/jnu.12691.
|
| 32. |
Chaiyakunapruk N, Kitikannakorn N, Nathisuwan S, Leeprakobboon K, Leelasettagool C. The efficacy of ginger for the prevention of postoperative nausea and vomiting: A meta-analysis. Am J Obstet Gynecol [Internet]. 2006;194(1):95–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0002937805008914.
|