Improving quality of life of completely edentulous patient with oral submucous fibrosis and infantile hemangioma
Abstract
Background: Oral submucous fibrosis is a premalignant condition characterized by rigidity of lips, tongue, and buccal mucosa. It makes rehabilitation difficult as it affects the stability and retention of the prosthesis.
Description: This technical report focuses on the use of intralesional hyaluronidase injections followed by conventional complete denture fabrication for an edentulous patient. These conservative and non-invasive options were chosen due to the presence of infantile hemangioma in the region of interest.
Conclusion: Hyaluronidase injections in the area of oral submucous fibrosis can bring about a major difference in the process of rehabilitation and potentially eliminate the morbidity associated with the surgical procedures.
Citation
Singh S, Dhawan P, Kaur H, Bhargava M. Improving quality of life of completely edentulous patient with oral submucous fibrosis and infantile hemangioma. Eur J Transl Clin Med. 2025;8(1):113-118Background
Insidious oral submucous fibrosis (OSMF) is a chronic disorder marked by fibrosis of the submucosa (comprising the lamina propria and deeper connective tissues) and an inflammatory response [1]. It has a prevalence rate of 0.2 percent to 0.5 percent in Southeast Asia and the Indian subcontinent [2]. There are numerous causative factors, although the most common are consumption of areca (betel) nuts, chilli or other spices, genetic susceptibility, and nutritional deficiencies. The most commonly involved areas are buccal mucosa, palate, and sometimes the pharynx and faucial pillars. The signs and symptoms include burning sensation, referred pain in the temporal region, changes in salivation (increased or decreased), difficulty with chewing, phonation, and swallowing, reduced mouth opening, and ulceration of the mucosa [3].
Evidence suggests that OSMF is multifactorial, with certain effects on specific subpopulations of fibroblasts, genetic predisposition and molecular mechanisms (via cytokines and growth factors), which could render the oral mucosa more susceptible to chronic inflammatory changes on exposure to carcinogens. The chemical constituents of the areca nuts can stimulate fibroblast proliferation leading to collagen synthesis. Apart from this, these extracts also have the capability to stabilize the collagen fibrils and make it resistant to enzymatic degradation. It is noteworthy that the areca nuts have a higher copper content than the more commonly eaten nuts. The copper is released in the oral cavity while chewing the nut. Lysyl oxidase, an extracellular copper enzyme is secreted by fibroblasts and initiates post-transitional modification of collagen fibers rendering them resistant to the action of collagenases [1].
In clinical staging, early OSMF presents with stomatitis and vesiculation, moderate OSF has a marble-like appearance and palpable fibrous bands, and severe OSMF is manifested by leukoplakia and erythroplakia. Whereas the histological staging/classification is determined by the number and distribution of fibroblasts, collagen fibers, inflammatory cells and blood vessels. Moreover, biomarkers such as proteins, mRNAs, and non-coding RNAs are also measured in OSF staging and classification [2-3].
Nutritional support, microwave diathermy, immunomodulatory medications, physiotherapy, local drug delivery, combination therapy, and surgical excision of the fibrotic bands are among the various treatment options recommended to manage OSMF. Steroids act as immunosuppressive agents, decrease fibroblast proliferation, and release cellular protease in the connective tissue which stimulates collagenase and zymogen, which consume insoluble collagen [4]. Hyaluronidase breaks down the collagen fibers, dissolves the hyaluronic acid matrix, and lowers the thickness of intracellular cemental materials more quickly in OSMF patients. According to studies, hyaluronidase and intralesional steroid injections reduce the clinical symptoms of OSMF for a longer period of time [5].
Rehabilitation of a completely edentulous patient with OSMF is difficult. One of the options are the commonly chosen sectional complete dentures, although various challenges are related to the impression making, fabrication orientation of denture bases, and risk of losing the attachments. The other option is implant supported prosthesis which can provide predictable functional and esthetic outcomes. In this technical report we present a method of improving the mouth opening of a patient with OSMF by utilizing intralesional injections followed by conventional complete denture prosthesis.
Case Description
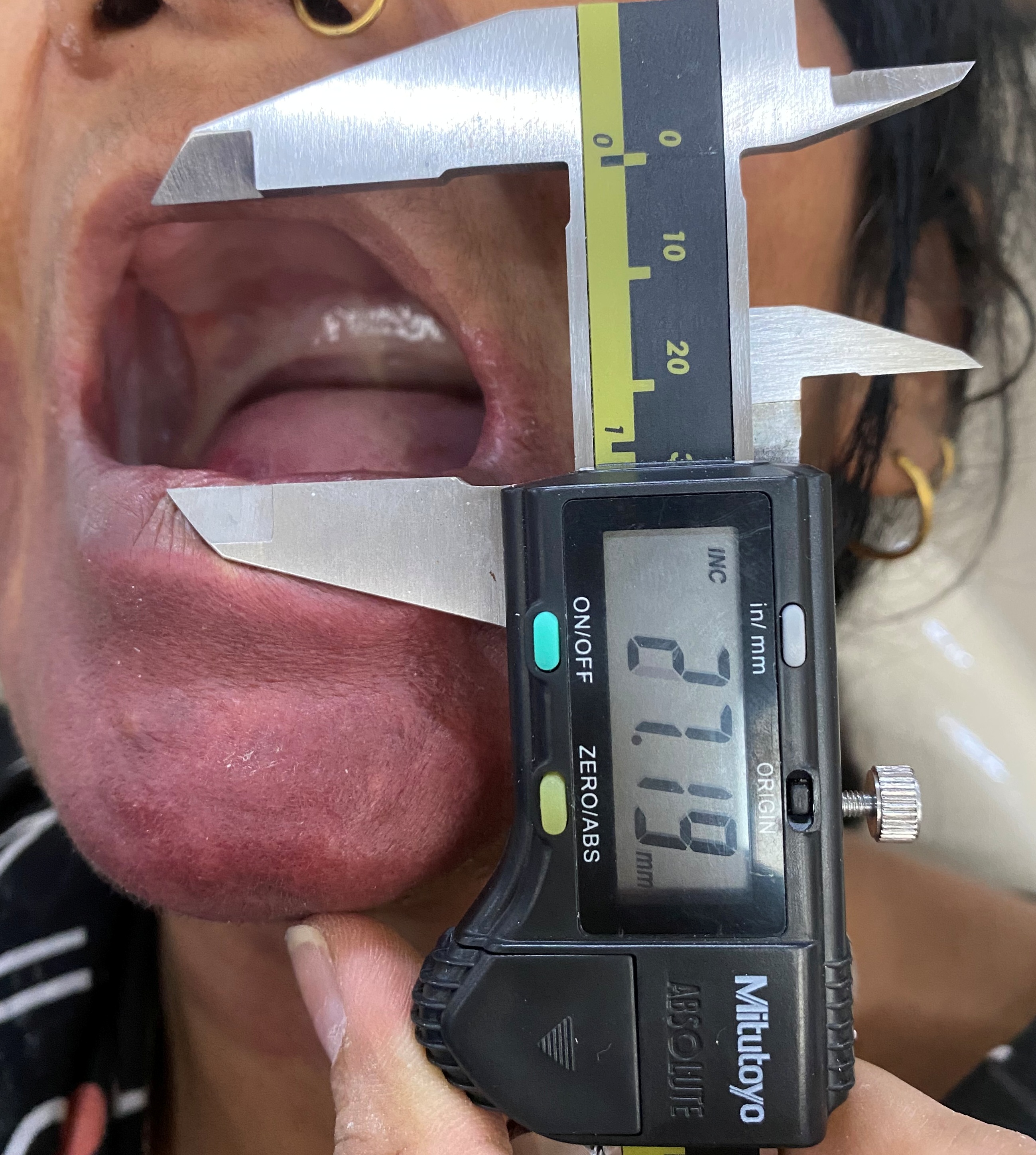
A 40-year-old female patient reported to the Department of Prosthodontics with a chief complaint of missing teeth and difficulty with chewing. The patient had a past medical history of infantile hemangioma and a 20-year history of chewing areca nuts. She complained of a burning sensation in her oral cavity and difficulty in opening the mouth. On physical examination, a pink to purple discoloration was seen, with undefined margins present on the chin and towards the cheek unilaterally (right side). The dimensions would be 6-7 cm super-inferiorly and 10-12 cm mesiodistally (Figure 1). Using a digital caliper the mouth opening was measured at 27.19 mm (Figure 2).

Figure 1. Extraoral congenital haemangioma
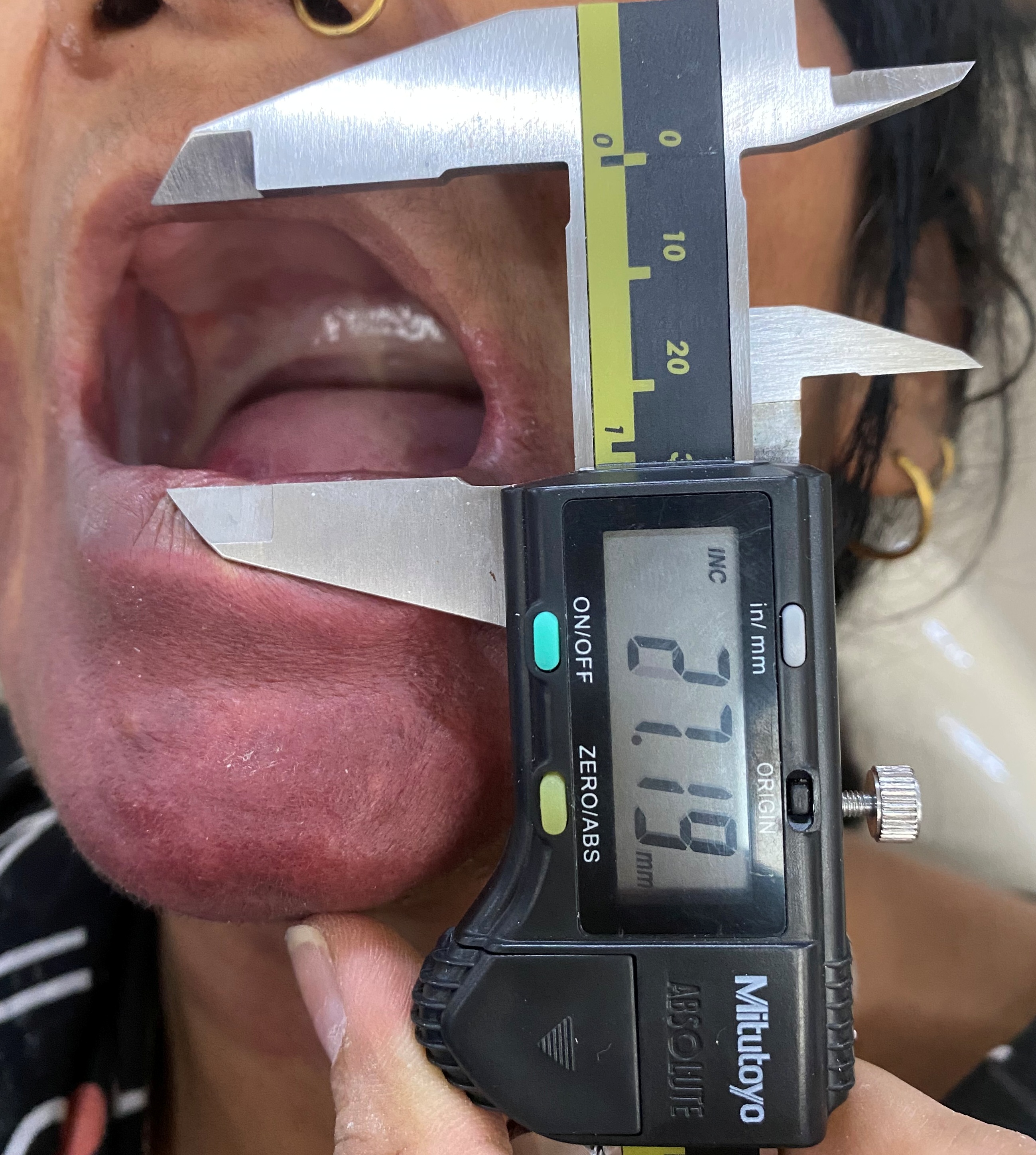
Figure 2. Restricted mouth opening upon initial physical examination
On intra-oral examination, diffused blanched white bands were seen bilaterally on the buccal mucosa in the molar region (Figure 3). The bands were taut and tough which led to a limited mouth opening. The hemangioma extended up to the buccal mucosa adjacent to the pre-molar region. There were completely edentulous maxillary and mandibular alveolar arches which had red discoloration on the mandibular anterior region due to the hemangioma present intraorally as well (Figure 4). Based on the physical examination and medical history, the patient was diagnosed with grade II OSMF.

Figure 3. Blanched white bands

Figure 4. Intraoral pink-red discoloration
Due to the infantile hemangioma, certain invasive procedures for improving the mouth opening (e.g. commisuroplasty) or rehabilitation of edentulous ridges (e.g. implant placement) were not appropriate. The mandibular implant supported overdenture is generally placed in the region between 2 mental foramina. In case of our patient, that area was completely covered with hemangioma, hence every surgical procedure was high risk for her. Furthermore, sectional dentures were also excluded because the thick bands present in the buccal mucosa can compromise retention and stability of the prosthesis.
We decided on pharmacological management of the patient, followed by a conventional complete denture. The mucosa was arbitrarily divided into 3 zones, and approximately equal amounts of hyaluronidase with 1 ml of 2% lidocaine and adrenaline (1:80000), were injected intralesionally (where the most fibrosis was felt on palpation) with a 28 gauge needle, twice weekly for 4 weeks (a total of 8 doses). The patient was instructed to avoid spicy food and the exercises to improve mouth opening were recommended. Transcutaneous electrical nerve stimulation (TENS) was patiensed as an adjunct to mouth opening exercises. The patient had an increase in mouth opening of 33 mm (Figure 5) and the buccal mucosa movement were easily performed. The complete denture prosthesis with balanced occlusion was fabricated conventionally (Figure 6). The patient was kept on regular follow-up after 24 hrs, 72 hrs, 1 month, 3 months, and 6 months.

Figure 5. Improved mouth opening
Figure 6. Complete denture in place
Discussion
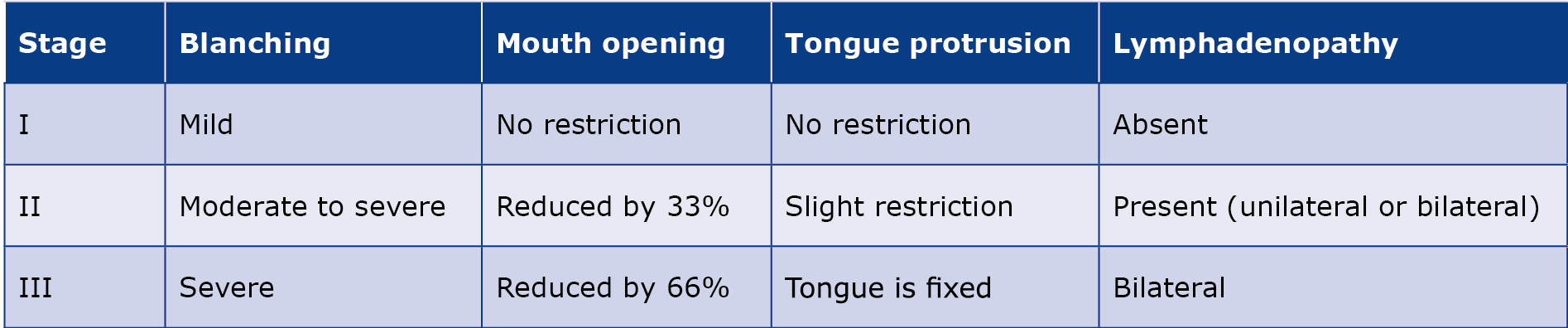
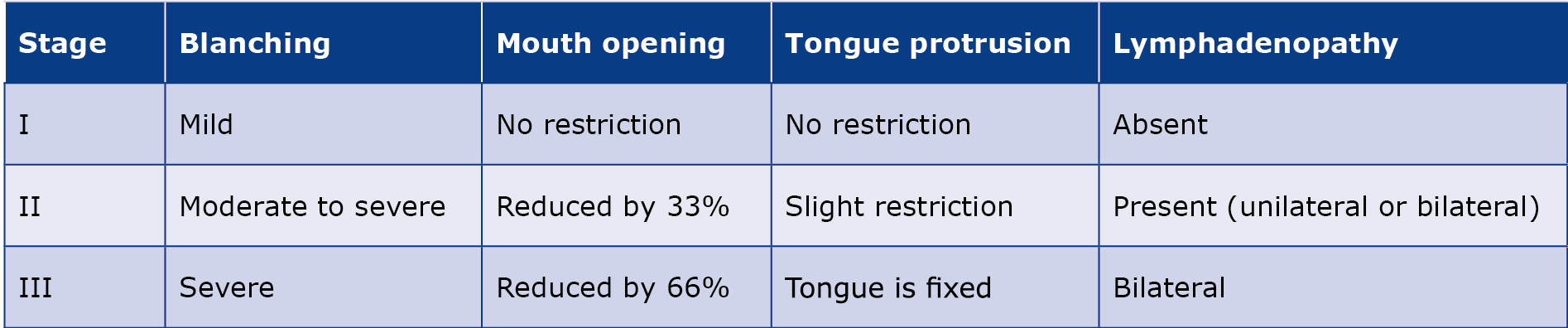
Based on clinical diagnosis, Nagesh and Bailoor [6] categorized OSMF into 3 stages [6] (Table 1). Unfortunately no such classification is available for edentulous patients. Hence, the treatment options to be implied for a particular stage of OSMF are also not specified. Symptomatic relief is provided by conservative methods (vitamins, topical steroids, physiotherapy and antioxidants) that have an anti-inflammatory effect and promote apoptosis. The most common OSMF treatment options are medical, surgical and physiotherapy [7]. Treatment modalities such as implant supported overdentures or sectional dentures are available. Furthermore, to improve the prosthetic outcome, neutral zone technique, intra-oral Gothic arch tracing and 3D printed denture bases can be used. How ever we did not consider the above-mentioned options due to our patient’s underlying condition of infantile hemangioma. Keeping the stability and retention of a sectional prosthesis is a difficult task for the patient and eventually leads to non-usage of the prosthesis and reduced quality of life.
Table 1. Stages of OSMF for the dentulous mouth based on clinical diagnosis (Nagesh and Bailoor) [6]
Steroids act by opposing the action of soluble factors generated by sensitized lymphocytes after activation by specific antigens. This results in anti-inflammatory and immunosuppressive activity and prevents fibrosis by decreasing fibroblastic proliferation and collagen deposition. The initial relief of OSMF symptoms may be due to anti-inflammatory action of steroids (e.g. dexamethasone), which clears the juxtaepithelial inflammation [3, 8]. By breaking down hyaluronic acid (the ground substance in connective tissue), hyaluronidase lowers the viscosity of intercellular cement substance. Better results were observed with respect to trismus and fibrosis.
Our patient achieved considerable improvement in mouth opening after 4 weeks of intra-lesional injections and TENS therapy. Post-treatment follow-up was conducted using Kapoor’s Index, which assesses the retention and stability of dentures. The retention and stability were satisfactory, indicating successful functional performance of the prosthesis (Figures 7-9). In addition to this, a thorough evaluation of the patient’s mouth opening was performed. The results showed that the achieved mouth opening after prosthetic rehabilitation was comparable to the outcomes typically observed following intra-lesional injection therapy, suggesting a favourable and functional result (Figure 10).



Figure 7-9. Complete denture in occlusion during follow-up appointments

Figure 10. Mouth opening at the 6 months follow-up visit
Kakar et al. reported that patients receiving hyaluronidase alone reported a quicker relief of symptoms, whereas combination with dexamethasone provided better long-term results [3]. Shah et al evaluated the efficacy of hyaluronidase and dexamethasone combination in the treatment of OSMF and reported a reduction of the burning sensation and an improvement in mouth opening [7].
Lanjekar et al. evaluated the efficacy of topical curcumin mucoadhesive semisolid gel, triamcinolone acetonide/hyaluronidase mucoadhesive semisolid gel and a combination of both in the treatment of oral submucous fibrosis (OSMF). They concluded that curcumin has a therapeutic effect on patients diagnosed with OSMF. Maximum utilization and enhanced drug delivery were achieved with the help of a combination other two active drugs, namely triamcinolone and hyaluronidase [3].
Bansal conducted a histopathological study to know the efficacy of local and systemic corticosteroid and hyaluronidase therapy in oral submucous fibrosis. The results of his study revealed that local and systemic corticosteroid and hyaluronidase therapy in patients with OSMF were found effective. However, histopathologically, it was not found statistically significant whether corticosteroids are given locally and/or systemic with or without injection hyaluronidase [10]. Although local corticosteroid injections are considered safe in patients with haemangiomas, we decided not to administer them due to the potential for adverse reactions. During treatment of children with local steroid injections it is suggested to routinely test endocrine/adrenal function and actively consult with an endocrinologist to confirm and then minimize the impact on the adrenal glands, growth and immune status [11].
Conclusion
Injections of hyaluronidase are an effective way to manage and eliminate morbidity in OSMF. The most notable effect of this treatment approach was an increase in mouth opening along with a decrease in a burning sensation. Also, it is a cost-effective method. Careful treatment planning and modification of conventional dentures allowed us to overcome the common clinical challenges of treating OSMF. Periodic recalling and prosthesis maintenance help with keeping the prosthesis stable, functional and easy to use.
Conflict of interests
None.
Funding
None.
References
| 1. |
Passi D, Bhanot P, Kacker D, Chahal D, Atri M, Panwar Y. Oral submucous fibrosis: Newer proposed classification with critical updates in pathogenesis and management strategies. Natl J Maxillofac Surg [Internet]. 2017;8(2):89. Available from: https://journals.lww.com/njms/fulltext/2017/08020/oral_submucous_fibrosis__newer_proposed.2.aspx.
|
| 2. |
Guna TP, Sathyanarayanan R, Pilavullathil R, Jude NJ, Kumaravel R, Selvakumar C, et al. Management of oral submucous fibrosis with intralesional injection of hyaluronidase and dexamethasone: a case report. J Sci Dent. 2020;10(2).
|
| 3. |
James L, Shetty A, Rishi D, Abraham M. Management of Oral Submucous Fibrosis with Injection of Hyaluronidase and Dexamethasone in Grade III Oral Submucous Fibrosis: A Retrospective Study. J Int Oral Heal JIOH [Internet]. 2015;7(8):82–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26464545.
|
| 4. |
Yadav A, Nair G, Naidu GS, Makkad RS, Nagi R, Dewangan G. Intralesional Steroid plus Hyaluronidase and Oral Physiotherapy in the management of Oral submucous fibrosis: Clinicians Experience. J Adv Med Dent Sci Res [Internet]. 2020;8(10):122–9. Available from: http://jamdsr.com/uploadfiles/28osmfvol8issue10pp122-129.20201016032628.pdf.
|
| 5. |
Kumari A, Roy S. Efficacy of Hyaluronidase in Management of OSMF-A Clinical Study. J Adv Med Dent Scie Res [Internet]. 2016;4(6):299–301. Available from: http://jamdsr.com/uploadfiles/73osmfvol4iss6p299-301.20190214091231.pdf.
|
| 6. |
Bhagvan More C, Gupta S, Joshi J, N Verma S. Classification System for Oral Submucous Fibrosis. Kailasam S, editor. J Indian Acad Oral Med Radiol [Internet]. 2012;24:24–9. Available from: http://www.jaypeejournals.com/eJournals/ShowText.aspx?ID=3032&Type=FREE&TYP=TOP&IN=~/eJournals/images/JPLOGO.gif&IID=235&isPDF=YES.
|
| 7. |
Shah PH, Venkatesh R, More CB, Vassandacoumara V. Comparison of Therapeutic Efficacy of Placental Extract with Dexamethasone and Hyaluronic Acid with Dexamethasone for Oral Submucous Fibrosis - A Retrospective Analysis. J Clin Diagn Res [Internet]. 2016;10(10):ZC63–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27891461.
|
| 8. |
Patel TL, Singh S. Comparative evaluation of treatment of Oral submucous fibrosis with intralesional injections of Dexamethasone and hyaluronidase with Triamcinolone Acetonide and hyaluronidase. Group [Internet]. 2015;1(9.81):1–61. Available from: http://www.jcmad.com/admin/pdf/337.pdf.
|
| 9. |
Lanjekar AB, Bhowate RR, Bakhle S, Narayane A, Pawar V, Gandagule R. Comparison of efficacy of topical curcumin gel with triamcinolone-hyaluronidase gel individually and in combination in the treatment of oral submucous fibrosis. J Contemp Dent Pr [Internet]. 2020;21(1):83–90. Available from: https://www.thejcdp.com/doi/JCDP/pdf/10.5005/jp-journals-10024-2726.
|
| 10. |
Bansal M. Efficacy of local and systemic corticosteroid and hyaluronidase therapy in oral submucous fibrosis: A histopathological study. Int J Otorhinolaryngol Head Neck Surg [Internet]. 2019;5(2):459–64. Available from: https://www.academia.edu/download/67852970/762.pdf.
|
| 11. |
Morkane C, Gregory JW, Watts P, Warner JT. Adrenal suppression following intralesional corticosteroids for periocular haemangiomas. Arch Dis Child [Internet]. 2011;96(6):587–9. Available from: https://adc.bmj.com/lookup/doi/10.1136/adc.2010.204859.
|