Abstract
Background: Fetal growth restriction (FGR) is a multifactorial disturbance of fetal nutrition with short- and long- -term consequences (e.g. autonomic malfunction and delayed neurological maturation). Fetal heart rate variability (HRV) is critically dependent on autonomic regulation. This study focused on identifying a correlation between neonatal biometry and HRV variables.
Material and methods: This was a descriptive cross-sectional study of 48 women at 22-36 weeks of pregnancy. The fetal cardiac signals were obtained from the maternal abdominal wall via non-invasive fetal electrocardiography (NI-FECG). The stress index (SI) was selected for evaluation among all linear HRV variables. Cardiotocographic parameters (short-term variation (STV) and long-term variation (LTV)) were determined, along with cardiographic: AC (acceleration capacity) and DC (deceleration capacity).
Results: FGR was detected in 9 women. The fetal growth was appropriate in 31 patients. 8 patients were excluded from the study. The detected variables of HRV in FGR were different, however statistical significance was impossible to determine (small number of cases). A strong linear correlation was detected between all the HRV variables: AC, DC, SI, STV, and LTV. Whereas, AC and DC had significant correlation with the 1-minute Apgar score. Multivariate regression analysis showed a statistically significant correlation of SI with the gestational age at birth.
Conclusions: SI could be of use in the advancement of conventional FGR management and has potential for further research.
Citation
Lakhno I V. Exploring the relationship between fetal growth restriction and heart rate variability parameters. Eur J Transl Clin Med. 2025;8(2):9-16Introduction
Fetal growth restriction (FGR) has short-term and longterm consequences on fetal and neonatal health and neurodevelopment. The fluctuations of fetal hemodynamics known as heart rate variability (HRV) reflect the fetus’s ability to support nutrition and well-being. The HRV level is critically dependent on autonomic regulation [1]. The autonomic malfunction was found in FGR and reflected the delayed neurological maturation in growth-restricted fetuses [2].
Ultrasonography is the gold standard for FGR diagnosis [3]. However, several studies found that HRV variables were possible predictors of FGR [4-6] Studies performed over last decade revealed the potential for ultrasonic cardiotocographic (CTG) assessment of fetal heart rate fluctuations in low-resource settings [7]. The use of fetal HRV in fetal growth assessment was demonstrated. However, ultrasound is not neutral for the fetus, therefore it could not be used for continuous Holter monitoring. CTG is a mechanical reflection of cardiac rhythm, but not the initial fluctuations in myocardium. Non-invasive fetal electrocardiography (NI-FECG) is a potential technique for obtaining cardiac signals through the maternal abdominal wall. There are some challenges associated with low signalto-noise ratio [8]. This method was found to be an alternative for cardiotocography anterpartum and during labor [9]. Systems for remote monitoring of fetal HRV via NI-FECG could be a good option for low-resource settings. This technique does not incur any major expense and helps calculate several sensitive parameters of fetal distress. Remote monitoring is appropriate during wartime [10].
NI-FECG captures primary electrophysiological processes in the heart. The variations in the duration of cardiac cycles reflect the continual changes in sympathovagal balance. Nowadays, both linear and non-linear methods are used to proceed with HRV. Some of them refer to sympathetic or parasympathetic regulation. The growing fetus demonstrates increased HRV in the process of neurological maturation. The known marker of fetal neurological maturation is reactivity to its motile activity in a non-stress test. Autonomic regulation is disturbed in fetal deterioration. Abnormally increased sympathetic tone is a marker of fetal compromise. Stress index (SI) is an integrative variable that expresses the load on regulatory systems influenced by the sympathetic branch of the autonomic function. Reflecting the central sympathetic circuit of hemodynamic regulation, SI is one of the most sensitive variables of sympathetic activity [2, 11]. The phase rectified signal averaging – acceleration capacity and deceleration capacity (AC/DC) are useful in the assessment of fetal well-being [12]. The technique for AC/DC calculation is dependent on RR extraction in NI-FECG and is a sensitive marker for fetal deterioration detected in long- or short-term recordings. Several parameters were obtained from CTG (Daws-Redman criteria) – short-term variations (STV) and long-term variations (LTV). They are very familiar and known to be useful in diagnosing fetal distress in the event of a nonreactive non-stress test [13]. This research was motivated by the speculation of decreased autonomic regulation in FGR. Probably, the pathological fetal environment reflecting abnormal HRV variables causes insufficient fetal growth. This study focused on detecting the correlation between neonatal biometry parameters and HRV variables.
Material and methods
This descriptive cross-sectional study was performed among pregnant women who were admitted to Kharkiv Municipal Perinatal Center between 1 April 2024 and 30 June 2024. The data were obtained from the hospital records system. Ethics approval was received from the Research Council and Ethical Committee of Kharkiv National Medical University (No. 25.0224p). Informed consent was obtained from all the patients. Patients from the Department of Maternal- -Fetal Medicine were selected at random, using the automated numbers technique. FGR was diagnosed in case fetal weight was lower than the 10th percentile according to ultrasound. The ultrasonic investigations were performed longitudinally following current clinical protocols [14]. Inclusion criteria were: healthy pregnancy with appropriate fetal growth, FGR. Whereas the exclusion criteria were: chromosomal abnormalities, multiple pregnancy, possible preterm birth, pre-eclampsia, gestational diabetes mellitus, pre-existing medical disorders (e.g. diabetes mellitus, metabolic syndrome, cardiac diseases, renal disease, thyrotoxicosis).
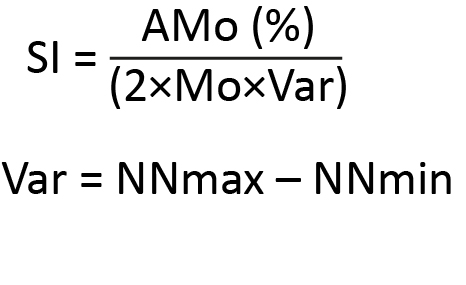
All of the fetal HRV variables were obtained from an RR-interval time series recorded from the maternal abdominal wall via the Cardiolab Baby Card NI-FECG device (XAI Medica, Kharkiv, Ukraine). The recordings lasted 30-60 minutes. The SI was selected for evaluation among all linear HRV variables and calculated according to the formula below.
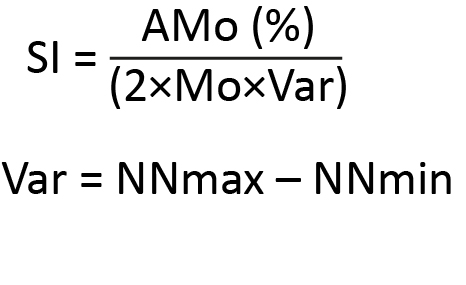
AMo (the most frequent NN interval value or the highest column in the histogram) – the number of NN intervals included in the pocket corresponding to the mode measured in percentages (%).
The obtained fetal RR interval time series was transformed into a cardiotocographic (CTG) tracing and the following CTG parameters were determined: short-term variation (STV) and long-term variation (LTV). The AC/DC variables were also detected [15]. All recordings were performed while the patients were resting in a recumbent position after eating. The study protocol also included recording several other parameters: gestational age at the time of investigation of HRV, gestational age at birth, neonatal biometry at birth (neonate’s body weight (gram), body length (sm), head circumference (sm)) and 1-minute Apgar score.
The Statistical Package for Social Sciences (SPSS) program (version 25.0., IBM Corp., Armonk, USA) was used for statistical analysis. The results were presented as means and standard deviations for numerical variables, whereas for categorical data as frequencies and percentages. The relation of the numerical variables to normal distribution was evaluated using skewness values and histograms. An independent sample t-test was used to compare the numerical variables that matched normal distribution. Variables that did not conform to normal distribution were analysed with the Mann-Whitney U test. The Chi-Square (or Fisher’s exact) test was used for comparing categorical variables. Depending on their distribution, Spearman or Pearson correlation analysis was used to assess the correlations between numerical variables. For multivariate examinations, a logistic regression analysis with the entered model was used. Sample size was calculated using confidence level 95% and margin of error 5%. A p-value of < 0.05 was considered statistically significant.
Results
A total of 48 females at 22-36 weeks of pregnancy were enrolled. FGR was detected in 9 patients. The fetal growth was appropriate in 31 patients. 8 patients were excluded from the study due to diagnosis of gestational diabetes mellitus (3 cases), severe pre-eclampsia (3 cases), and potential preterm birth (2 cases). The average age of the patients in the study cohort was 24.1 ± 6.8 years and the mean body mass index was 26.5 ± 7.2 (units). NI-FECG tracing was successfully recorded in 100.0% of the patients. The detected variables in the FGR were different (Table 1). However, the number of patients was too small to determine statistical significance. The gestational age at investigation, AC, DC, STV, LTV, gestational age at birth, body weight, body length, head circumference, and Apgar score were lower in patients with FGR. SI was higher in growth-restricted fetuses.
Table 2 shows a significant or moderate correlation between the gestational age at investigation and all other parameters: AC (r = 0.44; p = 0.005), DC (r = 0.43; p = 0.006), SI (r = -0.44; p = 0.004), STV (r = 0.47; p = 0.002), LTV (r = 0.51; p = 0.001), gestational age at birth (r = 0.34; p = 0.029), body weight (r = 0.34; p = 0.033), body length (r = 0.4; p = 0.011); head circumference (r = 0.4; p = 0.011), and the Apgar score (r = 0.46; p = 0.03). A strong or moderate correlation was detected between all the HRV variables: AC, DC, SI, STV, and LTV. AC and DC both demonstrated a significant correlation with the 1-minute Apgar score. However, no correlation was found between HRV variables and neonatal biometry at birth.
Table 1. Descriptive statistics of the variablesin the study cohort
AC – acceleration capacity; DC – deceleration capacity; LTV – long-term variations; SD – standard deviation; SI – stess index;
STV – short-term variation
Table 2. The correlation and significance between the detected variables in the study cohort
AC – acceleration capacity; DC – deceleration capacity; LTV – long-term variations; SI – stess index; STV – short-term variation
Table 3. Multivariate logistic regression model with SI coefficient
AC – acceleration capacity; DC – deceleration capacity; LTV – long-term variations; STV – short-term variations
Discussion
These results showed a linear correlation between gestational age and fetal HRV, and the link between SI and gestational age at birth following logistic regression parameters. The linear correlation showed similarities and mutual origin between AC, DC, SI, STV, and LTV. Correlations were found between AC and Apgar score, as well as DC and Apgar score, demonstrating the usefulness of these variables in diagnosing fetal distress. However, the linear correlation did not provide evidence of a potential connection between fetal HRV and neonatal biometry parameters. This outcome may have been influenced by the significant time interval between fetal NI-FECG recording and the time of birth. Probably, fetal HRV reflected environmental conditions responsible for fetal growth, maturation, and well-being during and after recording. Since the non-stress test performed via CTG has no predictive value, the prognostic ability of NI-FECG is of interest [16]. The relationships between fetal growth and maturation throughout gestation were clearer. The verification of a possible link with body length and head circumference requires further study on a larger cohort. This suggests that this temporal HRV index may be associated with the anthropometric parameters of newborns.
FGR is a multifactorial disturbance of fetal nutrition causing short- and long-term consequences. Severe maternal comorbidities or gestational complications were not included in this study. Such methodology helped determine the relations between fetal HRV and growth without any repercussions from maternal autonomic dysfunction. However, the aetiological reason for FGR is still under question or undetermined in the majority of cases. Idiopathic FGR is associated with placental disorders [17]. Therefore, screening for FGR is a key point in the management of patients. The humanitarian crisis caused by armed conflict necessitates the use of low-resource techniques. During armed conflict, access to obstetric care can be limited (e.g. due to the urgent need to relocate or to stay in a bomb shelter), thus increasing the need for reliable wireless fetal monitoring technologies. Our results demonstrated a certain potential for NI-FECG in measuring fetal growth, further research involving a larger study cohort is required. This technique could promote better wireless monitoring in the event of fetal arrhythmia or any suspicion of fetal deterioration.
The generalizability of this study is limited by the small number of observed FGR cases. Lower gestational age at birth in FGR was to be expected. The long time interval between NI-FECG and delivery could be also a limitation for this research. In addition, the findings were not corroborated by repeating NI-FECG prior to delivery. Receiver operating characteristic analysis could be the next stage in investigating efficient diagnostic algorithms based on fetal NI-FECG. Since FGR is a model for the study of fetal programming, the investigation of fetal autonomic maldevelopment could help to create novel antenatal markers for the diseases of adulthood. FGR is associated with an increased rate of cardiac abnormalities and arrhythmia. The systems based on NI-FECG can improve wireless fetal monitoring [2, 18].
Conclusions
SI demonstrated a correlation with gestational age at birth. This variable could be of use in the advancement of conventional management of FGR and has potential for further research.
Acknowledgements
The author appreciates the help of the Staff of the Kharkiv Municipal Perinatal Center.
Conflict of interest
The author declares no conflict of interest.
Funding
The author declares that no financial support was received for this study.
Data availability
All data and materials are available from the author.
------------
Image source: DeepAI (public domain)
References
| 1. |
Frasch MG. Heart Rate Variability Code: Does It Exist and Can We Hack It? Bioengineering [Internet]. 2023 Jul 10;10(7):822. Available from: https://www.mdpi.com/2306-5354/10/7/822.
|
| 2. |
Hoyer D, Żebrowski J, Cysarz D, Gonçalves H, Pytlik A, Amorim-Costa C, et al. Monitoring fetal maturation—objectives, techniques and indices of autonomic function. Physiol Meas [Internet]. 2017 May 1;38(5):R61–88. Available from: https://iopscience.iop.org/article/10.1088/1361-6579/aa5fca.
|
| 3. |
Nardozza LMM, Caetano ACR, Zamarian ACP, Mazzola JB, Silva CP, Marçal VMG, et al. Fetal growth restriction: current knowledge. Arch Gynecol Obstet [Internet]. 2017 May 11;295(5):1061–77. Available from: http://link.springer.com/10.1007/s00404-017-4341-9.
|
| 4. |
Smith V, Nair A, Warty R, Sursas JA, da Silva Costa F, Wallace EM. A systematic review on the utility of non-invasive electrophysiological assessment in evaluating for intra uterine growth restriction. BMC Pregnancy Childbirth [Internet]. 2019 Dec 5;19(1):230. Available from: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-019-2357-9.
|
| 5. |
Zizzo AR, Hansen J, Petersen OB, Mølgaard H, Uldbjerg N, Kirkegaard I. Growth‐restricted human fetuses have preserved respiratory sinus arrhythmia but reduced heart rate variability estimates of vagal activity during quiescence. Physiol Rep [Internet]. 2022 Nov 21;10(22). Available from: https://physoc.onlinelibrary.wiley.com/doi/10.14814/phy2.15458.
|
| 6. |
Stroux L, Redman CW, Georgieva A, Payne SJ, Clifford GD. Doppler‐based fetal heart rate analysis markers for the detection of early intrauterine growth restriction. Acta Obstet Gynecol Scand [Internet]. 2017 Nov 27;96(11):1322–9. Available from: https://obgyn.onlinelibrary.wiley.com/doi/10.1111/aogs.13228.
|
| 7. |
Stroux L, Martinez B, Coyote Ixen E, King N, Hall-Clifford R, Rohloff P, et al. An mHealth monitoring system for traditional birth attendant-led antenatal risk assessment in rural Guatemala. J Med Eng Technol [Internet]. 2016 Nov 16;40(7–8):356–71. Available from: https://www.tandfonline.com/doi/full/10.1080/03091902.2016.1223196.
|
| 8. |
Odendaal HJ, Kieser E, Crockart IC, Brink LT, Du Plessis C, Nel DG. Clinical associations of fetal heart rate accelerations as derived from transabdominal fetal electrocardiograms. Eur J Obstet Gynecol Reprod Biol [Internet]. 2022 Dec;279:5–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0301211522005437.
|
| 9. |
Velayo CL, Funamoto K, Silao JNI, Kimura Y, Nicolaides K. Evaluation of Abdominal Fetal Electrocardiography in Early Intrauterine Growth Restriction. Front Physiol [Internet]. 2017 Jun 26;8. Available from: http://journal.frontiersin.org/article/10.3389/fphys.2017.00437/full.
|
| 10. |
Lakhno I. The Insight into Obstetric Care near the Front Line in Kharkiv. Acta medica Litu [Internet]. 2022 Sep 26;29(2):187–95. Available from: https://www.zurnalai.vu.lt/AML/article/view/28051.
|
| 11. |
Lakhno I. The Use of Fetal Noninvasive Electrocardiography. Scientifica (Cairo) [Internet]. 2016;2016:1–6. Available from: http://www.hindawi.com/journals/scientifica/2016/5386595/.
|
| 12. |
Stampalija T, Casati D, Monasta L, Sassi R, Rivolta M, Muggiasca M, et al. Brain sparing effect in growth‐restricted fetuses is associated with decreased cardiac acceleration and deceleration capacities: a case–control study. BJOG An Int J Obstet Gynaecol [Internet]. 2016 Nov 23;123(12):1947–54. Available from: https://obgyn.onlinelibrary.wiley.com/doi/10.1111/1471-0528.13607.
|
| 13. |
Hoyer D, Schmidt A, Gustafson KM, Lobmaier SM, Lakhno I, van Leeuwen P, et al. Heart rate variability categories of fluctuation amplitude and complexity: diagnostic markers of fetal development and its disturbances. Physiol Meas [Internet]. 2019 Jun 1;40(6):064002. Available from: https://iopscience.iop.org/article/10.1088/1361-6579/ab205f.
|
| 14. |
Leal CRV, Rezende KP, Macedo E do CP de, Rezende G de C, Corrêa Júnior MD. Comparison between Protocols for Management of Fetal Growth Restriction. Rev Bras Ginecol e Obs / RBGO Gynecol Obstet [Internet]. 2023 Feb 28;45(02):096–103. Available from: https://journalrbgo.org/article/comparison-between-protocols-for-management-of-fetal-growth-restriction/.
|
| 15. |
Ponsiglione AM, Cosentino C, Cesarelli G, Amato F, Romano M. A Comprehensive Review of Techniques for Processing and Analyzing Fetal Heart Rate Signals. Sensors [Internet]. 2021 Sep 13;21(18):6136. Available from: https://www.mdpi.com/1424-8220/21/18/6136.
|
| 16. |
Kapaya H, Jacques R, Anumba D. Comparison of diurnal variations, gestational age and gender related differences in fetal heart rate (FHR) parameters between appropriate-for-gestational-age (AGA) and small-for-gestational-age (SGA) fetuses in the home environment. Frasch MG, editor. PLoS One [Internet]. 2018 Mar 9;13(3):e0193908. Available from: https://dx.plos.org/10.1371/journal.pone.0193908.
|
| 17. |
Kingdom JC, Audette MC, Hobson SR, Windrim RC, Morgen E. A placenta clinic approach to the diagnosis and management of fetal growth restriction. Am J Obstet Gynecol [Internet]. 2018 Feb;218(2):S803–17. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0002937817323402.
|
| 18. |
Liu B, Ridder A, Smith V, Thilaganathan B, Bhide A. Feasibility of antenatal ambulatory fetal electrocardiography: a systematic review. J Matern Neonatal Med [Internet]. 2023 Dec 31;36(1). Available from: https://www.tandfonline.com/doi/full/10.1080/14767058.2023.2204390.
|