Attempt at profiling and regionalisation of COVID-19 vaccine campaigns in Poland – preliminary results
Abstract
Background
Social attitudes and context have a fundamental impact on the COVID-19 vaccine acceptance. This issue will be challenging the existing Polish public health infrastructure during the planned immunisation program.
Material and methods
We attempt to exemplify Poland-specific social background via causal diagram and regional factor analysis based on dimensions (epidemiological potential, ability to act, magical thinking, corona scepticism, information needs etc.) by December 2020 – shortly before vaccination started.
Results
We identified several potential target subpopulations and provide possible regional classification. We distinguish clusters of regions where communication strategies should be taken into consideration: 1) extending campaign reach, common social goods and conformism; 2) individual’s profits and misinformation blocking.
Conclusions
We are signalling the need for profiling and regionalization in campaigns and propose possible starting points for protocols for various voivodeships when safe and effective vaccines are available in Poland.
Citation
Jarynowski A, Skawina I. Attempt at profiling and regionalisation of COVID-19 vaccine campaigns in Poland – preliminary results. Eur J Transl Clin Med. 2021;4(1):13-21Introduction
The National Anti-Covid Immunisation Programme announced on 08.12.2020 [1] involves a widespread, voluntary and free vaccination to take place in Poland in 2021. Discovery, delivery and logistics of candidates or soon available SARS-CoV-2 vaccines seem to be one of the biggest challenges in the history of medicine [2]. However, due to shortened clinical trials or conspiracy theories [3-4], the issue of vaccine acceptance arose in particular societies. According to the opinion polls and surveys [5-9], less than 50% of the Polish adult population are willing to undergo any kind of anti-coronavirus vaccination and the majority still remains undecided. In Poland, confidence in vaccines for other diseases is a little below EU average, however Poles less confident over time [10]. The Polish government plans to carry out a large information and pro-turnout campaign [1], but empirical research on the relationship between vaccination uptake intent and acceptance in various Polish subpopulations is necessary [11-12]. The willingness [13-15] of a given person to be vaccinated is a combination of various factors: rational (homo oeconomicus), such as efficacy vs. safety calculation, psychological (homo psychologicus), such as trust or cognitive dissonance, as well as normative factors (homo sociologicus), like cultural or socialization issues. Achieving high acceptance of immunization in the population is required in order to achieve a high coverage level needed to reach herd immunity [11]. This will be a complex challenge [16-17] necessitating collaboration among various stakeholders, e.g. medical scientists, communication researchers and marketers, social and cognitive scientists, policy makers, public health officials, NGOs and patient group representatives and health care workers.
Material and methods
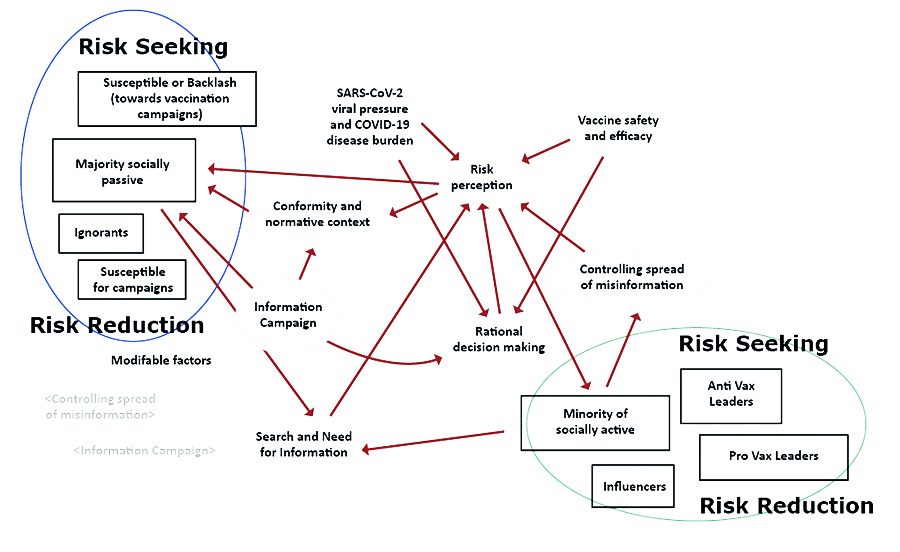
Due to the lack of empirical evidence based on the Polish population [11], some analysts and experts in medical communication are extrapolating the results from foreign studies, mainly from English-speaking countries. However, it could lead to cognitive errors and misinterpretation, because the Polish sociocultural context has its own unique set of factors that significantly differ between geographical regions of Poland [18- 19]. For instance, belief in conspiracy theories about COVID-19 significantly increases with eHealth literacy [20], just as vaccine safety negation increases with the education level [5, 21]. None of the conducted studies showed a univariate relationship between political views and various definitions of vaccination acceptance [5, 21-22]. On the other hand, opinions on mandatory prophylactic vaccination strongly depend on the education level, etc place of living, declared financial situation, religiosity etc [23]. In order to understand Poland-specific perspectives of COVID-19, both theoretical and pre-pandemic knowledge [11] should be accompanied with empirical research containing a rich variety of the concerns which can be captured via survey, observation, in-depth interviews or secondary data analysis [24-25]. It would then allow for identifying and profiling main target groups (Fig. 1), which in turn could increase the effectiveness of campaigns with main modifiable factors [3], such as vaccine information (information campaigns) and mitigate the harmful effects of misinformation and disinformation (information spread).
Some attempts to characterize each subpopulation have already been made (Fig. 1): for instance, it seems that young adult males are overrepresented within the “Ignorant” group, females among the “Anti-vaccination Leaders” and the elderly among the “Susceptible to campaigns”, populists among “Susceptible to backlash” [5, 26-28]. However, some further profiling is needed. It is especially noticeable with regard to populations previously marginalized in pandemic social studies [24-25], i.e. the Polish elderly (disproportionately affected by the COVID-19), who need adequate support and information networks concerning the vaccination, as well as immigrants, who might be facing language barriers [29]. These groups are especially hardly able to properly estimate the risk-benefit ratio related to vaccination, so reaching them and providing information will be a key influencing factor. Moreover, some topics and concerns based on other vaccination programs [30-38] and COVID-19 vaccine [5, 39-41] have been preliminarily mapped.
Figure 1. An attempt to use a causal diagram to describe the Polish social system with regard to vaccination amidst the pandemic. Rectangles are subpopulations (with its own composition of age, gender, place of residence, income, etc.), arrows indicate main interactions, shadow variables are modifiable factors (information campaigns and controlling the spread of (mis)-information)
Results
To understand the ground for COVID-19 vaccine acceptance in Poland, let us consider the data available at the voivodeship level (NUTS-2). In the various theories of social action usually the common assumption is that one should distinguish attitudes (as well as opinions) and socio-epidemiological background (context) from the sphere of activity (actions). A given population may not be fully confident about the COVID-19 vaccine, but it could be not enough for an active refusal - for this, a fertile social environment is needed. For instance, the inhabitants of big cities declare skipping mandatory vaccination a few times more than the rest of the population [23]. A high fraction of people who were not convinced by immunisation and did not trust doctors, science or the government, were still agreeing to vaccination [21].
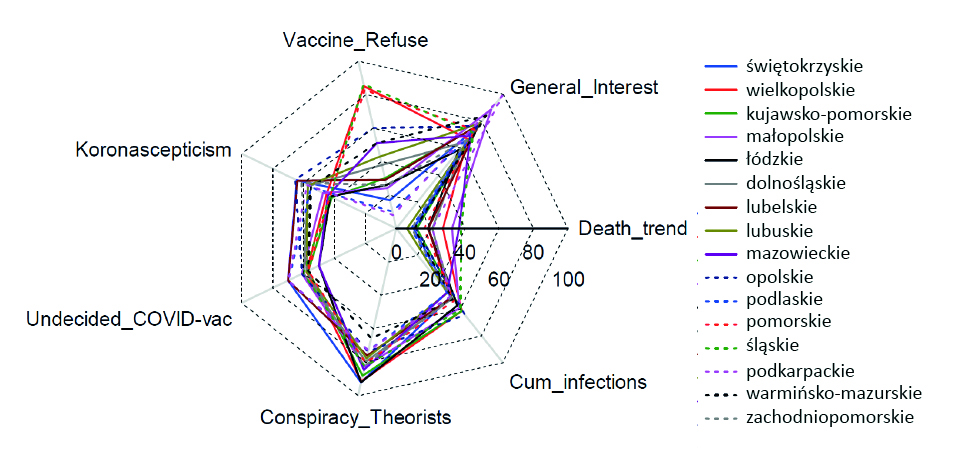
In order to operationalize the concepts of interest, let us try to define the following socio-epidemiological dimensions:
1. Corona sceptisism – mean Google relative search volume (RSV) [42] 25.07-25.08.2020 (30 days) for phrases: “fałszywa pandemia” (false pandemic), “plandemia” (plandemic), “epidemia+ściema” (fake epidemic). The level of corona scepticism could be a proxy for susceptibility to backlash [43] (Fig. 1).
2. General_interest – interest of the general population in coronavirus by mean Google RSV [42] 25.07-25.08.2020 (30 days) for phrases: “koronawirus” (coronavirus), “zakażenia” (infections) and Coronavirus topic. To some extent, this measures information needs [11] with regard to the disease (Fig. 1).
3. Conspiracy_Theorists: Conspiracy Theories Potential is defined as an interest of the general population in various paranatural or conspiracy concepts by mean Google RSV [42] 08.12.2019-07.12.2020 (12 months) for phrases: QAnon, Kabala, UFO, as well as Horoscope and New World Order topics. Magical thinking [44] is known to anticorrelate with trust in vaccines [21] in Poland.
4. Cum_infections – Cumulative SARS-CoV-2 case notification number since the beginning of the epidemic until 8 XII 2020 per 5000 inhabitants [16].
5. Death_trend – Trend in the number of deaths defined as the trend coefficient of daily death case registry due to COVID-19 1 XI – 8 XII 2020 [19]. Experienced total viral pressure (point 4) and recent disease burden (point 5) known as epidemiological potential in local neighborhoods may infer risk perception [45, 14].
6. Vaccine_refuse – vaccination refusal rate [46] for non-medical reasons (per 10000 planned vaccination aged 0-19 in 2018). This could be a proxy of potential ability to act.
7. Undecided_COVID-vac – percentage of respondents who in the Kantar survey [8] (mid October 2020) did not declare willingness to undergo vaccination against COVID-19 (on a macroregion NUTS-1 level only). It is a proxy of the size of subpopulation which could be susceptible to campaigns (Fig. 1).
Negative attitudes towards childhood immunisation according to surveys performed 2009 by voivodeship [47] anticorrelated with vaccine refusal rate, which suggest dissonance between attitude and action. It is worth noting that these dimensions may be defined in a different manner and many other dimensions could be added. Moreover, epidemiological potential and general interest (Fig. 1, 2) are highly temporal variables, so a longitudinal approach would be prefered as we have already seen that our observables are changing in time [48].
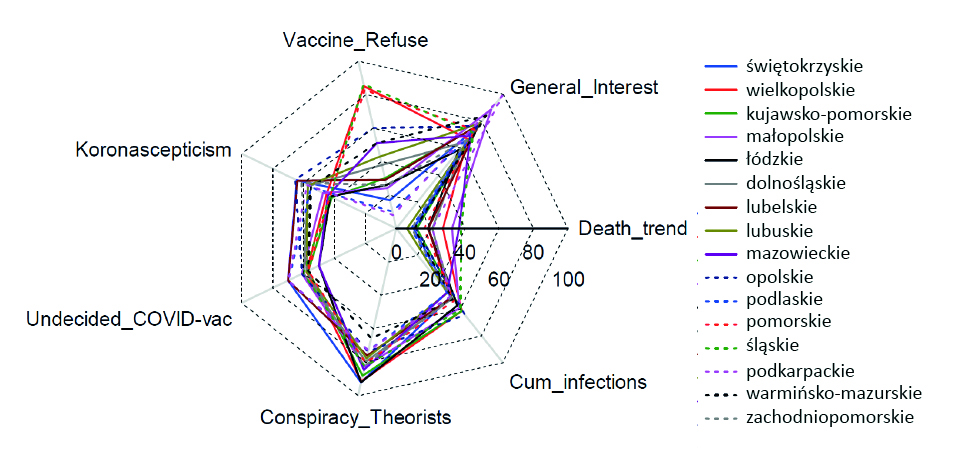
Figure 2. Radar graph of 7 chosen socio-epidemiological dimensions potentially related to willingness to COVID-19 vaccine uptake for the 16 Polish voivodeships
Discussion
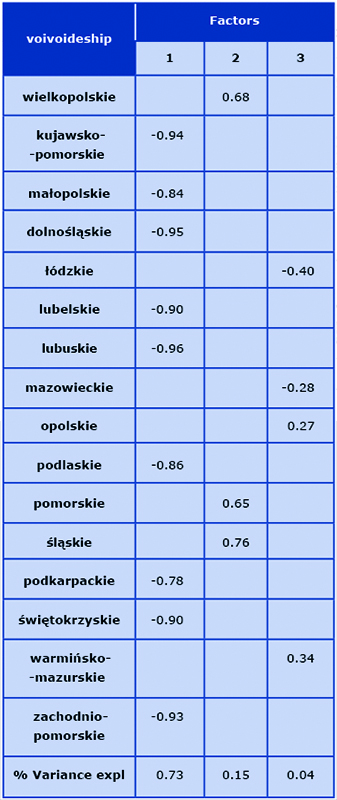
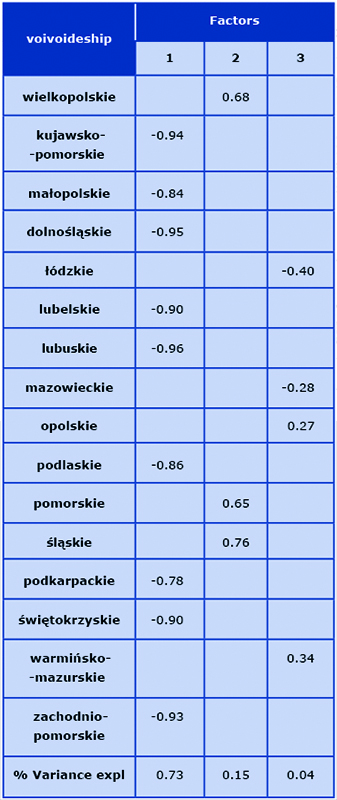
We attempt to systematize geographical diversity by factor analysis. In this simplified approach we do not assume any weights and all 7 dimensions are considered as equal predictors of attitude towards COVID-19 vaccine.
Geographical differences (Tab. 1) could be utilized in a dedicated communication practice [45, 49]:
- Factor 1 – regions with a low potential for action but with a high rate of undecided people. Recommended communication strategy should consider improving the reach of campaigns with emotionally-oriented content referring to conformism and common good [50].
- Factor 2 – regions that can significantly engage in vaccination refusal (high potential for action and high interest in conspiracy theories). Recommended communication strategy should emphasize individual profits [51] such as access to specific services and goods. Moderation of discussion in local traditional and social media could be considered for instance in Poznań, the Tricity [52] or in the górnośląskie agglomeration [53].
- Factor 3 – structurally heterogeneous vulnerable regions. Probably a separate strategy should be prepared for the Warsaw metropolitan area and the rest of mazowieckie. As usual, the opolskie Voivodeshipis difficult to classify due to its uniqueness [54].
Table 1. Factor loads estimated with minimum likelihood method (using Statistica 13)
It is important to mention that the proposed classification has partially revealed the socio-epidemiological structure of the regions, but a proper mix of qualitative and quantitative studies [55] should be conducted for each administrative unit to extensively explore the composition of subpopulations (Fig. 1) and the socio-epidemiological context (Fig. 2).
The issue of how to convince people to actually take the inoculum is very difficult and it requires the transfer of knowledge about audience profiling and content targeting from marketing research to public health. We showed that the simple rational and trust/information [41] deficit models alone could not easily explain vaccine hesitancy in Poland. This is just a preliminary and signalling study based on limited empirical data [56] and e.g. keywords selection in defining socio-epidemiological dimensions should be justified as the next step as well as Polish speaking Internet users are only a subset of the entire population. Vaccine discourse in core regions (factor 2), which tends to dominate due to a stronger political and economic position with a well-informed population knowing their civil rights, could be different to peripheral regions (factor 1), where counter-Enlightenment cultural and political initiative are more common [27]. However, based on this exploratory research, we can claim that the main responsibility should fall on the regional media and local governments (which on average acquire much higher trust than their national counterparts [57-58]) to prepare their own effective dissemination strategy. Especially during the first wave of COVID-19, local media (at least in dolnośląskie) broadcasted more reliable and less polarized information on coronavirus-related issues [59], in comparison with the nationwide media. Moreover, during the pandemic, central governmental agencies and the main players from the opposition parties are known to distribute fake news and manipulate the public by using sociotechnics, which is probably due to short-term political profits [59-60]. Thus, significant funds and responsibilities should be assigned to 16 voivodeships (NUTS-2) or even better to 380 poviats (NUTS-4) to prepare regional communication strategies in collaboration with local traditional and social journalists. Due to possible inequalities in organizational capital among regions, support from central institutions, think tanks and research centers could be required. Example of misclassification of mazowieckie (Table 1) suggests that even voivodeship could be too heterogeneous and deeper geographical mapping would be preferred (however it could be too difficult for logistical reasons in some less organized counties).
Nevertheless, our approach is only a local adaptation of the main information management pillars concerning COVID-19 vaccine [61-62], such as:
- accurate and timely knowledge transition on actual vaccine effectiveness (on individual and herd level) and safety, which must reach citizens and be understood by them;
- infoveillance of traditional and social media to monitor behavioral attitudes in all parts of the given society (Fig. 2);
- building (e)Health literacy, tailoring advice and messages to address various audiences (Fig. 1);
- controlling and improving knowledge propagation (e.g. fact checking), strategic partnerships should be formed across all local and central stakeholders.
Conclusions
To conclude, only local authorities and researchers who have the knowledge of their society [63-64] and communities with special needs as elderly [65-67], could deliver information in appropriate form and content [68]. Safe and effective vaccines do not only help the inoculated people (efficacy confirmed in multiple RCT), but their primary role should be stopping the spread of SARS-CoV-2 (if proved in observational studies or clinical trials). The theoretical effect of vaccination seems to be super-linear [69], so higher vaccine coverage could mean ever more QALYs (quality-adjusted life years) saved due to infections in the local population, as long as the proper balance in delivery among essential workers and high-risk groups in the first phase is satisfied. Thus, regionalized marketing could synergize with national [1, 41, 70] and pan-European [71] evidence-based platforms on benefit- -risk disseminations for vaccines and further candidates, while the first person was vaccinated against COVID-19 in Poland on 27 XII 2020.
Acknowledgements
The authors would like to thank students from the Scientific Circle of Health Promotion at the Wrocław Medical University for coding COVID-19 vaccine-related media releases from Dolnośląskie as well as Karolina Czopek and the NCN (2016/22/E/HS2/00034) from the Warsaw University for the hardware, software licence and sociolingistic support. The dataset is available at: https://ejtcm.gumed.edu.pl/articles/134674
Attachments
References
| 1. |
Narodowy Program Szczepień przeciw COVID-19 [in Polish] [Internet]. Ministerstwo Zdrowia. 2020 [cited 2020 Dec 11]. p. 1–34. Available from: https://www.gov.pl/attachment/0061e723-fc8c-4f79-8d7b-e33ab58181a8.
|
| 2. |
Adel Ali K, Brolin K, Funke S, Johansen K, Nicolay N, Olsson K, et al. Overview of COVID-19 vaccination strategies and vaccine deployment plans in the EU/EEA and the UK / ECDC Technical Report [Internet]. 2020. Available from: https://www.ecdc.europa.eu/en/publications-data/overview-current-eu-eea-uk-plans-covid-19-vaccines.
|
| 3. |
Lazarus J V, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med [Internet]. 2021 Feb 20;27(2):225–8. Available from: https://doi.org/10.1038/s41591-020-1124-9.
|
| 4. |
Call for Action: Managing the Infodemic. A global movement to promote access to health information and mitigate harm from health misinformation among online and offline communities / WHO [Internet]. 2020 [cited 2020 Dec 11]. Available from: https://www.who.int/news/item/11-12-2020-call-for-action-managing-the-infodemic.
|
| 5. |
Stosunek do szczepień przeciw COVID-19 [in Polish] [Internet]. CBOS News. [cited 2021 Apr 21]. Available from: https://www.cbos.pl/PL/publikacje/news/2020/41/newsletter.php.
|
| 6. |
Zygiel A. Sondaż dla RMF FM i ‘DGP’: Połowa Polaków nie chce szczepić się przeciwko koronawirusowi [in Polish] [Internet]. RMF 24. 2020 [cited 2020 Dec 11]. Available from: https://www.rmf24.pl/raporty/raport-koronawirus-z-chin/polska/news-sondaz-dla-rmf-fm-i-dgp-polowa-polakow-nie-chce-szczepic-sie,nId,4861072.
|
| 7. |
Morawiecki: za pomocą szczepień ‘chcemy osiągnąć jedno’ [video in Polish] [Internet]. TVN24; 2020. Available from: https://tvn24.pl/polska/szczepienia-na-covid-19-premier-mateusz-morawiecki-nikogo-nie-bedziemy-zmuszac-do-szczepien-za-ich-pomoca-chcemy-ochronic-przed-wirusem-polakow-4767685.
|
| 8. |
Ponad połowa Polaków nie chce zaszczepić się przeciw koronawirusowi Sars-Cov2 [in Polish] [Internet]. ISB Zdrowie. 2020 [cited 2020 Dec 11]. Available from: https://www.isbzdrowie.pl/2020/11/ponad-polowa-polakow-nie-chce-zaszczepic-sie-przeciw-koronawirusowi-sars-cov2/.
|
| 9. |
Feleszko W, Lewulis P, Czarnecki A, Waszkiewicz P. Flattening the Curve of COVID-19 Vaccine Rejection — A Global Overview. SSRN Electron J [Internet]. 2020; Available from: https://www.ssrn.com/abstract=3631972.
|
| 10. |
The State of Vaccine Confidence in the EU: 2018 [Internet]. Vaccine Confidence Project. 2018 [cited 2020 Dec 11]. Available from: https://www.vaccineconfidence.org/research-feed/the-state-of-vaccine-confidence-in-the-eu-2018.
|
| 11. |
Jarynowski A, Wójta-Kempa M, Płatek D, Czopek K. Attempt to Understand Public Health Relevant Social Dimensions of COVID-19 Outbreak in Poland. Society Register [Internet], 2020 Apr;4(3):7-44. Available from: https://pressto.amu.edu.pl/index.php/sr/article/view/22533.
|
| 12. |
Boguszewski R, Makowska M, Podkowińska M. A Typology of Poles’ Attitudes toward COVID-19 during the First Wave of the Pandemic. Int J Environ Res Public Health [Internet]. 2021 Feb 19;18(4):2002. Available from: https://www.mdpi.com/1660-4601/18/4/2002.
|
| 13. |
MacDonald NE, Butler R, Dubé E. Addressing barriers to vaccine acceptance: an overview. Hum Vaccin Immunother [Internet]. 2018 Jan 2;14(1):218–24. Available from: https://doi.org/10.1080/21645515.2017.1394533.
|
| 14. |
Brown VJ. Risk Perception: It’s Personal. Environ Health Perspect [Internet]. 2014 Oct;122(10). Available from: https://ehp.niehs.nih.gov/doi/10.1289/ehp.122-A276.
|
| 15. |
Kuchar E, Ludwikowska K, Marciniak D, Szenborn L, Nitsch-Osuch A. Public Perception of the Risks Associated with Infectious Diseases in Poland: Ebola and Influenza and Their Impact on the Attitude to Vaccination. In: Pokorski M, editor. Respiratory System Diseases Advances in Experimental Medicine and Biology vol 980 [Internet]. Springer, Cham.; 2017. p. 27–36. Available from: http://link.springer.com/10.1007/5584_2016_207.
|
| 16. |
Odone A, Ferrari A, Spagnoli F, Visciarelli S, Shefer A, Pasquarella C, et al. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage. Hum Vaccin Immunother [Internet]. 2015 Jan;11(1):72–82. Available from: http://www.tandfonline.com/doi/abs/10.4161/hv.34313.
|
| 17. |
Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ. Strategies for addressing vaccine hesitancy – A systematic review. Vaccine [Internet]. 2015;33(34):4180–90. Available from: https://www.sciencedirect.com/science/article/pii/S0264410X15005046.
|
| 18. |
Jarynowski A, Wójta-Kempa M, Krzowski Ł. An attempt to optimize human resources allocation based on spatial diversity of COVID-19 cases in Poland. medRxiv [Internet]. 2020 Jan 1;2020.10.14.20090985. Available from: https://www.medrxiv.org/content/10.1101/2020.10.14.20090985v1.
|
| 19. |
Rogalski M. COVID-19 w Polsce [in Polish] [Internet]. 2020. Available from: http://bit.ly/covid19-poland.
|
| 20. |
Duplaga M. The Determinants of Conspiracy Beliefs Related to the COVID-19 Pandemic in a Nationally Representative Sample of Internet Users. Int J Environ Res Public Health [Internet]. 2020 Oct 26;17(21):7818. Available from: https://www.mdpi.com/1660-4601/17/21/7818.
|
| 21. |
Furman FM, Zgliczyński WS, Jankowski M, Baran T, Szumowski Ł, Pinkas J. The State of Vaccine Confidence in Poland: A 2019 Nationwide Cross-Sectional Survey. Int J Environ Res Public Health [Internet]. 2020 Jun 24;17(12):4565. Available from: https://www.mdpi.com/1660-4601/17/12/4565.
|
| 22. |
Kossowska M, Szwed P, Czarnek G. Ideology shapes trust in scientists and attitudes towards vaccines during the COVID-19 pandemic. PsyArxiv [Internet]. 2021 [cited 2021 Apr 21];[preprint]. Available from: https://psyarxiv.com/hcbmw/.
|
| 23. |
Włodarska A, Gujski M, Pinkas J, Raciborski F. The influence of socio-demographic characteristics on attitudes towards prophylactic vaccination in Poland. Int J Occup Med Environ Health [Internet]. 2021;34(1):121–32. Available from: https://doi.org/10.13075/ijomeh.1896.01671.
|
| 24. |
Jarynowski A. Empiryczne badania społeczne w Polsce istotne dla zdrowia publicznego i epidemiologii w kontekście COVID-19 [in Polish] [Internet]. IBI. 2020 [cited 2021 Apr 21]. Available from: http://interdisciplinary-research.eu/badania-epmiryczne-spoleczne-w-polsce-istotne-dla-zdrowia-publicznego-i-epidemiologii-w-kontekscie-covid-19.
|
| 25. |
Jarynowski A, Stochmal M, Maciejewski J. Przegląd i charakterystyka prowadzonych w Polsce badań na temat społecznych uwarunkowań epidemii COVID-19 w jej początkowej fazie [in Polish]. Bezpieczeństwo Obron Socjol [Internet]. 2020;(13/14):38–87. Available from: http://yadda.icm.edu.pl/yadda/element/bwmeta1.element.desklight-a8f411a3-64a8-4d36-a7d6-c02e1acb8489/c/A_Jarynowski_M_Stochnal_J_Maciejewski.pdf.
|
| 26. |
Krueger T. Epidemia covid-19: Analiza sytuacji biezacej i prognozy krotkoterminowe. 2020. Available from: https://mocos.pl/assets/images/reports/20200513/wroclaw/report_wroclaw_20200513.pdf.
|
| 27. |
Żuk P, Żuk P, Lisiewicz-Jakubaszko J. The anti-vaccine movement in Poland: The socio-cultural conditions of the opposition to vaccination and threats to public health. Vaccine [Internet]. 2019 Mar;37(11):1491–4. Available from: https://www.sciencedirect.com/science/article/pii/S0264410X19301586.
|
| 28. |
Ganczak M, Kalinowski P, Drozd-Dąbrowska M, Biesiada D, Dubiel P, Topczewska K, et al. School life and influenza immunization: A cross-sectional study on vaccination coverage and influencing determinants among Polish teachers. Vaccine [Internet]. 2020 Jul;38(34):5548–55. Available from: https://www.sciencedirect.com/science/article/pii/S0264410X19314471.
|
| 29. |
Ganczak M, Bielecki K, Drozd-Dąbrowska M, Topczewska K, Biesiada D, Molas-Biesiada A, et al. Vaccination concerns, beliefs and practices among Ukrainian migrants in Poland: a qualitative study. BMC Public Health [Internet]. 2021 Dec 7;21(1):93. Available from: https://doi.org/10.1186/s12889-020-10105-9.
|
| 30. |
Kraśnicka J, Krajewska-Kułak E, Klimaszewska K, Cybulski M, Guzowski A, Kowalewska B, et al. Mandatory and recommended vaccinations in Poland in the views of parents. Hum Vaccin Immunother [Internet]. 2018 Dec 2;14(12):2884–93. Available from: https://www.tandfonline.com/doi/full/10.1080/21645515.2018.1496766.
|
| 31. |
Lusawa A, Pinkas J, Zgliczyński WS, Mazurek M, Wierzba W. Nieprawdziwe informacje w zakresie szczepień ochronnych jako wyzwanie dla zdrowia publicznego [in Polish]. Zdr Publiczne i Zarządzanie [Internet]. 2019;17(1):40–5. Available from: https://www.ejournals.eu/Zdrowie-Publiczne-i-Zarzadzanie/2019/Tom-17-zeszyt-1/art/15353.
|
| 32. |
Cianciara D, Szmigiel A. Posting on „Nie szczepimy („We don’t vaccinate”) Internet forum. Przegl Epidemiol [Internet]. 2019;73(1):105–15. Available from: http://www.przeglepidemiol.pzh.gov.pl/files/peissues/PE_1_2019__calosc_NET_bez_okladki.pdf#page=105.
|
| 33. |
Kołłątaj B, Kołłątaj W, Karwat I, Sobieszczański J, Panasiuk L. Anti-vaccine movements – health care, ignorance or a diversion aimed at destabilizing the health situation? Part 2. Contemporary conditions for the functioning and development of anti-vaccination movements. Ann Agric Environ Med [Internet]. 2020 Dec 22;27(4):553–61. Available from: http://www.aaem.pl/Anti-vaccine-movements-health-care-ignorance-or-a-diversion-aimed-at-destabilizing,126014,0,2.html.
|
| 34. |
Żuk P, Żuk P. Right-wing populism in Poland and anti-vaccine myths on YouTube: Political and cultural threats to public health. Glob Public Health [Internet]. 2020 Jun 2;15(6):790–804. Available from: https://www.tandfonline.com/doi/full/10.1080/17441692.2020.1718733.
|
| 35. |
Jaroszewska K, Marciniak A, Gawlak M, Życińska K, Wardyn K, Nitsch-Osuch A. Postrzeganie aktywności ruchów antyszczepionkowych przez rodziców małych dzieci. Postępy Nauk Med [Internet]. 2014;27(9):617–21. Available from: http://31.186.81.235:8080/api/files/view/9236.pdf.
|
| 36. |
Kuchar E, Szenborn L. Postawy antyszczepionkowe i możliwości polemiki. Przew Lek GPs [Internet]. 13(5). Available from: https://www.termedia.pl/Postawy-antyszczepionkowe-i-mozliwosci-polemiki,8,15917,0,0.html.
|
| 37. |
Kardas P, Zasowska A, Dec J, Stachurska M. Reasons for low influenza vaccination coverage: crosssectional survey in Poland. Croat Med J [Internet]. 2011;52(2):126–33. Available from: https://hrcak.srce.hr/index.php?id_clanak_jezik=106365&show=clanak.
|
| 38. |
Czajka H, Czajka S, Biłas P, Pałka P, Jędrusik S, Czapkiewicz A. Who or What Influences the Individuals’ Decision-Making Process Regarding Vaccinations? Int J Environ Res Public Health [Internet]. 2020 Jun 21;17(12):4461. Available from: https://www.mdpi.com/1660-4601/17/12/4461.
|
| 39. |
Troszyński M, Bieliński J, Bukowska X, Iwińska K, Markowska B, Nowicka M, et al. Czas pandemii w polskich mediach społecznościowych / Collegium Civitas [in Polish] [Internet]. 2020. Available from: https://www.civitas.edu.pl/wp-content/uploads/2020/07/czas_pandemii_w_polskich_mediach_spolecznosciowych.pdf.
|
| 40. |
Krawczyk M, Mikulski K. COVID-19: Dezinformacja w polskiej cyberprzestrzeni / Instytut Kościuszki [in Polish] [Internet]. 2020. Available from: https://ik.org.pl/wp-content/uploads/raport_dezinformacja_pl_v3.pdf.
|
| 41. |
Rzymski P, Borkowski L, Drąg M, Flisiak R, Jemielity J, Krajewski J, et al. The Strategies to Support the COVID-19 Vaccination with Evidence-Based Communication and Tackling Misinformation. Vaccines [Internet]. 2021 Feb 1;9(2):109. Available from: https://www.mdpi.com/2076-393X/9/2/109.
|
| 42. |
Google Trends [Internet]. [cited 2020 Dec 8]. Available from: https://trends.google.com/trends/?geo=PL.
|
| 43. |
Shetty P. Experts concerned about vaccination backlash. Lancet [Internet]. 2010 Mar;375(9719):970–1. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673610604217.
|
| 44. |
Malinowski B, Redfield R. Magic, science and religion and other essays: Selected, and with an introduction by Robert Redfield. Illinois: The Free Press; 1948.
|
| 45. |
Luz PM, Nadanovsky P, Leask J. How heuristics and cognitive biases affect vaccination decisions. Cad Saude Publica [Internet]. 2020;36(suppl 2). Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2020001405006&tlng=en.
|
| 46. |
Jaka jest liczba uchyleń dotyczących szczepień obowiązkowych? [in Polish] [Internet]. Szczepienia info. 2020 [cited 2020 Dec 11]. Available from: https://szczepienia.pzh.gov.pl/faq/jaka-jest-liczba-uchylen-szczepien-obowiazkowych/.
|
| 47. |
Rogalska J, Augustynowicz E, Gzyl A, Stefanoff P. Postawy rodziców wobec szczepień ochronnych w Polsce / Parental attitudes towards childhood immunisations in Poland [in Polish]. Przegl Epidemiol [Internet]. 2010;64(1):91–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20499667.
|
| 48. |
Jarynowski A. Potencjał protestów w Polsce [in Polish] [Internet]. Infodemia Koronawirusa – Analiza polskiego Internetu. 2020. Available from: http://www.infodemia-koronawirusa.pl/potencjal-protestow-w-polsce/.
|
| 49. |
Braczkowska B, Kowalska M, Braczkowski R, Barański K. Determinants of vaccine hesitancy. Prz Epidemiol [Internet]. 2017;71:227–36. Available from: http://www.przeglepidemiol.pzh.gov.pl/files/peissues/PE_nr_2_2017_Caly_srodek_internet.pdf#page=75.
|
| 50. |
Voinson M, Billiard S, Alvergne A. Correction: Beyond Rational Decision-Making: Modelling the Influence of Cognitive Biases on the Dynamics of Vaccination Coverage. PLoS One [Internet]. 2016 Dec 1;11(12):e0167842. Available from: https://dx.plos.org/10.1371/journal.pone.0167842.
|
| 51. |
Maliszewski N. How Do People Resolve Conflict Between Implicit and Explicit Attitudes? Polish Psychol Bull [Internet]. 2011 Jan 1;42(1):36–45. Available from: http://journals.pan.pl/dlibra/publication/114612/edition/99665/content.
|
| 52. |
Szczupak M, Augustyniak T, Sikorska K. The avoidance of vaccinations among people aged 0-18 years in pomorskie voivodeship in 2000-2017. Przegl Epidemiol [Internet]. 2020;74(1):109–18. Available from: http://www.przeglepidemiol.pzh.gov.pl/pobierz-artykul?id=2309.
|
| 53. |
Hubicki L, Czech E, Kowalska M, Zejda JE. Szczepienia ochronne dzieci w rodzinach o różnym stanie społeczno-ekonomicznym w Bytomiu. Prz Epidemiol [Internet]. 2004;58(4):713–23. Available from: http://www.przeglepidemiol.pzh.gov.pl/szczepienia-ochronne-dzieci-w-rodzinach-o-roznym-stanie-spoleczno-ekonomicznym-w-bytomiu.
|
| 54. |
Kisielewicz D. Historyczne uwarunkowania odrębności regionu Śląska Opolskiego [in Polish]. Pogran Polish Borderl Stud [Internet]. 2015;3(1):7–18. Available from: https://depot.ceon.pl/bitstream/handle/123456789/14684/kisielewicz_t3n1.pdf?sequence=1&isAllowed=y.
|
| 55. |
Jarynowski A, Paradowski M, Buda A. Modelling communities and populations : An introduction to computational social science. Stud Metodol [Internet]. 2019;(39):123–52. Available from: http://repozytorium.amu.edu.pl:8080/bitstream/10593/25476/1/SM39_MT_Cz¦Ö%2BŤ¦ç6.pdf.
|
| 56. |
Szmuda T, Ali S, Özdemir C, Syed MT, Singh A, Hetzger TV, et al. Datasets and future research suggestions concerning the novel Coronavirus (COVID-19). Eur J Transl Clin Med [Internet]. 2020 Dec 3;3(2):80–5. Available from: https://ejtcm.gumed.edu.pl/articles/72.
|
| 57. |
Zaufanie społeczne / CBOS [in Polish]. Komun z Badań [Internet]. 2020;(43):1–16. Available from: https://www.cbos.pl/SPISKOM.POL/2020/K_043_20.PDF.
|
| 58. |
Newman N, Fletcher R, Schulz A, Andı S, Nielsen KR. Reuters Institute Digital News Report 2020 [Internet]. 2020. Available from: https://reutersinstitute.politics.ox.ac.uk/sites/default/files/2020-06/DNR_2020_FINAL.pdf.
|
| 59. |
Jarynowski A. Monitorowanie percepcji ryzyka Covid-19 na Dolnym Śląsku za pomocą analizy śladu cyfrowego w internecie 15.01-05.08.2020 [in Polish]. Wrocław: Instytut Badań Interdyscyplinarnych; 2020.
|
| 60. |
Komunikat ICM w związku z informacjami medialnymi dotyczącymi wpływu aktualnie trwających protestów na rozwój epidemii COVID-19 [Internet]. ICM. 2020. Available from: https://icm.edu.pl/blog/2020/11/03/komunikat-icm-zwiazku-informacjami-medialnymi-dotyczacymi-wplywu-aktualnie-trwajacych-protestow-rozwoj-epidemii-covid-19/.
|
| 61. |
Eysenbach G. How to Fight an Infodemic: The Four Pillars of Infodemic Management. J Med Internet Res [Internet]. 2020 Jun 29;22(6):e21820. Available from: http://www.jmir.org/2020/6/e21820/.
|
| 62. |
Tangcharoensathien V, Calleja N, Nguyen T, Purnat T, D’Agostino M, Garcia-Saiso S, et al. Framework for Managing the COVID-19 Infodemic: Methods and Results of an Online, Crowdsourced WHO Technical Consultation. J Med Internet Res [Internet]. 2020 Jun 26;22(6):e19659. Available from: http://www.jmir.org/2020/6/e19659/.
|
| 63. |
Andrzejak R. Zdrowie dla regionu [in Polish]. Wałbrzych: Wydawnictwo Uczelniane Państwowej Wyższej Szkoły Zawodowej im. Angelusa Silesiusa; 2015.
|
| 64. |
Ludwikowska KM, Biela M, Szenborn L. HPV vaccine acceptance and hesitancy – lessons learned during 8 years of regional HPV prophylaxis program in Wroclaw, Poland. Eur J Cancer Prev [Internet]. 2020 Jul 25;29(4):346–9. Available from: https://journals.lww.com/10.1097/CEJ.0000000000000556.
|
| 65. |
Mesjasz J, Skawina I. Współczesne wyzwania gerontologii.Człowiek w pełni – podejście holistyczne [in Polish] [Internet]. Łódź: Społeczna Akademia Nauk; 2019. Available from: http://monografie.san.edu.pl/wp-content/uploads/2020/03/SiM-85.pdf.
|
| 66. |
Ganczak M, Gil K, Korzeń M, Bażydło M. Coverage and Influencing Determinants of Influenza Vaccination in Elderly Patients in a Country with a Poor Vaccination Implementation. Int J Environ Res Public Health [Internet]. 2017 Jun 20;14(6):665. Available from: http://www.mdpi.com/1660-4601/14/6/665.
|
| 67. |
Nessler K, Krztoń-Królewiecka A, Chmielowiec T, Jarczewska D, Windak A. Determinants of influenza vaccination coverage rates among primary care patients in Krakow, Poland and the surrounding region. Vaccine [Internet]. 2014 Dec;32(52):7122–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X14014017.
|
| 68. |
Bispo Júnior JP, Morais MB. Participação comunitária no enfretamento da COVID-19: entre o utilitarismo e a justiça social. Cad Saude Publica [Internet]. 2020;36(8). Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2020000803001&tlng=pt.
|
| 69. |
Jarynowski A, Grabowski A. Modelowanie Epidemiologiczne Dedykowane Polsce [in Poland]. Portal CZM [Internet]. 2015;9(6):1–22. Available from: http://www.czm.mif.pg.gda.pl/wp-content/uploads/fam/publ/jarynowski2.pdf.
|
| 70. |
Stanowisko 7. zespołu ds. COVID-19 przy Prezesie PAN: Szczepienie jest jedynym racjonalnym wyborem, dzięki któremu będziemy mogli szybciej wyjść z pandemii [in Poland] [Internet]. 2020 [cited 2012 Dec 11]. Available from: https://informacje.pan.pl/index.php/informacje/materialy-dla-prasy/3210-stanowisko-7-zespolu-ds-covid-19-przy-prezesie-pan-szczepienie-jest-jedynym-racjonalnym-wyborem-dzieki-ktoremu-bedziemy-mogli-szybciej-wyjsc-z-pandemii.
|
| 71. |
Sturkenboom M, Bahri P, Chiucchiuini A, Grove Krause T, Hahné S, Khromava A, et al. Why we need more collaboration in Europe to enhance post-marketing surveillance of vaccines. Vaccine [Internet]. 2020 Dec;38:B1–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X19310023.
|