Abstract
Background: During the COVID-19 era, it is crucial to determine the level of relevant infectious disease knowledge amongst medical students as they may influence public opinion by acting as informal medical advisors to their friends and family. We sought to assess the knowledge of students regarding COVID-19 at a single Polish medical university, to understand the level of knowledge and determine if dedicated COVID-19 education is necessary.
Material and methods: The survey was conducted in Google Forms and access was obtained through the university’s secure email. After exclusion, 1,001 students were enrolled.
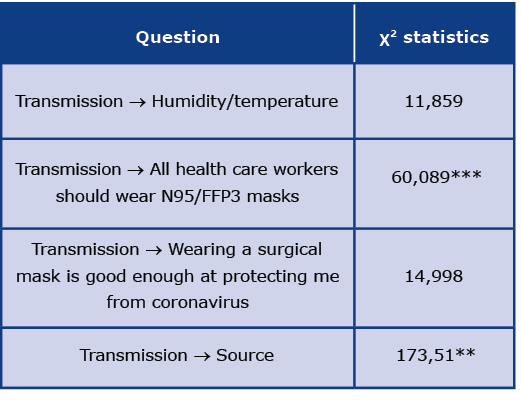
Results: The most common mask used amongst students is a surgical mask. Regarding SARS-CoV-2 transmission, 79,1% chose droplet and 19,3% chose airborne transmission. Only 35% agreed that surgical masks protect them from coronavirus and 70% strongly agreed or agreed that all healthcare workers should wear an N95/FFP3 mask. Students with a healthcare worker in the family more likely agreed that all healthcare workers should wear N95/FFP3 (p = 0.001). The source of information used affected the route of transmission chosen (p = 0.006).
Conclusions: We recommend combating contradictory information by implementing dedicated education into the healthcare student curriculum on SARS-CoV-2, PPE, filtering efficiency of masks, modes of transmission of viruses, and how to use evidence-based medicine.
Citation
Kamieniecki A, Marek D, Dułak N A, Skrzypkowska P, Olofsson H, Szmuda T, Słoniewski P, Ali S. In the midst of imbalance: medical and healthcare students versus SARS-CoV-2. Eur J Transl Clin Med. 2022;5(2):42-52Introduction
Studies have shown that medical students are more willing to obtain the COVID-19 vaccine compared to non-medical students, possibly due to better health awareness [1]. During the pandemic, studies have shown that medical students have a high level of knowledge regarding COVID-19 and could help educate the general public [2-3]. According to a study from the UK, the portrayal of COVID-19 safety measures has been inaccurate. Instead of highlighting the resilience of students and young people even in the absence of support, headlines remained about the few individuals that engaged in risky behaviors despite a raging pandemic [4]. We wanted to determine how knowledgeable medical students are amidst the COVID-19 pandemic and their approach to COVID-19 safety.
Despite the rapid increase of published medical articles regarding COVID-19 [5], virus transmission and protection remain unclear, which is why more research is needed to guide public health [6]. Widespread access to the internet and social media led to the quick dissemination of fake news about the new coronavirus (SARS-CoV-2). Unfortunately, not only anonymous members of society spread disinformation, but also public figures that were believed to be reliable [7]. Commonly implemented face mask mandates raised concerns about mask safety and efficacy. Comfort (physical and psychological), cost, insufficient efficacy with improper usage are only some arguments mentioned against wearing a mask [8]. Another problem is the antivaccine movement. Very rare, but life-threatening adverse effects of vaccines are constantly mentioned [9].
Medical students may have more time than practicing physicians to stay up-to-date with current medical guidelines and new research studies. Medical students may also be more aware of effective public health measures and basic hygiene to control COVID-19. We sought to determine the medical students’ level of knowledge about infectious diseases and COVID-19. By doing so, one can gauge how well medical information about COVID-19 is being disseminated and understood. Moreover, it may encourage medical schools to augment their curriculum by emphasizing relevant public health and infectious disease principles to their students.
Material and methods
The survey aiming to investigate healthcare students’ knowledge about SARS-CoV-2 safety and approaches was designed through a discussion amongst the co-authors. The final version was reviewed and accepted by final-year medical students (n = 4) and neurosurgery specialists guiding this research project (n = 2). The final version of the questionnaire consisted of a total of 36 questions. The first 8 questions consisted of single choice questions regarding demographic data (sex, age, residence, study language, year of studies, exposure to healthcare environments, family in healthcare). Furthermore, 11 questions consisted of the most common types of masks worn, safety measures used, route of transmission, testing positive for COVID-19, vaccination and vaccine efficacy [10]. Next, there were 15 Likert scale statements with answers ranging from: strongly disagree, disagree, I don’t know, agree, strongly agree. Lastly, 2 questions asked about the main sources of information. The survey was conducted by using Google Forms and the link to the survey was sent out through the University’s secure email system. The link was also shared on the English Division Medical student pages on Facebook, therefore using the snowball sampling method. The survey was sent out from January 18th to March 31st 2021.
The statistical analysis was performed using an R software package version 4.1.0. Single choice questions were analyzed using frequency tables and the chi-squared test. Due to the small number of specific groups in some conditions, the p-value is based on the Monte Carlo approach.
Results
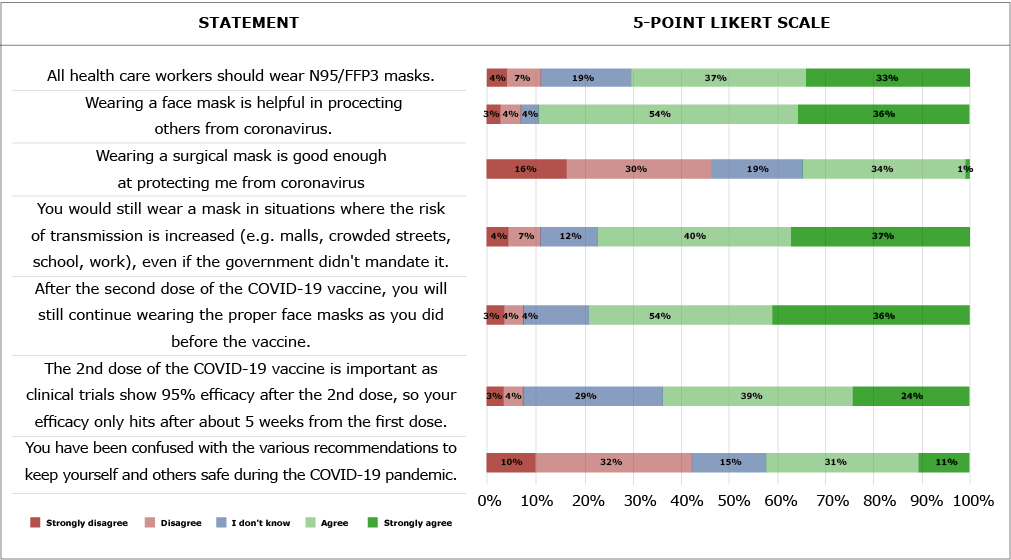
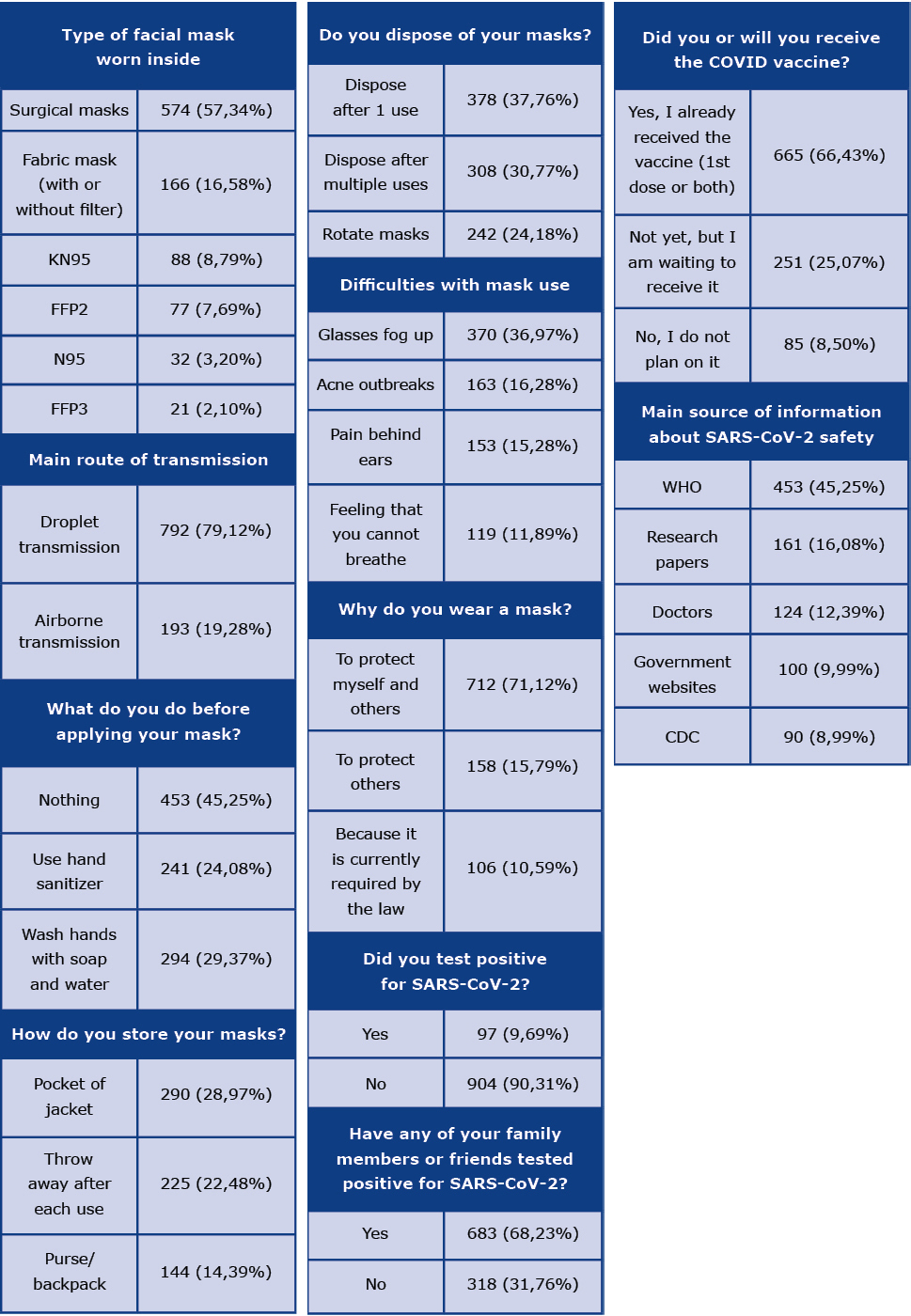
The general demographics of the participants are described in Table 1. The results of single or multiple-choice questions can be seen in Table 2. The most significant 5-point Likert scale questions can be seen in Figure 1, along with the following descriptions of the remainder. Face shields are not considered good enough at protecting yourself from coronavirus by 86,21% of participants. Avoiding high-risk situations and crowded environments are implemented by 72,83% of respondents. 36,46% of respondents stated that they do not know if taking supplements such as vitamin D and vitamin C every day may be used as prophylaxis or treatment of COVID-19. 55,54% agreed or strongly agreed with the statement that they take supplements such as vitamin D, vitamin C, B complex, and/or zinc every day. 65,73% strongly agreed and agreed that in the past month, they have felt uncomfortable not wearing a mask when around others. 65,93% agreed and strongly agreed that other factors such as humidity and temperature affect virus transmission.
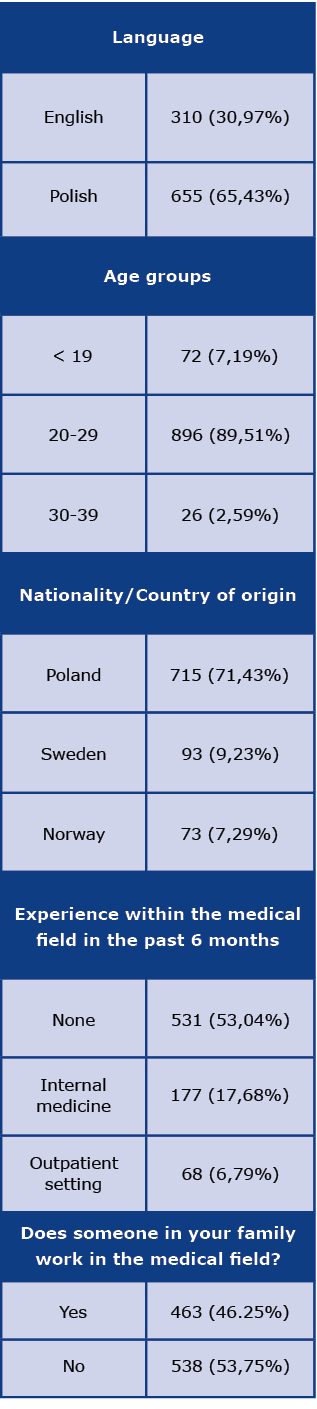
Table 1. General demographics and divisions of participants
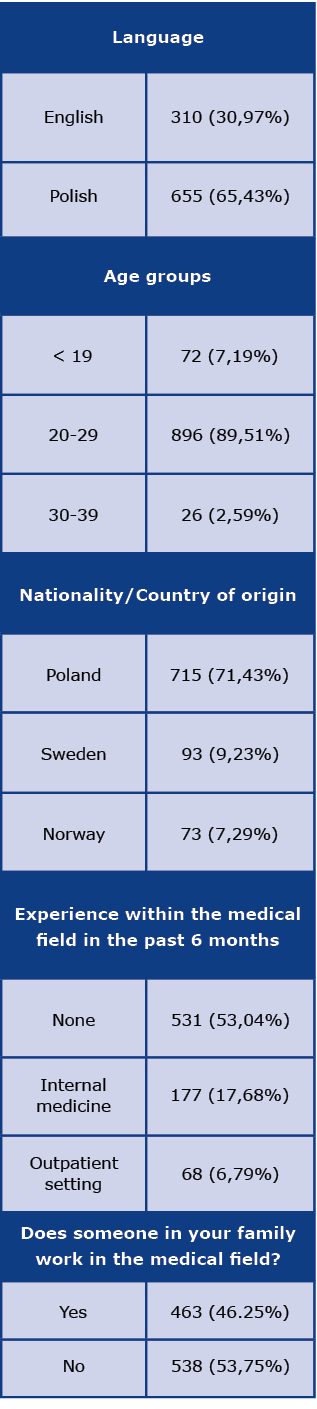
Table 2. Single or multiple choice questions
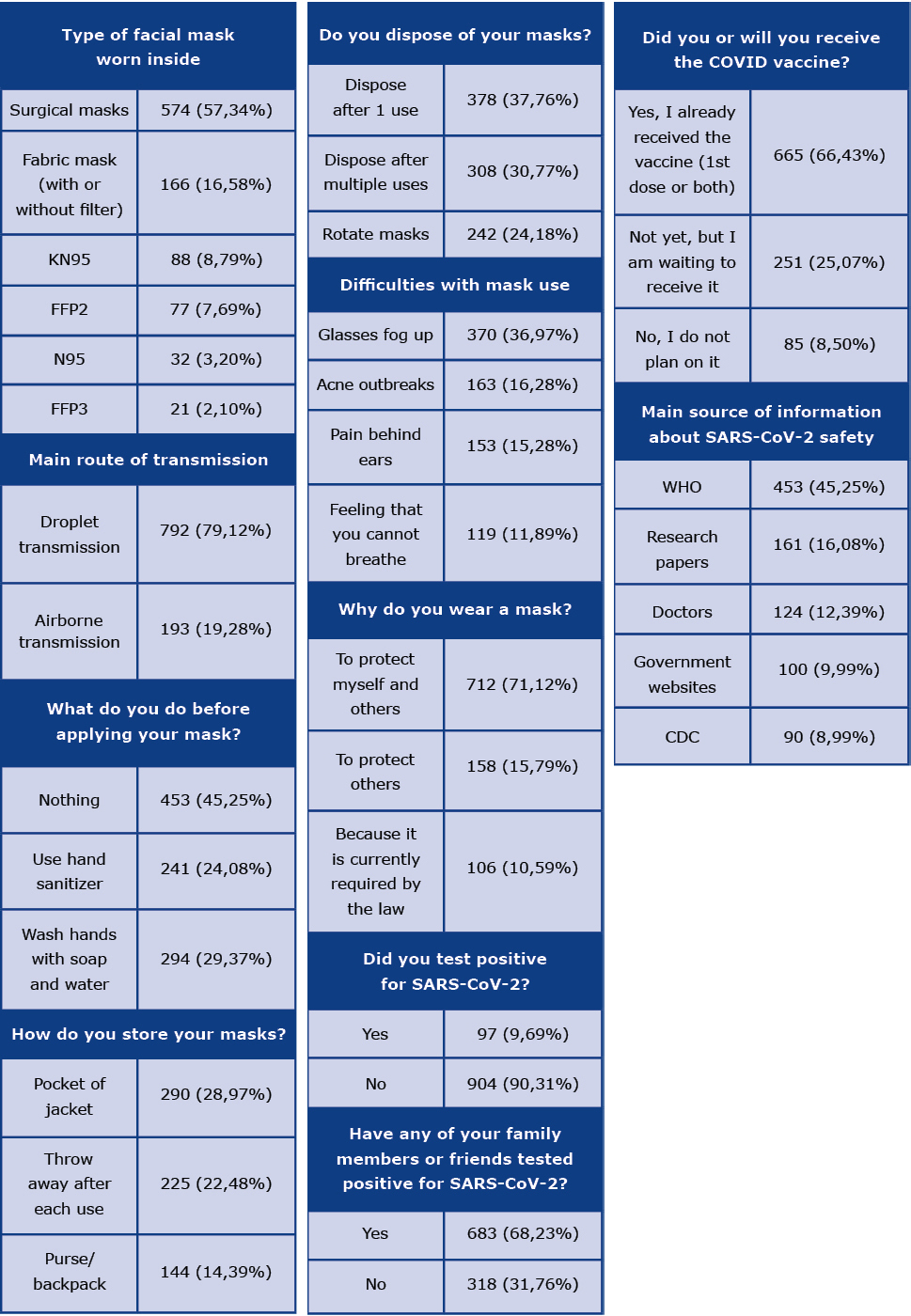
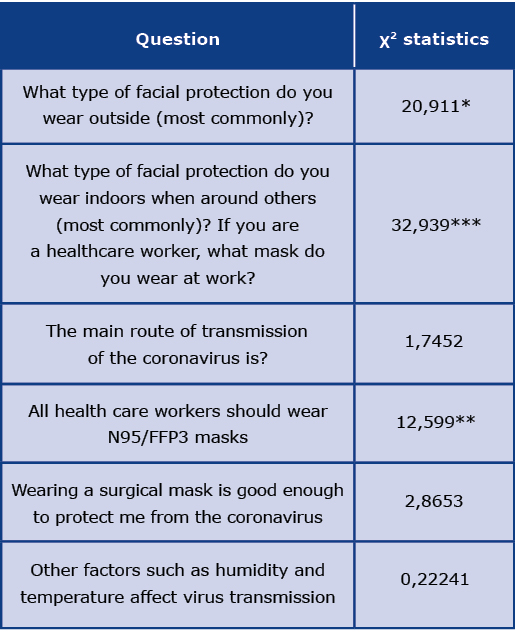
Table 3. The differences between responses of participants with and without relatives in the medical field
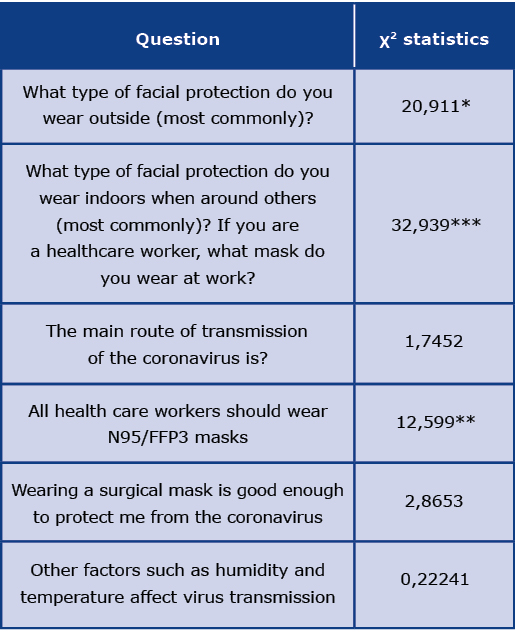
*p < 0,05; **p < 0,01; ***p < 0,001
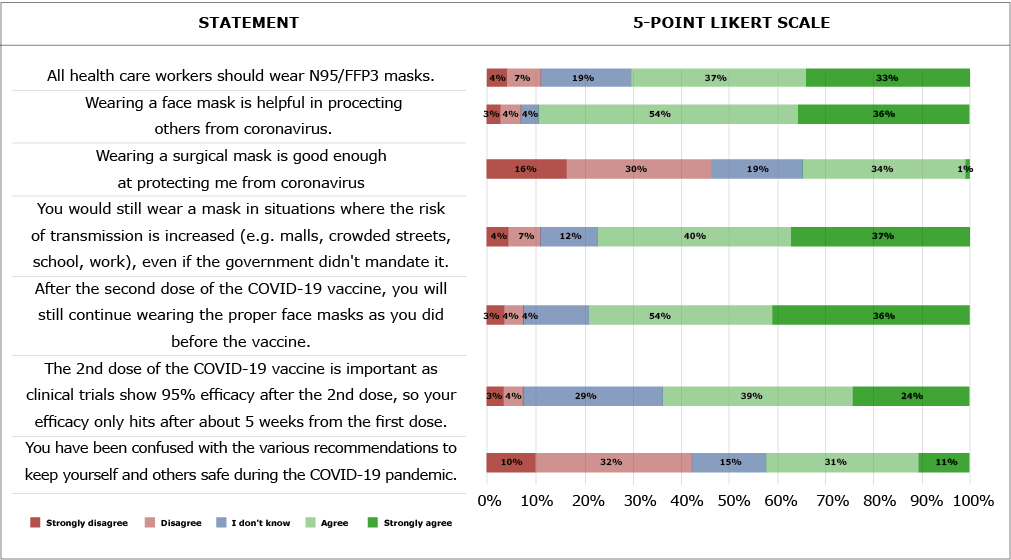
Figure 1. Likert scale figure
The most common mask used outside and indoors by both groups was a surgical mask, but participants with relatives in the medical field more frequently chose KN95, FFP2, and FFP3 masks. Participants without relatives in medical fields rather chose scarves, bandanas, or other fabric masks. Participants with relatives in medical fields agreed or strongly agreed with the statement that “All health care workers should wear N95/FFP3 masks,” while those without relatives in the medical field tended to have no opinion or more frequently disagreed with the statement.
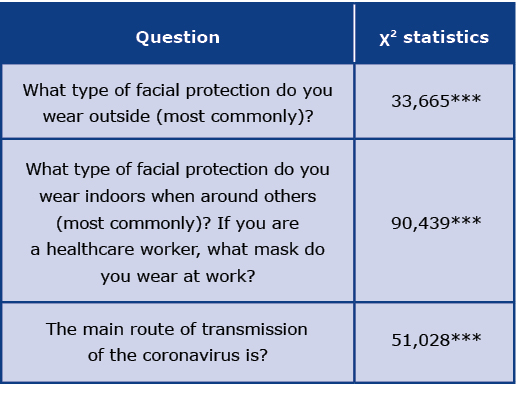
Students most commonly wore surgical masks indoors and outside, but students who studied in the Polish language more frequently had chosen fabric masks with or without filters as their second choice – Table 4.
Table 4. The differences between the responses of students studying in English and Polish
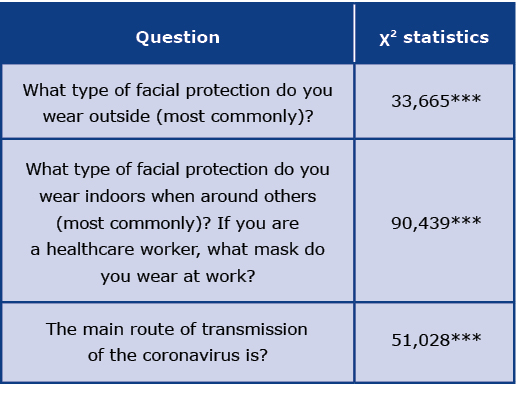
*p < 0,05; **p < 0,01; ***p < 0,001
Table 5 shows the significance of the main route of transmission chosen on the other questions. There were no significant differences between the chosen main route of transmission and the opinion about efficiency of surgical masks, however the participants who chose droplets as a main route of transmission, more frequently agreed with the sentence that all healthcare workers should wear N95/ FFP3 masks than participants who had chosen an airborne route of transmission. The choice of the main route of transmission of SARS-CoV-2 did not affect the understanding of humidity and temperature on transmission (p = 0.596). Even though proportions of main sources of information about the transmission of SARS-CoV-2 were similar, the participants who had chosen the droplet route as the main route, significantly more frequently had pointed to World Health Organization (WHO) and research papers as their main source than people who had chosen the airborne route.
Table 5. Selected differences between different routes of transmission
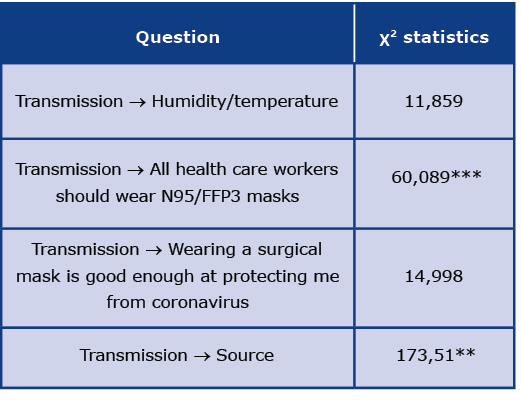
*p < 0,05; **p < 0,01; ***p < 0,001
Discussion
Amid an imbalance between COVID-19 recommendations, it is crucial to find reliable sources of information and examples of role models to follow in society. In our study, we wanted to find out whether medical students' knowledge about SARS-CoV-2 protection is as up-to-date as currently possible, if there are deficiencies in knowledge and if the current generation of healthcare students could potentially be reliable role models for communities in the future. It appears that parts of society started to undermine government recommendations possibly due to facing constant changes (to wear or not to wear masks) within a country as well as in neighboring countries. There are also different opinions about if to wear or not to wear a mask when fully vaccinated due to the delta strain. The inconsistencies between government recommendations can lead to a growing mistrust towards current and forthcoming government recommendations. Recent studies show that higher levels of conspiracy thinking were associated with less adherence to government recommendations or willingness to get vaccinated [11].
Type of masks and the understanding of the transmission of SARS-CoV-2 amongst healthcare students
The debate on the mode of transmission of SARS-CoV-2 is ongoing and far from concluded. We recognize that medical students are not expected to know the definite main route of transmission of SARS-CoV-2, but we sought to determine what they think based on their medical knowledge of other viruses. According to the article by Greenhalgh et al, the dominant route of SARS-CoV-2 is airborne [12]. Interestingly, although most participants stated that droplet transmission is the main route of transmission, around 20% chose airborne transmission. Students must learn to practice medicine based on new research, instead of relying on general opinions. Surprisingly, nearly half of the participants disagreed that surgical masks are effective in protecting themselves from the novel coronavirus even though most participants chose the droplet route of transmission. To enable students to learn and thrive during the pandemic, we believe they should always feel protected. Although most participants chose droplet transmission and most chose that they wear surgical masks most commonly, the majority still agreed that all healthcare workers should wear N95/FFP3 masks. This leads to questions about why most of the respondents think all healthcare workers should wear masks with higher filtering efficiency and if made available, would most medical students choose to wear them?
Interestingly, the participants that chose airborne transmission were less likely to agree that all healthcare workers should wear N95-type masks (p = 0.001). This may have been due to participants that chose airborne transmission knew the importance of higher filtering efficiency masks and the shortage of personal protection equipment (PPE) in settings with the highest risk of transmission, e.g. COVID- -intensive care units. Results from an appraisal study showed that the healthcare workers’ major concern was running out of PPE [13]. Although not statistically significant, fabric or cloth masks were the second most common masks worn amongst students, despite the fact that cloth masks are not worn in operating rooms and there is a lack of evidence of their efficacy [14-15]. It is important to note that the participants who stated they have a healthcare worker in the family, chose different masks than those who did not (p ≤ 0.001). Students without family members in healthcare chose lesser filtering efficiency masks. Students with families in healthcare may have been exposed to more studies and personal experiences with COVID-19 leading to their precautions. Students need to understand what filtering efficiency and PPE is necessary to protect themselves according to the mode of transmission and size of viruses. Additionally, if there is a lack of PPE, students should be taught how to best replicate PPE conditions with available materials and understand that the quality of masks matters for their protection.
The questionnaire did not include ‘aerosolized particles’ among the answer choices, to determine if there would be considerable contrast between answers with fewer choices. Droplets are not present in the air for long periods and instead, they convert into bioaerosol residues which could then remain in the air for extended periods [16]. When droplets evaporate, they become “droplet nuclei” which are driedup particles that contain viruses that can remain airborne and can be widely dispersed over an extensive area [17]. The rate of evaporation is directly related to ambient humidity and temperature and the dispersion of droplet nuclei does depend on ambient conditions [17]. As described by Borak, hotter and more humid environments lead to less dispersion of virus-containing particles [17]. Most healthcare students agreed that other factors such as humidity and temperature affect virus transmission, although this knowledge did not affect their choices of the route of transmission. Educating medical students on the possible routes, conditions, and detailed mechanisms of transmission of viral particles will be crucial for the next generation of medical doctors to stay safe.
Harvey explained the next generation of medical students will need to be able to deal with future pandemics and will live in a world of PPE and the fears of aerosolized dangers. He explained that students may have been told to stay home for their protection and possibly due to the PPE shortage [18]. Most participants agreed that in the past month, they have felt uncomfortable not wearing a mask when around others. Knowledge may alleviate these discomforts. Educating future physicians is crucial in filling in gaps between healthcare demand and access to care and even more so during a pandemic [19]. It was described that the non-essential label should not discourage students, but rather reflect a necessary safety precaution [19]. One of the roles of medical students during the COVID-19 pandemic involved educating peers online. Studies concluded that due to a medical student’s knowledge base, during restricted clinical duties, students could serve as a voice of leadership to non-medical peers [19].
Are medical students and students of healthcare fields good examples for the public to follow?
While face shields are useful as an additional protective measure, they are not good at protecting others due to the expelled droplets that can spread easily [20]. Almost all participants agreed that face shields alone would not protect one from SARS-CoV-2. The face shield could be related to plexiglass used in supermarkets because both are used as a barrier. Large droplets could be blocked, but barriers such as these would not be effective for aerosolized particles [21]. High-quality cloth masks or surgical masks are preferred over masks with exhalation valves to minimize SARS-CoV-2 spread [22]. Our survey participants acknowledged the need to protect others with the use of proper face masks during a time when few were vaccinated.
Despite the Center for Disease Control (CDC) recommendations, not all national governments mandated wearing face masks in public places. On the other hand, in some countries the law required mask use even outdoors. The efficacy of cloth masks in the prevention of infection transmission is quite limited [23] and there has been a constant debate about universal mask use since the COVID-19 pandemic outbreak [24]. The majority of our respondents agreed that they would wear masks in high-risk situations even without a government mandate, which together with social distancing and avoiding high-risk environments are considered to be crucial in controlling the coronavirus spread [24-25]. The willingness to wear a mask without a mandate in high-risk situations signifies the understanding of viral spread by students.
Apart from universal knowledge about SARS-CoV-2 infection prevention which includes wearing a mask, avoiding close contacts, and washing hands [25], alternative approaches with food supplements are widely discussed. Taking vitamin C during the winter months, especially while having cold symptoms is a common practice. In the light of common cold prophylaxis and treatment with zinc [26-27] or vitamin C [28,29], we wanted to determine whether our respondents were using an analogous approach against SARS-CoV-2 infection. This could be relevant to our study population since many adults in Poland are vitamin D deficient [30]. However, a recent study by Li et al. observed no association between low vitamin D levels and SARS-CoV-2 seropositivity after adjusting for potential cofounders [31]. In a randomized control trial Murai et al. measured the efficacy of a single high dose of vitamin D3 on COVID-19 patients’ duration of hospital stay. In comparison with placebo, there was no significant reduction in days of hospital stay [32]. Current coronavirus prevention guidelines do not recommend any pharmacological prophylaxis due to the lack of data supporting its efficacy [33]. Some studies have proven antiviral, anti-inflammatory, and antioxidant effects of several food supplements [34-36], however, it is worth noting that potential laboratory effects may not be clinically relevant. These disagreements most likely led to the hesitancy of our respondents when answering questions about taking supplements as possible prophylaxis or treatment of COVID-19. Their responses resembled what was available in the literature at the time and signifies that they could be role models for the public to learn from. Additionally, students could help in answering common misconceptions about dietary supplementation for COVID-19 infection.
Are medical students and health science students good examples for post-vaccine public health protection?
Although 90% of respondents never tested positive for SARS-CoV-2, there was still a high amount of positive cases among their close family members and friends. Almost half of the participants had someone in their family that works in the medical field. This confirms the importance of awareness of safety measures in this specific group. Previous studies have shown [37] that more than 90% of medical students are aware, but only have a superficial understanding of the disease’s etiology, currently known modes of transmission, primary symptoms and risk perception. There is a need to improve student awareness about safety measures to strengthen the possible pivotal role students can play in public health awareness about the SARS-CoV-2 [2, 19, 37]. Most participants knew that the 2nd dose of an mRNA vaccination series is important to reach maximum vaccine efficacy. The high willingness to get vaccinated against SARSCoV-2 amongst students is yet another affirmation of the possibility of students being on the frontline of combating SARS-CoV-2 misinformation. The poor attitude of the general population towards vaccination is mainly due to the mistrust of vaccine benefits and concerns about its adverse effects. Healthcare students can be a great resource for the general population’s doubts about the vaccine. Students should be up-to-date on new publications that could impact the public’s health decisions and could reduce vaccine hesitancy. Students should be taught how to define vaccine risks and benefits.
General problems found amongst students and approaches to public health
The most common primary source of information about face masks and COVID-19 safety was the WHO, research papers and doctors. Surprisingly, research papers were not the most common source amongst students. The source of information that participants chose had a significant effect on their answer to the questions about the main route of transmission (p=0.006). Although participants used various sources, the most commonly chosen route of transmission remained the same amongst groups. In a study about what the world expects from the WHO, there were multiple deficiencies of the WHO listed along with recommendations for improvement [38]. Precautions can be taken only when national bodies responsible for epidemic control agree and recognize the importance of the route of transmission which can then lead to appropriate actions [39]. Mask protection and filtering efficiency should also be topics that medical students are taught and truly understand.
Due to the delta variant, the newest WHO recommendation [40] for fully vaccinated people is to continue wearing face masks. Our study group reflected these recommendations with the high interest of our respondents in choosing to continue wearing proper face masks post-vaccination. However, caution should be drawn from this conclusion due to the time frame; at the time of vaccinating these medical students, most of the general public was not vaccinated yet. When new mutations were discovered, their impact was unknown [41]. At the time (as of July 1st 2021), 57,1% of the population of Israel was fully vaccinated [42]. Due to the national vaccination campaign, Israel became a role model for other countries regarding an efficient vaccination process. Now, the world is looking at the situation in Israel with fear due to the new COVID-19 delta variant, which was proven to infect some fully vaccinated adults [43-44]. With rising daily coronavirus infection rates, Israel has reimposed the requirement of wearing masks indoors for everyone [45-46], while the WHO has also recommended that fully vaccinated people continue wearing masks. This may be the reason for contradictory information between WHO and CDC recommendations. It is noteworthy that according to a recent study the Pfizer-BioNTech's tozinameran vaccine (in Europe marketed as Comirnaty®) vaccine has a minimal decrease in effectiveness (about a 5,5% decrease) against the new delta variant [47]. Interestingly, the WHO’s recommendations do not match the CDC’s recommendations for fully vaccinated people at the moment. According to the CDC’s newest public health recommendations, resuming most activities for fully vaccinated people without wearing masks is recommended [48]. Fully vaccinated people also do not need COVID-testing after exposure and before or after travel. Fully vaccinated people also do not need to self-quarantine, which is different from the current WHO recommendations [48-49]. Students should be taught how to interpret recommendations because such discrepancies can be very distressing, particularly to those who are paying close attention to the pandemic. Students should be informed on how to interpret studies about new virus variants to be able to determine risks for themselves and their future patients.
Pre-pandemic studies have found that there is a decline in empathy possibly due to the increase of psychological stress in medical school and residency which can further compromise professionalism and can threaten the quality of healthcare [50]. Lack of balance was mentioned as the main stressor for medical students [51]. The constantly changing COVID restrictions and schedules for students would not be defined as consistent. Studies determined it will be important to study the extent of student adaptation during the COVID-19 pandemic and its effect on medical education overall [52]. With more adequate availability of PPE, medical students should be allowed back to the bedside to learn valuable lessons from frontline survivors [53]. Medical schools can consider adding virtual credits for students taking part in scientific writing and continuing student engagement whenever possible [53]. Studies have shown that COVID-19 had the greatest effect on students’ confidence and preparedness to jump from student to doctor [54]. Barriers to critical thinking have been described amongst medical students with obedience to the system being one of the contributing factors [55]. Anxiety, stress, and fatigue were shown to prevent critical focus and thinking [55]. It is important to prioritize teaching medical students to filter out what the media and news intensify and focus on evidence-based medicine. Students must be included in medical education so that when they finish their studies, they can continue to support public health while having the psychological strength to do so.
There was a bias of more female respondents and participants from the Polish division. Response bias may be present due to healthcare and medical students’ desirable answers to topics that are perceived as sensitive such as health behaviors and safety [56-57]. Nonetheless, responses varied and not all participants chose desirable answers to controversial statements like government mandates and avoiding high-risk situations. Caution should be taken when drawing conclusions from this study due to the time frame the survey was administered. At the time of the survey, (January 18th – March 31st 2021) the post-vaccination time frame for most students was during a time when most of the general population was still not vaccinated.
Conclusions
Medical and healthcare students have the potential to be even better role models for the general public to follow. Students had a high willingness to get vaccinated and the majority knew the importance of the 2nd dose of an mRNA series in reaching maximum efficacy. There is a need to educate students on the filtering efficiency of masks and what PPE is necessary according to the mode of transmission and size of viruses. Although most participants stated that droplet is the route of SARS-CoV-2 transmission and most marked that they wear surgical masks most commonly, they didn’t believe surgical masks protect them and stated that all healthcare workers should wear N95/FFP3 masks. Students should be informed on how to find appropriate sources of information and how to interpret studies about new virus variants to be able to determine risks for themselves and their future patients.
Acknowledgments
The authors declare that there is no conflict of financial or personal interests.
Funding
None.
Conflicts of interests
None.
References
| 1. |
Szmyd B, Bartoszek A, Karuga FF, Staniecka K, Błaszczyk M, Radek M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines [Internet]. 2021 Feb 5;9(2):128. Available from: https://www.mdpi.com/2076-393X/9/2/128.
|
| 2. |
Alsoghair M, Almazyad M, Alburaykan T, Alsultan A, Alnughaymishi A, Almazyad S, et al. Medical Students and COVID-19: Knowledge, Preventive Behaviors, and Risk Perception. Int J Environ Res Public Health [Internet]. 2021 Jan 19;18(2):842. Available from: https://www.mdpi.com/1660-4601/18/2/842.
|
| 3. |
Matusiak Ł, Szepietowska M, Krajewski P, Białynicki-Birula R, Szepietowski J. Face masks use during the COVID-19 pandemic: Differences in attitudes and practices between medical and non-medical students. A survey of 2256 students in Poland. Adv Clin Exp Med [Internet]. 2020 Oct 30;29(10):1201–3. Available from: http://www.advances.umed.wroc.pl/pdf/2020/29/10/1201.pdf.
|
| 4. |
Reicher S, Drury J. Pandemic fatigue? How adherence to covid-19 regulations has been misrepresented and why it matters. BMJ [Internet]. 2021 Jan 18;372:n137. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.n137.
|
| 5. |
Chen Q, Allot A, Lu Z. LitCovid: an open database of COVID-19 literature. Nucleic Acids Res [Internet]. 2021 Jan 8;49(D1):D1534–40. Available from: https://academic.oup.com/nar/article/49/D1/D1534/5964074.
|
| 6. |
The Lancet Respiratory Medicine. COVID-19 transmission – up in the air. Lancet Respir Med [Internet]. 2020 Dec;8(12):1159. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2213260020305142.
|
| 7. |
Orso D, Federici N, Copetti R, Vetrugno L, Bove T. Infodemic and the spread of fake news in the COVID-19-era. Eur J Emerg Med [Internet]. 2020 Oct 23;27(5):327–8. Available from: https://journals.lww.com/10.1097/MEJ.0000000000000713.
|
| 8. |
Matuschek C, Moll F, Fangerau H, Fischer JC, Zänker K, van Griensven M, et al. Face masks: benefits and risks during the COVID-19 crisis. Eur J Med Res [Internet]. 2020 Dec 12;25(1):32. Available from: https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-020-00430-5.
|
| 9. |
Hotez P. COVID vaccines: time to confront anti-vax aggression. Nature [Internet]. 2021 Apr 29;592(7856):661–661. Available from: http://www.nature.com/articles/d41586-021-01084-x.
|
| 10. |
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med [Internet]. 2020 Dec 31;383(27):2603–15. Available from: http://www.nejm.org/doi/10.1056/NEJMoa2034577.
|
| 11. |
Freeman D, Waite F, Rosebrock L, Petit A, Causier C, East A, et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol Med [Internet]. 2022 Jan 21;52(2):251–63. Available from: https://www.cambridge.org/core/product/identifier/S0033291720001890/type/journal_article.
|
| 12. |
Greenhalgh T, Jimenez JL, Prather KA, Tufekci Z, Fisman D, Schooley R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet. 2021 May;397(10285):1603–5.
|
| 13. |
Hoernke K, Djellouli N, Andrews L, Lewis-Jackson S, Manby L, Martin S, et al. Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open [Internet]. 2021 Jan 20;11(1):e046199. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2020-046199.
|
| 14. |
Chughtai AA, Seale H, Macintyre CR. Effectiveness of Cloth Masks for Protection Against Severe Acute Respiratory Syndrome Coronavirus 2. Emerg Infect Dis [Internet]. 2020 Oct;26(10). Available from: http://wwwnc.cdc.gov/eid/article/26/10/20-0948_article.htm.
|
| 15. |
Chughtai AA, Seale H, MacIntyre CR. Use of cloth masks in the practice of infection control – evidence and policy gaps. Int J Infect Control [Internet]. 2013 Jun;9(3):3. Available from: https://www.ijic.info/article/view/11366.
|
| 16. |
Jayaweera M, Perera H, Gunawardana B, Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ Res [Internet]. 2020 Sep;188:109819. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0013935120307143.
|
| 17. |
Borak J. Airborne Transmission of COVID-19. Occup Med (Chic Ill) [Internet]. 2020 Jul 17;70(5):297–9. Available from: https://academic.oup.com/occmed/article/70/5/297/5849370.
|
| 18. |
Harvey EJ. A lost cohort of medical students. Can J Surg [Internet]. 2020 Oct 1;63(5):E489–E489. Available from: http://www.canjsurg.ca/lookup/doi/10.1503/cjs.020620.
|
| 19. |
Patrinely JR, Zakria D, Berkowitz ST, Johnson DB, Totten DJ. COVID-19: the Emerging Role of Medical Student Involvement. Med Sci Educ [Internet]. 2020 Dec 12;30(4):1641–3. Available from: https://link.springer.com/10.1007/s40670-020-01052-6.
|
| 20. |
Khan MM, Parab SR. Safety Guidelines for Sterility of Face Shields During COVID 19 Pandemic. Indian J Otolaryngol Head Neck Surg [Internet]. 2021 Mar 30;73(1):85–6. Available from: https://link.springer.com/10.1007/s12070-020-01865-2.
|
| 21. |
Pilkington BC, Wilkins V, Nichols DB. Educating ethically during COVID-19. Int J Ethics Educ [Internet]. 2021 Apr 29;6(1):177–93. Available from: http://link.springer.com/10.1007/s40889-021-00120-8.
|
| 22. |
Verma S, Dhanak M, Frankenfield J. Visualizing droplet dispersal for face shields and masks with exhalation valves. Phys Fluids [Internet]. 2020 Sep 1;32(9):091701. Available from: http://aip.scitation.org/doi/10.1063/5.0022968.
|
| 23. |
Sharma S, Mishra M, Mudgal S. Efficacy of cloth face mask in prevention of novel coronavirus infection transmission: A systematic review and meta-analysis. J Educ Health Promot [Internet]. 2020 Jul;9(1):192. Available from: http://www.jehp.net/text.asp?2020/9/1/192/290942.
|
| 24. |
Tirupathi R, Bharathidasan K, Palabindala V, Salim SA, Al-Tawfiq JA. Comprehensive review of mask utility and challenges during the COVID-19 pandemic. Le Infez Med [Internet]. 2020 Jun 1;28(suppl 1):57–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32532940.
|
| 25. |
How to Protect Yourself & Others | CDC [Internet]. 2022 [cited 2022 Aug 10]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html.
|
| 26. |
Al-Nakib W, Higgins PG, Barrow I, Batstone G, Tyrrell DAJ. Prophylaxis and treatment of rhinovirus colds with zinc gluconate lozenges. J Antimicrob Chemother [Internet]. 1987 Dec;20(6):893–901. Available from: https://academic.oup.com/jac/article-lookup/doi/10.1093/jac/20.6.893.
|
| 27. |
Science M, Johnstone J, Roth DE, Guyatt G, Loeb M. Zinc for the treatment of the common cold: a systematic review and meta-analysis of randomized controlled trials. Can Med Assoc J [Internet]. 2012 Jul 10;184(10):E551–61. Available from: http://www.cmaj.ca/lookup/doi/10.1503/cmaj.111990.
|
| 28. |
Sasazuki S, Sasaki S, Tsubono Y, Okubo S, Hayashi M, Tsugane S. Effect of vitamin C on common cold: randomized controlled trial. Eur J Clin Nutr [Internet]. 2006 Jan 1;60(1):9–17. Available from: https://www.nature.com/articles/1602261.
|
| 29. |
Johnston C, Barkyoumb G, Schumacher S. Vitamin C Supplementation Slightly Improves Physical Activity Levels and Reduces Cold Incidence in Men with Marginal Vitamin C Status: A Randomized Controlled Trial. Nutrients [Internet]. 2014 Jul 9;6(7):2572–83. Available from: http://www.mdpi.com/2072-6643/6/7/2572.
|
| 30. |
Płudowski P, Ducki C, Konstantynowicz J, Jaworski M. Vitamin D status in Poland. Polish Arch Intern Med [Internet]. 2016 Aug 9;126(7–8):530–9. Available from: http://pamw.pl/en/node/3479.
|
| 31. |
Li Y, Tong CH, Bare LA, Devlin JJ. Assessment of the Association of Vitamin D Level With SARS-CoV-2 Seropositivity Among Working-Age Adults. JAMA Netw Open [Internet]. 2021 May 19;4(5):e2111634. Available from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2779952.
|
| 32. |
Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CSC, et al. Effect of a Single High Dose of Vitamin D 3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19. JAMA [Internet]. 2021 Mar 16;325(11):1053. Available from: https://jamanetwork.com/journals/jama/fullarticle/2776738.
|
| 33. |
Adams KK, Baker WL, Sobieraj DM. Myth Busters: Dietary Supplements and COVID-19: https://doi.org/101177/1060028020928052. 2020 May;54(8):820–6.
|
| 34. |
Mrityunjaya M, Pavithra V, Neelam R, Janhavi P, Halami PM, Ravindra P V. Immune-Boosting, Antioxidant and Anti-inflammatory Food Supplements Targeting Pathogenesis of COVID-19. Front Immunol [Internet]. 2020 Oct 7;11:2337. Available from: https://www.frontiersin.org/article/10.3389/fimmu.2020.570122/full.
|
| 35. |
Sahebnasagh A, Saghafi F, Avan R, Khoshi A, Khataminia M, Safdari M, et al. The prophylaxis and treatment potential of supplements for COVID-19. Eur J Pharmacol [Internet]. 2020 Nov;887:173530. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0014299920306221.
|
| 36. |
Shakoor H, Feehan J, Al Dhaheri AS, Ali HI, Platat C, Ismail LC, et al. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: Could they help against COVID-19? Maturitas [Internet]. 2021 Jan;143:1–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0378512220303467.
|
| 37. |
Ikhaq A, Bint E Riaz H, Bashir I, Ijaz F. Awareness and Attitude of Undergraduate Medical Students towards 2019-novel Corona virus. Pakistan J Med Sci [Internet]. 2020 May 18;36(COVID19-S4):S32. Available from: https://www.pjms.org.pk/index.php/pjms/article/view/2636.
|
| 38. |
Kuznetsova L. COVID-19: The World Community Expects the World Health Organization to Play a Stronger Leadership and Coordination Role in Pandemics Control. Front Public Heal [Internet]. 2020 Sep 8;8:470. Available from: https://www.frontiersin.org/article/10.3389/fpubh.2020.00470/full.
|
| 39. |
Morawska L, Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ Int [Internet]. 2020 Jun;139:105730. Available from: https://linkinghub.elsevier.com/retrieve/pii/S016041202031254X.
|
| 40. |
Coronavirus disease (COVID-19) [Internet]. Geneva; 2020. Available from: https://apps.who.int/iris/handle/10665/334383.
|
| 41. |
Grubaugh ND, Hanage WP, Rasmussen AL. Making Sense of Mutation: What D614G Means for the COVID-19 Pandemic Remains Unclear. Cell [Internet]. 2020 Aug;182(4):794–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0092867420308175.
|
| 42. |
Coronavirus (COVID-19) Vaccinations - Statistics and Research / Our World in Data [Internet]. 2021 [cited 2021 Oct 12]. Available from: https://ourworldindata.org/covid-vaccinations?country=JPN~USA.
|
| 43. |
Lieber D. Delta Variant Outbreak in Israel Infects Some Vaccinated Adults. Wall Str J [Internet]. 2021; Available from: https://www.wsj.com/articles/vaccinated-people-account-for-half-of-new-covid-19-delta-cases-in-israeli-outbreak-11624624326.
|
| 44. |
Hendrix S. Israel says vaccine protecting it against delta variant. Washington Post [Internet]. 2021; Available from: https://www.washingtonpost.com/world/middle_east/israel-delta-vaccine-shield-holding/2021/06/28/1ba865b2-d7e1-11eb-8c87-ad6f27918c78_story.html.
|
| 45. |
Coronavirus: Israel races to vaccinate children as Delta variant cases swell South [Internet]. China Morning Post. 2021 [cited 2021 Oct 12]. Available from: https://www.scmp.com/news/world/middle-east/article/3139463/coronavirus-israel-races-vaccinate-children-delta-variant?module=perpetual_scroll_0&pgtype=article&campaign=3139463.
|
| 46. |
Staff T. Bennett: Young people must get vaccinated to avoid reinstatement of restrictions [Internet]. Times of Israel. 2021 [cited 2021 Oct 12]. Available from: https://www.timesofisrael.com/cases-rise-but-hospitalizations-remain-low-as-coronavirus-cabinet-set-to-meet/.
|
| 47. |
Bernal JL, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N Engl J Med [Internet]. 2021 Aug 12;385(7):585–94. Available from: http://www.nejm.org/doi/10.1056/NEJMoa2108891.
|
| 48. |
Interim Public Health Recommendations for Fully Vaccinated People [Internet]. CDC. 2021 [cited 2021 Oct 22]. Available from: https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/grc-747228?lang=en.
|
| 49. |
Episode #23 - I am vaccinated, what next? [Internet]. WHO. 2021 [cited 2021 Oct 12]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-23---i-am-vaccinated-what-next.
|
| 50. |
Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy Decline and Its Reasons: A Systematic Review of Studies With Medical Students and Residents. Acad Med [Internet]. 2011 Aug;86(8):996–1009. Available from: http://journals.lww.com/00001888-201108000-00024.
|
| 51. |
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online [Internet]. 2018 Jan 5;23(1):1530558. Available from: https://www.tandfonline.com/doi/full/10.1080/10872981.2018.1530558.
|
| 52. |
Ferrel MN, Ryan JJ. The Impact of COVID-19 on Medical Education. Cureus [Internet]. 2020 Mar 31;12(3). Available from: https://www.cureus.com/articles/29902-the-impact-of-covid-19-on-medical-education.
|
| 53. |
Chandratre S. Medical Students and COVID-19: Challenges and Supportive Strategies. J Med Educ Curric Dev [Internet]. 2020 Jan 24;7:238212052093505. Available from: http://journals.sagepub.com/doi/10.1177/2382120520935059.
|
| 54. |
Choi B, Jegatheeswaran L, Minocha A, Alhilani M, Nakhoul M, Mutengesa E. The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC Med Educ [Internet]. 2020 Dec 29;20(1):206. Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02117-1.
|
| 55. |
Kasalaei A, Amini M, Nabeiei P, Bazrafkan L, Mousavinezhad H. Barriers of Critical Thinking in Medical Students’ Curriculum from the Viewpoint of Medical Education Experts: A Qualitative Study. J Adv Med Educ Prof [Internet]. 2020 Apr;8(2):72–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32426391.
|