Abstract
Background
A late clip slippage from the previously properly secured cerebral aneurysm is rarely observed. To date these complications have not pooled and evaluated using systematic review methodology. The objective was to report factors attributed to the late slippage of the aneurysm clip in the postoperative period.
Material and methods
All causes of postoperative clip slippage were systematically reviewed and analysed according to PRISMA Individual Patient Data protocol. Medline (PubMed), Embase, Cochrane, ISI Web of Knowledge and Google Scholar were searched for all relevant cases.
Results
Systematic review of the literature yielded 105 original cases proving slipped clip in the postoperative period. The slipped clip caused bleeding in 53.8% of patients. The putative cause of clip slippage was provided in only 34.7% of the published cases. If a single clip was used, then complete clip slippage was noted more often (p=0.04). Multiple clipping and clip-wrapping techniques were postulated as ways to prevent postoperative clip slippage.
Conclusions
The reason for late slippage of the aneurysm clip remains unexplained by most authors. Based on systematic reviewing, the use of tandem of clips prevents their late migration off the aneurysm. Clipping with wrapping or use of a single clip reinforced by any wrapping material seems a more durable solution.
Citation
Szmuda T, Słoniewski P. Late postoperative slippage of the cerebral aneurysm clip. A systematic review and meta-analysis. Eur J Transl Clin Med. 2019;2(1):56-69Introduction
Postoperative clip slippage is a rarely observed complication. Authors attributed this complication to the application of a short clip, some alloy features or clip closing pressure [1,2]. Repetitive opening of the clip further reduces its closing forces [3–5]. Another factor is the so-called scissoring effect [6–9]. Various authors demonstrated the examples of late clip migration following seemingly successful operations [10–13]. Less than 1% of the postoperative angiograms show an insufficiently secured aneurysm or a rotated clip [14]. Authors demonstrated various techniques in order to avoid clip slippage, although their interests were focused on the particular operative environment. Hundreds of case reports that were never critically appraised. To date, cases of clip slippage have not been pooled and analysed using a validated systematic review methodology. We aimed to collect and summarize the existing literature about clip slippage phenomena using the reproducible and widely accepted PRISMA Statement methodology [15].
Methods and materials
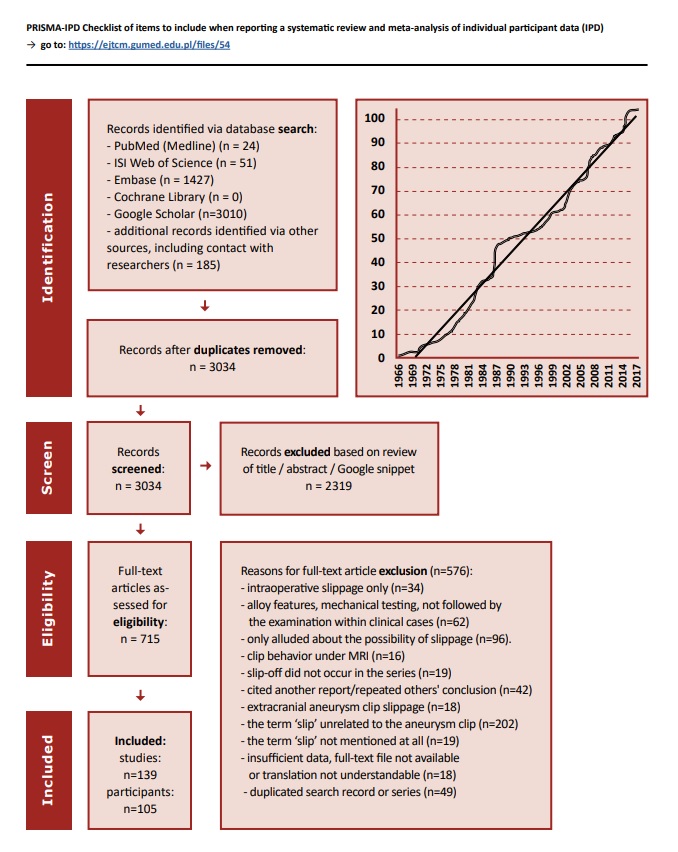
After reaching consensus, the authors developed a detailed protocol [16]. One author searched (November 2017), selected the articles and extracted data. Online Medline, Embase, Web of Knowledge, Cochrane and Google Scholar engines were queried for phrase: ‘aneurysm’ AND (‘clip’ OR ‘clipping’) AND (‘slip’ OR ‘slippage’). Duplicating records were removed using Mendeley Software (ver.1.17.10). Screening was based on titles and abstracts. We accepted original case reports, reviews, commentaries, expert opinions including animal, technical studies, PhD dissertations and patents. No limits in time of publication or language were applied. Google Translate website was used in case of abstracts and articles not in English. Following eligibility assessment, extensive searches for relevant references followed data extraction. Two types of data were deemed valid for further narrative synthesis of evidence: (1) descriptions of postoperative clip slippage and (2) intraoperative manoeuvres intended for prevention of a late slip-off phenomena. Raw data from each patient (Individual Participant Data method, IPD) were analysed as if all slippage occurrences belonged to an assumed single cohort. The evaluation was performed in accordance to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for IPD systematic reviews, which included search, eligibility, extraction, and reporting [17]. Publication bias was not assessed.
We used typical statistical methods for relevant comparisons: chi-square, t-test or Mann-Whitney U test. Probability value less than 0.05 was considered significant. Statistica v. 13.1 (StatSoft Co, Tulsa, OK; USA) and Prism (GraphPad Software, La Jolla, CA; USA) were used. IRB Committee in the institution of systematic reviews is exempt.
Results
The literature search yielded 3034 records, mostly identified via Google Scholar which explores full-texts for keywords. ‘Slip’ unrelated to cerebral aneurysm was the main exclusion criterion. Finally, 139 studies were included for the synthesis.
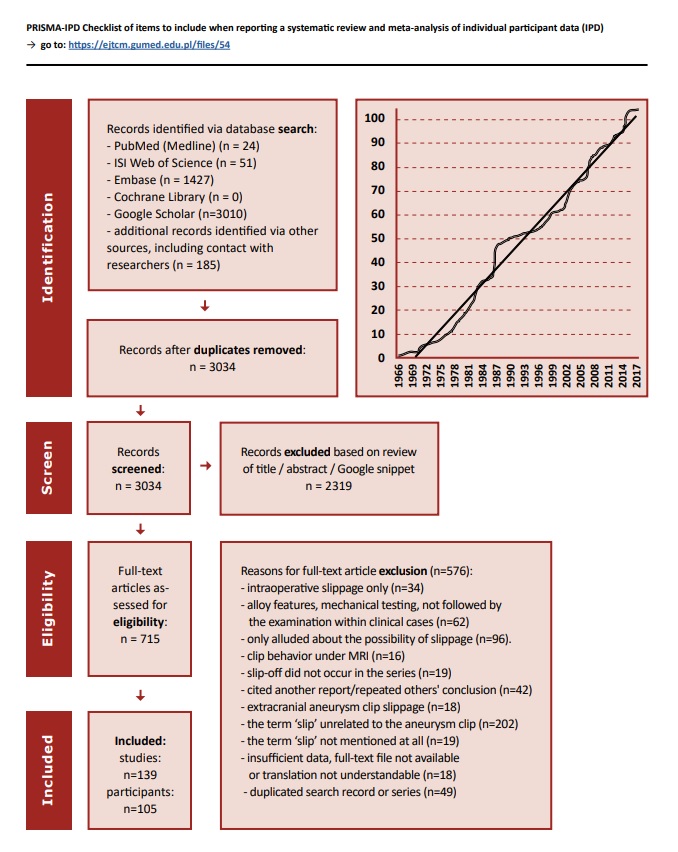
Fig. 1. Flowchart depicting the strategy for literature search. Cumulative number of cases involving aneurysm clip slippage. The graph demonstrates the constantly increasing publication rate on this subject.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097.
We found 105 original cases reporting late clip migration. In a half of the cases the slipped clip caused bleeding (53.8%; 43/80), half of which were fatal (23/43). A routine postoperative angiography revealed the incidental clip displacement in 32.5% of cases (26/80). Anterior communicating artery (n=15), internal carotid artery (n=21, including 2 blister-like), middle cerebral artery (n=12) and basilar artery (n=7) were commonly encountered locations. In majority of cases (65.3%; 62/95) the authors were not able to provide any reason for clip slippage. Others blamed the defect of clip material in 15 patients (16.0%) and persistent arterial pulsation in 6 (6.4%). Surprisingly, specific features of the particular aneurysm were attributed to only 5 cases of slipped clips (5.3%).
(Supplementary Table 1)
Download file with the Supplementary Table 1
Download file with the References to the Supplementary Table 1
The published reports rarely included aneurysm size, usually only if the aneurysm was giant (85.0%; 8/10). In a quarter of the slippage cases more than one clip was applied (23.3%; 10/43). In 82.9% of cases (68/80) a clip completely slipped off the aneurysm dome. Aneurysm location (p=0.65), size (p=0.26), rebleeding as the first symptom (p=0.65), fatal rebleeding (p=0.89) and occurrence in postoperative DSA (p=0.52) were not related to the degree (complete or incomplete) of clip migration. On the other hand, complete clip slip-off was significantly more often encountered if a single clip was used (82.1% vs. 44.4%, p=0.04). Regarding the direction of slip, in 87.5% of reports the clip migrated off the aneurysm (87.5%; 70/80), whereas in 8 cases (11.4%) the clip was displaced down onto the parent vessel, causing cerebral ischemia in 3 patents (37.5%).
Out of the 139 studies, 78 (56.1%) provided at least one suggestion on how to avoid late clip migration. The most commonly suggested method was placing several clips instead of one (15.8%; 24/139), followed by applying of clip-wrapping technique (7.2%p; 10/139) and performing DSA shortly after clipping (4.3%; 6/139). The suggested preventive methods were location-specific, e.g. in case of blood blister-like aneurysm authors postulated placing clips parallel to ICA or clip-wrapping.
Discussion
Our systematic review was divided into two stages: we pooled all valid cases in which an aneurysm clip slid off and collected all studies addressing prevention of clip slippage. By including every type of study into the systematic review, we intended to reveal case reports and authors’ own experiences. However, most authors (65.3%) did not provide any reason why the clip slipped off. The incomplete clipping and insufficient amount of used clips were the most commonly stated reasons. On the other hand, tandem clipping seems more durable option proposed by 15.8% of authors in our systematic review [9,18–20].
The prevention of clip slippage depended on aneurysm location. Specifically, reinforcing with any wrapping material, clip-wrapping methods and placing blades parallel to carotid were proposed in blood blister-like aneurysms [21–25]. Whereas in cases of a clip slipped from ACoA aneurysm, the authors did not provide any suggestions for repair.
Our systematic review pooled reports of slipped cerebral aneurysm clips. Based on this cohort we concluded that by using a single clip the surgeon should consider aneurysm recurrence. It was often speculated in the literature that multiple clipping more seems to be a more durable solution. Plenty of valuable hints on how to avoid postoperative clip slippage were suggested in the literature and we listed all of them based on the specific aneurysm location.
Ethical approval
Formal consent is not required for this type of study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
| 1. |
Drake CG, Peerless SJ, Hernesniemi JA. Surgery of Vertebrobasilar Aneurysms [Internet]. Vienna: Springer Vienna; 1996. Available from: http://link.springer.com/10.1007/978-3-7091-9409-6.
|
| 2. |
Giannotta SL. Complication A voidance for Large and Giant Carotid Ophthalmic Aneurysms. In. New Trends in Management of Cerebro-Vascular Malformations [Internet]. Pasqualin A, Da Pian R, editors. Vienna: Springer Vienna; 1994 [cited 2014 Sep 12]. 198-202 p. Available from: http://link.springer.com/10.1007/978-3-7091-9330-3.
|
| 3. |
Szmuda T, Słoniewski P. Giant Intracranial Aneurysms - Surgical Treatment, Accessory Techniques and Outcome. In: Murai Y, editor. Aneurysm [Internet]. InTech; 2012 [cited 2014 Sep 5]. p. 351–82. Available from: http://cdn.intechopen.com/pdfs-wm/38617.pdf.
|
| 4. |
Carvi y Nievas M, Höllerhage H. Risk of intraoperative aneurysm clip slippage: a new experience with titanium clips. J Neurosurg [Internet]. 2000 Mar [cited 2014 Sep 5];92(3):478–80. Available from: http://thejns.org/doi/abs/10.3171/jns.2000.92.3.0478.
|
| 5. |
Carvi y Nievas M. Assessment of the clipping efficacy of intracranial aneurysms: analysis of the employed methodology in relation to case difficulty. Neurol Res [Internet]. 2007 Jul [cited 2014 Sep 3];29(5):506–16. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17535574.
|
| 6. |
Horiuchi T, Li Y, Seguchi T, Sato A, Aoyama T, Hanaoka Y, et al. Clip blade scissoring with titanium bayonet clip in aneurysm surgery. Two case reports. Neurol Med Chir (Tokyo) [Internet]. 2012 [cited 2017 Nov 26];52(2):84–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22362289.
|
| 7. |
Kariyattil R, Panikar D. Scissoring of a Cobalt Alloy Aneurysm Clip causing Slippage during Cerebral Aneurysm Surgery: Case report and review of literature. Sultan Qaboos Univ Med J [Internet]. 2013 Feb [cited 2014 Sep 2];13(1):179–82. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3616789&tool=pmcentrez&rendertype=abstract.
|
| 8. |
Asgari S, Wanke I, Schoch B, Stolke D. Recurrent hemorrhage after initially complete occlusion of intracranial aneurysms. Neurosurg Rev [Internet]. 2003 Oct [cited 2014 Sep 2];26(4):269–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12802695.
|
| 9. |
Giannotta SL, Litofsky NS. Reoperative management of intracranial aneurysms. J Neurosurg [Internet]. 1995 Sep [cited 2014 Sep 2];83(3):387–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7666212.
|
| 10. |
McKissock W. Recurrence of an Intracranial Aneurysm after Excision. J Neurosurg [Internet]. 1965 Nov [cited 2017 Nov 26];23(5):547–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/5858447.
|
| 11. |
Kim YH, Kim JE, Kang H-S, Han DH. Migration of an aneurysm clip to the sacral subarachnoid space. Acta Neurochir (Wien) [Internet]. 2009 Mar 10 [cited 2014 Sep 2];151(6):699–700. Available from: http://www.scopus.com/inward/record.url?eid=2-s2.0-67650444427&partnerID=tZOtx3y1.
|
| 12. |
Oyesiku NM, Jones RK. Migration of a Heifetz aneurysm clip to the cauda equina causing lumbar radiculopathy. Case report. J Neurosurg [Internet]. 1986 Aug [cited 2014 Sep 5];65(2):256–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2941527.
|
| 13. |
Hayashi Y, Kimura M, Satake R, Kinoshita A. Possible participation of clip rotation in the formation of de novo aneurysm. J Clin Neurosci [Internet]. 2004 Apr [cited 2014 Sep 6];11(3):331–4. Available from: http://www.sciencedirect.com/science/article/pii/S0967586803001991.
|
| 14. |
Beltagy M El, Muroi C, Roth P, Fandino J, El Beltagy M, Imhof H-G, et al. Recurrent Intracranial Aneurysms After Successful Neck Clipping. World Neurosurg [Internet]. 2010 [cited 2014 Sep 5];74:472–7. Available from: http://www.sciencedirect.com/science/article/pii/S1878875010002846.
|
| 15. |
Szmuda T, Słoniewski P. Postoperative cerebral aneurysm clip slippage: systematic review. PROSPERO 2014 CRD42014013843 [Internet]. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=13843.
|
| 16. |
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med [Internet]. 2009 Jul 21 [cited 2014 Mar 20];6(7):e1000097. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2707599&tool=pmcentrez&rendertype=abstract.
|
| 17. |
Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, et al. Preferred Reporting Items for Systematic Review and Meta-Analyses of individual participant data: the PRISMA-IPD Statement. JAMA [Internet]. 2015 Apr 28 [cited 2016 Dec 27];313(16):1657–65. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2015.3656.
|
| 18. |
Wester K. Lessons learned by personal failures in aneurysm surgery: what went wrong, and why? Acta Neurochir (Wien) [Internet]. 2009 Sep [cited 2014 Sep 3];151(9):1013–24. Available from: http://www.scopus.com/inward/record.url?eid=2-s2.0-69249213985&partnerID=tZOtx3y1.
|
| 19. |
Park CK, Shin HS, Choi SK, Lee SH, Koh JS, Martin N. Clinical Analysis and Surgical Considerations of Atherosclerotic Cerebral Aneurysms: Experience of a Single Center. J Cerebrovasc Endovasc Neurosurg [Internet]. 2014 Sep 1 [cited 2017 Jul 10];16(3):247. Available from: https://synapse.koreamed.org/DOIx.php?id=10.7461/jcen.2014.16.3.247.
|
| 20. |
Nakamura K, Kitabayashi M, Murata T. Clipping for Wide-necked Asymptomatic Unruptured Intracranial Aneurysm. Surg Cereb Stroke [Internet]. 2012 Mar 19 [cited 2014 Sep 7];40(4):251–6. Available from: https://www.jstage.jst.go.jp/article/scs/40/4/40_251/_article.
|
| 21. |
Fujioka S. clipping on wrapping method for treatment of short aneurysms. Surg Cereb Stroke [Internet]. 2003 [cited 2014 Sep 4];31:375–9. Available from: http://jlc.jst.go.jp/JST.JSTAGE/scs/31.375?from=Google.
|
| 22. |
Shigeta H, Kyoshima K, Nakagawa F, Kobayashi S. Dorsal internal carotid artery aneurysms with special reference to angiographic presentation and surgical management. Acta Neurochir (Wien). 1992;119(1–4):42–8.
|
| 23. |
Yoshimoto Y, Ochiai C, Nagai M. Cerebral aneurysms unrelated to arterial bifurcations. Acta Neurochir (Wien). 1996;138(8):958–63.
|
| 24. |
Mooney MA, Kalani MYS, Nakaji P, Albuquerque FC, McDougall CG, Spetzler RF, et al. Long-term Patient Outcomes After Microsurgical Treatment of Blister-Like Aneurysms of the Basilar Artery. Neurosurgery [Internet]. 2015 Sep [cited 2016 Dec 27];11 Suppl 3:387–93. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00006123-201509001-00005.
|
| 25. |
Brown MA, Guandique CF, Parish J, McMillan AC, Lehnert S, Mansour N, et al. Long-term follow-up analysis of microsurgical clip ligation and endovascular coil embolization for dorsal wall blister aneurysms of the internal carotid artery. J Clin Neurosci [Internet]. 2017 May [cited 2017 Nov 26];39:72–7. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0967586816309419.
|