Abstract
Lipoedema is a chronic disease with various manifestation of symptoms, related to excessive deposition of subcutaneous adipose tissue in the legs, hips and buttocks. The scale of the problem is enormous and may affect up to one in five women. Lipoedema is often underdiagnosed and misdiagnosed with lymphedema, obesity or lipohypertrophy. In recent years, lipedema has been diagnosed in an increasing number of younger women, and its first symptoms may manifest already in puberty. Even though it is often perceived as only an aesthetic problem, it has a huge impact on the quality of life, mental health, self-esteem or self-confidence. Moreover, lipoedema causes stigmatization, unfortunately also in healthcare professionals. Nevertheless, recently, diagnostic criteria (also ultrasound) have been created, and lipedema has been classified in ICD-10 (E88.2). There are also more and more treatment options, with emphasis on the role of psychological care. Awareness and knowledge of lipoedema have also increased despite its underestimation but still is not enough. The multidimensional nature of lipoedema and its impact on many aspects of life highlights the essential role of comprehensive support to patients. Nowadays, in times of caring for mental health, it is crucial to increase public awareness and spread knowledge about lipoedema.
Citation
Tomczak J, Dzierla J, Sarba A, Fałczyńska A, Krasiński Z, Gabriel M. Multifaced lipoedema: a problematic and complex condition in the population of young women. Eur J Transl Clin Med. 2025;8(1):103-112Introduction
Lipoedema (ICD 10 code E88.2, ICD 11 code EF02.2) is a chronic disease marked by excessive deposition of subcutaneous adipose tissue in legs, hips and buttocks, mainly occurring in adult women [1]. Various studies have shown that lipoedema affects 11-19% of females [2]. The first symptoms (e.g. moderate and severe leg heaviness, pain, numbness, cold skin, feeling cold or easy bruising) can appear in puberty, which may explain the hormonal background of this disease [2-4]. Additionally, lipoedema has a significant impact on the patient’s mental health and self-esteem [5]. Diagnosis is based on clinical findings and exclusion criteria [6]. The treatment demands a holistic approach, reduction of symptoms severity, preventing impaired function and disease progression. Moreover, the therapeutic approach also includes taking care of factors influencing the course of lipoedema, e.g. obesity [7]. Our aim was to summarize the knowledge about diagnosing and managing patients with lipoedema, a frequently misdiagnosed condition.
Material and methods
We searched for relevant literature published in the years 1950 to 2024 using the PubMed search engine. Due to the spelling differences in British and American literature, we used the keywords “lipedema” and “lipoedema.” German-language articles indexed in PubMed contain abstracts translated to English, therefore we also included them in this search.
Results
We found a total of 577 abstracts. After screening the abstracts and reading the full texts, we included 43 articles in this review.
Epidemiology
The available data is insufficient to reveal the specific prevalence of lipoedema in the general population [8]. Lack of accurate diagnostic markers of lipoedema and confusion regarding its definition results in a high rate of misdiagnosis and wrong mistreatment, which may imply rare diagnosis [9-10]. Several studies have already shown greater prevalence of lipoedema than it was previously suggested. Lipoedema affects 11-19% of females [2]. The estimated frequency of lipoedema in the general population varies between 0.06% and 19% depending on the study [2, 11-13]. However, typical symptoms of lipoedema are common among young women. First symptoms appear already in puberty or childhood (57.1-64.2% of cases) [5, 14]. Also, a study of 209 patients with lipoedema showed that symptoms typically appear around age 16 [4]. In another, 70% of women with lipoedema experienced onset before age 30, but unfortunately only 1.6% were diagnosed earlier by a healthcare professional [3]. Furthermore, cases of lipoedema occurring in children have also been recorded [15-16].
Diagnosis is usually made in middle-aged women, although first symptoms can manifest in puberty, which suggest a hormonal basis of lipoedema [4]. In the literature, there are only a few reported cases of male patients with lipoedema and all of them had a medical history of hyperestrogenemia and hypotestosteronemia [6].
Pathogenesis
The pathophysiology of lipoedema remains unexplained, although some factors such as hormones, genetic predisposition, impaired sympathetic system, and vasculature may play an essential role [17]. Estrogens regulate adipogenesis and adipocyte lipid deposition by metabolic signaling. Their excess may form increased adipose depot mass. The fact that lipoedema often appears in phases of hormonal change such as puberty, pregnancy or menopause confirms this theory [10]. According to the literature, family history of lipoedema varies between 16% and 64% [6, 10, 15]. The familial character of lipoedema was confirmed by revealing the mutation of the gene AKR1C1, which is responsible for the progesterone metabolism, although it is present in obese women or with lipoedema [15, 17-18]. Vessel microangiopathy and lymphatic vessel disfunction are suggested to be typical for lipoedema. Pathological changes in the vessels’ structure conduct excess accumulation fluid in the subcutaneous adipose tissue, causing remodeling, adipose oedema and hematoma due to increased permeability. All of these processes decrease blood flow in subcutaneous adipose tissue, causing inflammation, hypoxia and formation of fibrotic lesions, which patients may perceive as pain [3].
Symptoms and classification
The typical localization of lipoedema adipose tissue is the gynoid region. In 97% cases it involves the hips, buttocks, thighs, and lower legs; only 3% is located in the upper extremities [8]. Almost all the symptoms reported by patients involve feet. Complaints apply to unpleasant sensations of heaviness and compression due to orthostatic oedema. The oedema increases during the day (also due to warmth and exercise) and there is no specific factor that could reduce its intensity [6, 9]. Concerning microangiopathy, patients bruise easily and their subcutaneous capillaries might be dilated [19]. Another cardinal sign is the daily pain (usually described as moderate to severe), which is responsible for reduced quality of life (QoL) and impaired mobility [3]. Pain might be associated with lipoedema adipose tissue, but also with joints and osteoarthritis due to increased body mass. Women with lipoedema are at a high risk of eating disorders, depression and other psychological complaints. Misdiagnosis and stigmatization cause mental conditions, it highlights the importance of distinguishing these two conditions. Nowadays, lipoedema is not linked to any metabolic diseases, although obesity may appear and influence the lipoedema subcutaneous adipose tissue [20].
Based on body distribution of adipose tissue, 5 types of lipoedema were determined by Amato et al. In stage I it is located only around the pelvis, hips and buttocks (the ‘saddle bag’ phenomenon), whereas in stage II it is present in the area from hips to knees, with the formation of folds of fat around the inner side of the knee. Stage III involves the region from hips to ankles, while in the IV stage, adipose edema is concentrated in the arms. The rarest is stage V, which requires involvement of calves [21].
Differential diagnosis
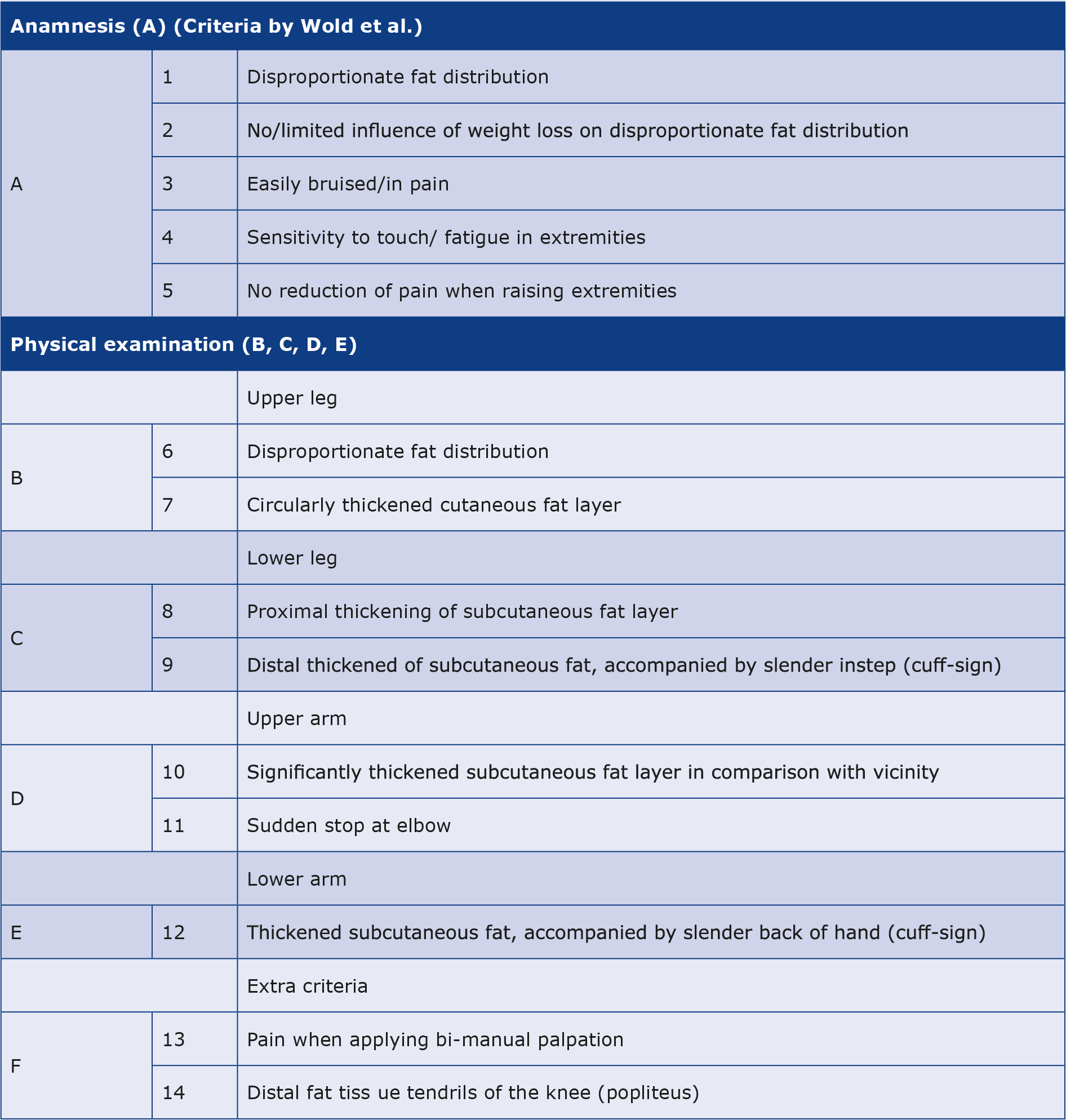
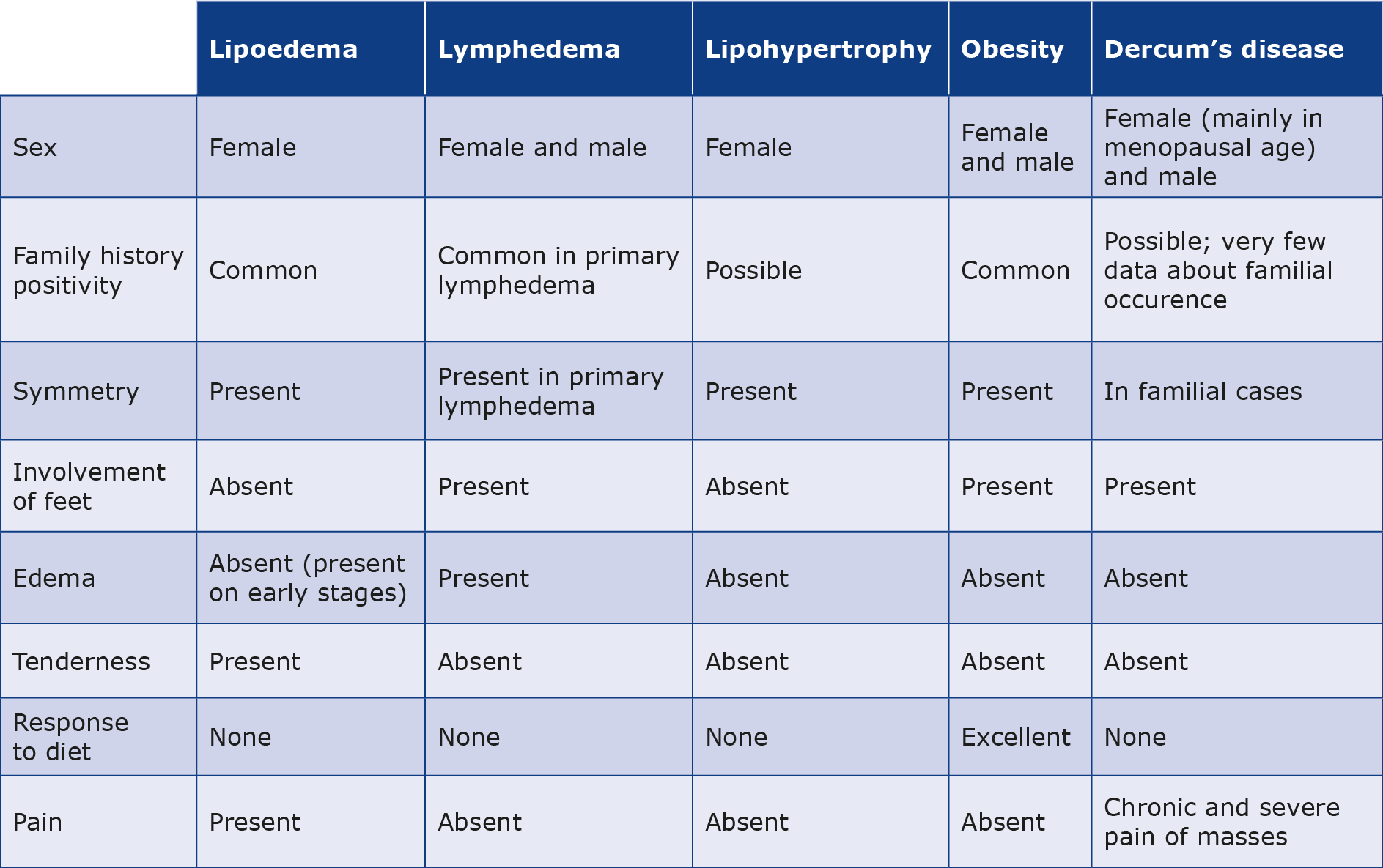
Although there are no specific diagnostic tests or markers that help diagnose lipoedema, some studies highlight the importance of adipose tissue-resident mesenchymal stem cells morphology in lipoedema subcutaneous adipose tissue [22]. Before confirmation of any molecular marker, identification of the condition requires the exclusion of other diseases characterizing oedema and deposition of fat tissue in the lower extremities [9, 15]. Clinicians should always consider localization of symptoms (bilaterally or unilateral). Furthermore, the presence of the Stemmer sign (the examiner pinches the dorsal skin proximal to the metatarsophalangeal joint of the second toe, or metacarpophalangeal joint of the second finger; the sign is positive if the examiner cannot create a fold of pinched skin) enables distinguishing lipoedema from lymphatic edema (lymphedema) and chronic venous insufficiency [8, 23]. Lipoedema typically spares the hands and feet, thus most patients have a negative Stemmer sign. However, a positive Stemmer sign does not rule out lipoedema and suggests the presence of concomitant lymphedema. If both conditions are present, the diagnosis is lipo-lymphedema. Another important symptom is pain (present also in Dercum’s disease (adiposis dolorosa): multiple painful fatty tumors (lipomas), generalized obesity (usually in menopausal age), weakness, fatigue, mental disturbances (including emotional instability, depression) and central nervous system disfunction (e.g. epilepsy, confusion and dementia) [6, 8, 24]. The absence of pain and oedema, but with the presence of increased symmetrical subcutaneous fat deposits in women is associated with lipohypertrophy [8-9]. The differential diagnosis is presented in Table 1.
Table 1. Differential diagnosis of lipoedema, lymphedema, lipohypertrophy, obesity and Dercum’s disease
Diagnostic steps
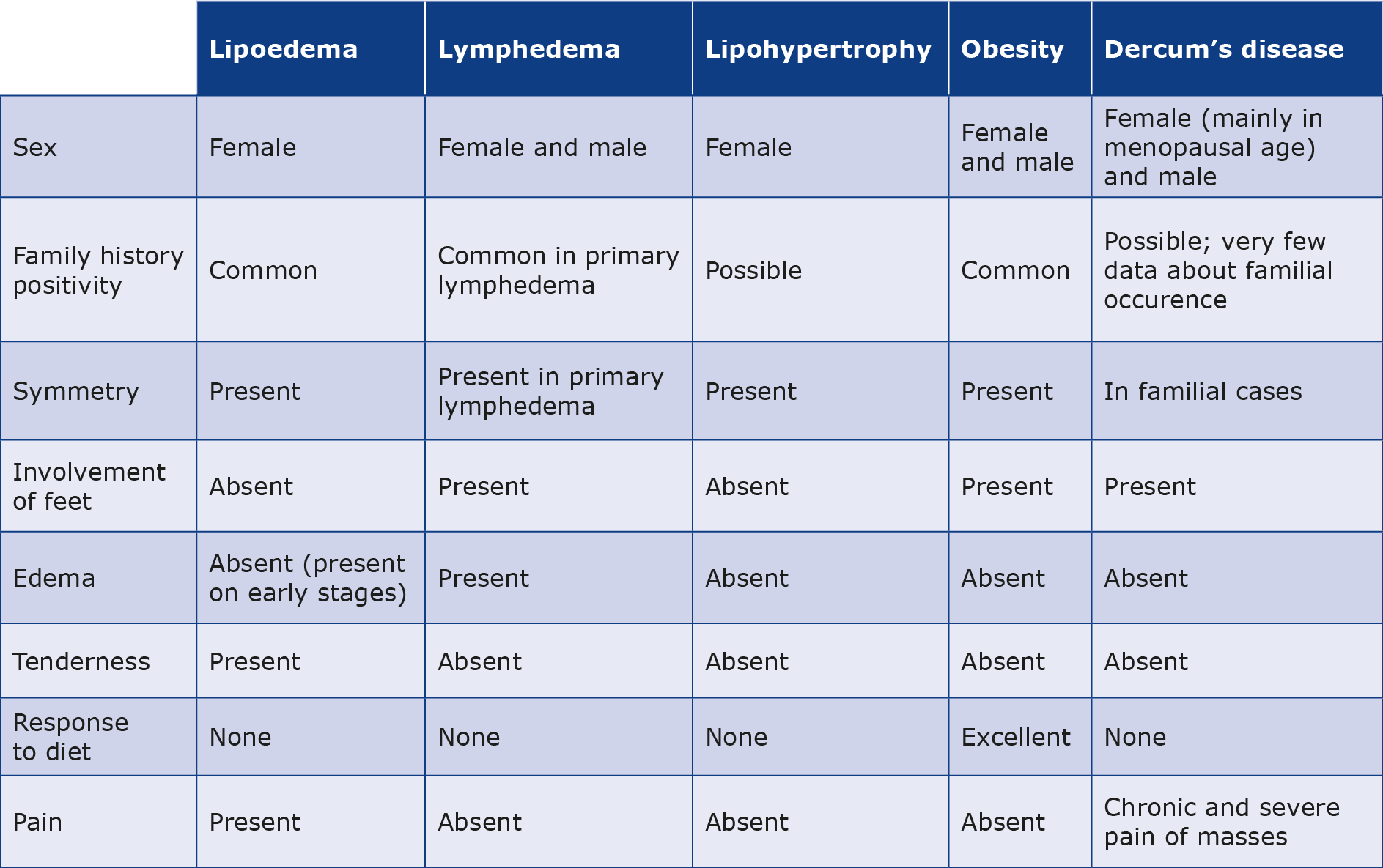
The diagnosis of lipoedema is based on clinical findings and exclusion criteria. First data was published in 1951 by Wold et al. and in 2017 was extended by Halk and Damstra in the form of guidelines (Table 2) [25-26]. Based on the 2017 guidelines by Wounds UK and others, the key steps in the assessment of a patient with suspected lipoedema are:
- detailed medical history (medical/surgical/family history, impact on daily living, mobility, personal relationships, work, emotional state),
- extent, distribution and severity of adipose tissue enlargement,
- skin assessment,
- vascular assessment,
- pain (measured with the numerical rating scale (NRS), visual analogue scale (VAS) or the Schmeller questionnaire),
- mobility and gait,
- dietary assessment,
- assessment of comorbidities,
- psychosocial assessment (there is a need for a validated survey),
- quality of life (SF-36 questionnaires),
- understanding of disease and expectations of treatment outcomes.
Table 2. Diagnosis of lipoedema, table created based on Dutch guidelines [20]
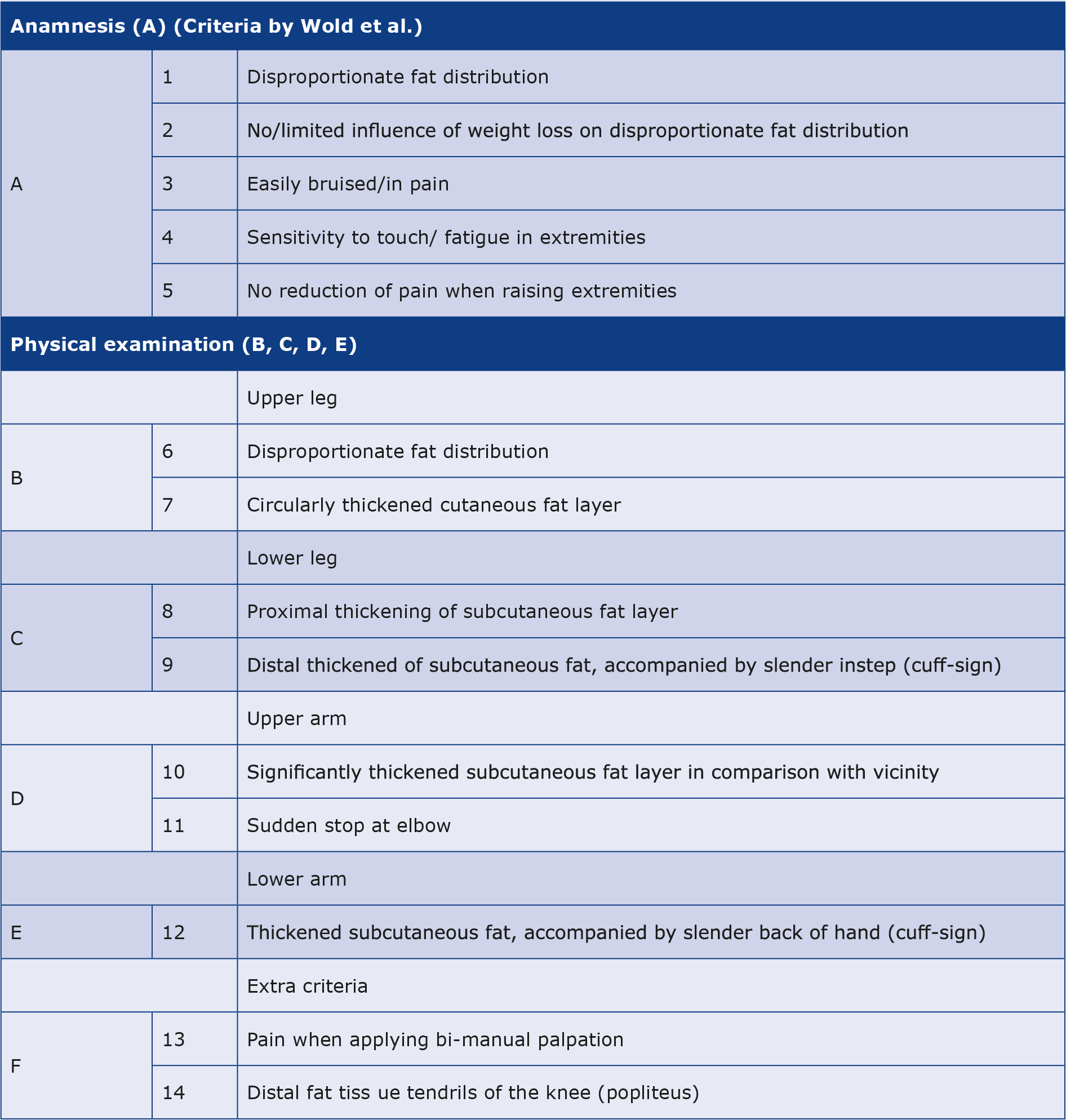
Diagnosis of lipoedema is certain when present: A1+A2+A3+A4+A5 PLUS ((B6+B7) or (C8+C9) or (D10+D11) or E12). In the case of absence of at most two of these five criteria (A to E), the presence of extra criteria F13 or F14 also assures the diagnosis of lipoedema [20].
Proper physical examination includes evaluation of typical signs of lipoedema such as subcutaneous tissue enlargement, cuffing (braceleting) at the ankles/wrists, loss of the concave spaces on either side of the Achilles tendon, bruising, altered skin appearance, temperature and texture, abnormal gait and limited mobility, negative Stemmer’s sign and pitting oedema. It must be highlighted that there are no specific diagnostic tests for lipoedema. Hence, we must exclude other diagnoses based on routine blood tests (urea, electrolytes, full blood count, thyroid function tests, liver, renal function tests, plasma proteins, brain natriuretic peptide, glucose, lipid profiles and insulin resistance) [10-11]. Imaging investigations such as ultrasound scans, magnetic resonance imaging scans or computed tomography may play a role if the diagnosis is uncertain.
Decisions about further management should be made by an interdisciplinary team. Depending on the needs, such team should consist of a clinician specializing in lipoedema/lymphoedema, physiotherapist, occupational therapist, dietitian, podiatrist, pain specialist, vascular specialist, diabetologist, psychologist, plastic surgeon or bariatric surgeon [27].
Imaging
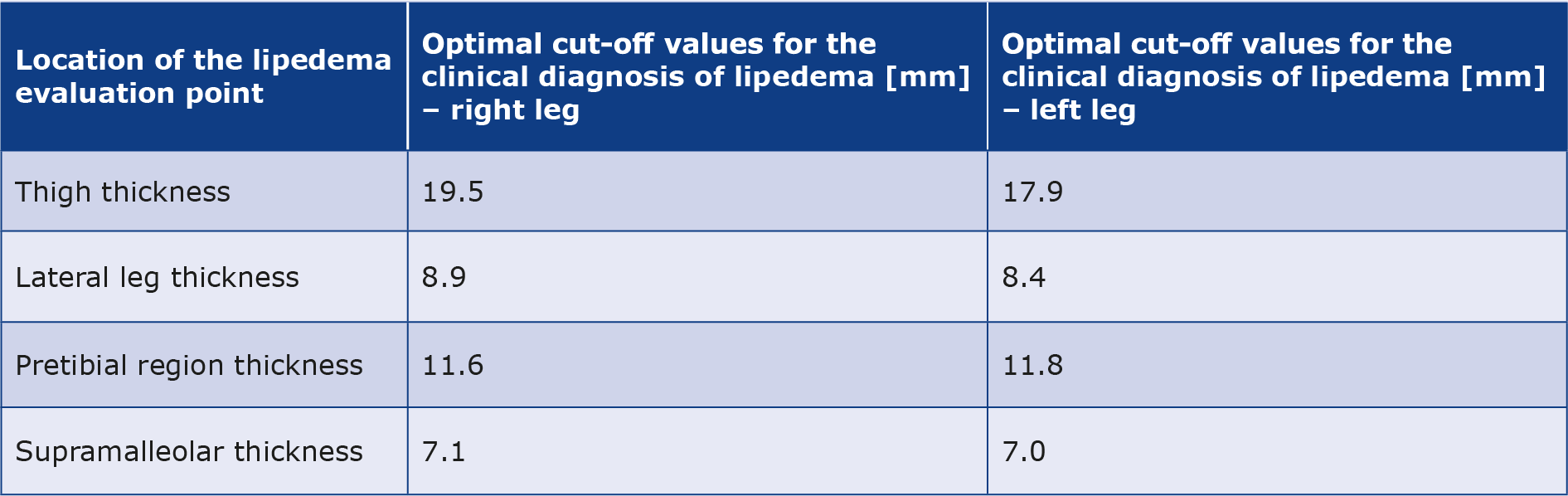
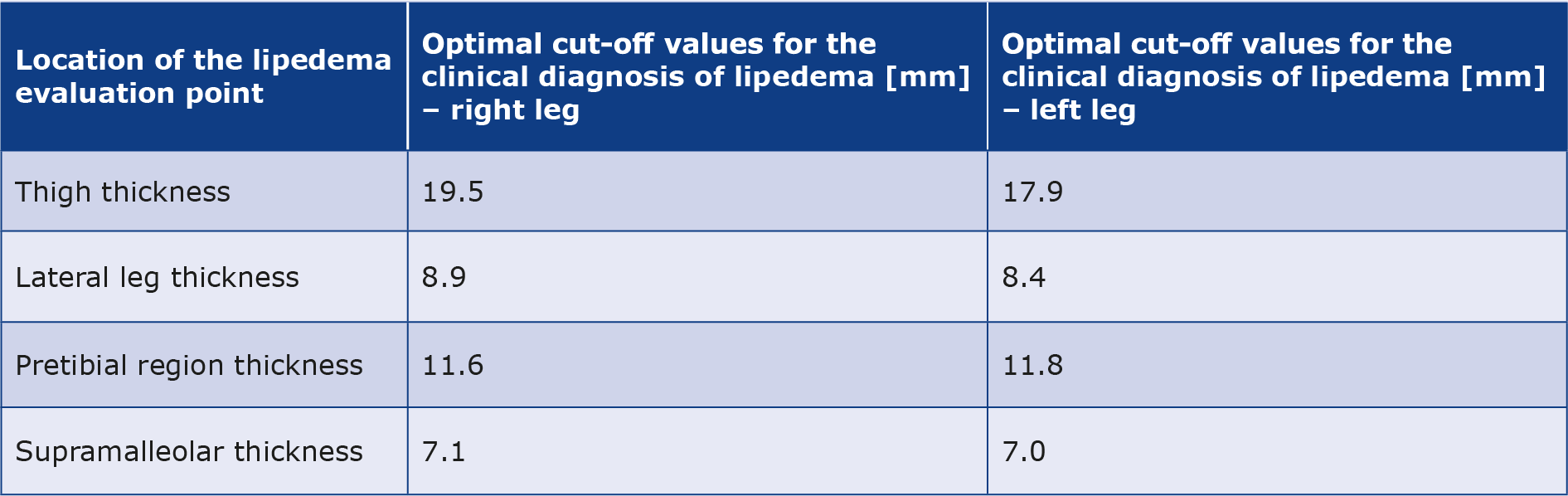
Marshall and Schwahn-Schreiber first proposed an ultrasound-based classification for lipoedema diagnosis based on specific cut-off values of the dermis thickness and subcutaneous tissue measurements 6 to 8 cm proximal the medial malleolus: average measurement for women without lipoedema (2.1 mm), lipohyperplasia or mild lipoedema (12 to 15 mm), moderate lipoedema (15 to 20 mm), indisputable lipoedema (> 20 mm) and severe lipoedema (> 30 mm) [21, 23, 28-29]. Later, Amato et al. described easy-to-obtain ultrasound measurements with the extension of Marshall’s assessment. They suggested evaluating lipoedema at more locations: thigh, pretibial, lateral leg, medial malleolus, and anteromedial region of the proximal leg with typical fat deposition for more precise investigation in the future (Table 3) [21].
Table 3. Optimal cut-off values for the clinical diagnosis of lipoedema using ultrasound suggested by Amato (estimated by Youden index) – an extension of Marshall assessment
Subcutaneous adipose tissue and skin can be likewise examined by computed tomography (CT) and/or magnetic resonance imaging (MRI) [10]. CT can be used to differentiate lipoedema from lymphedema. The presence of subcutaneous fluid accumulation, the honeycomb pattern and muscle enlargement do not occur in lipoedema and therefore confirm the suspicion of lymphedema [8]. MRI is suggested to evaluate lymphatic circulation or to distinguish lipoedema from obesity (examination of subcutaneous fat accumulation) [11, 17]. Non-tracer-based MR lymphangiography evaluates elevated atrial and lymphatic insufficiency in lower extremities [17]. Because of significant changes in body composition presented by patients with lipoedema, bioimpedance and dual-energy X-ray absorptiometry (DXA) are supposed to be diagnostic tools. In some studies, DXA was used to estimate torso and leg fat in comparison to total body mass. In lipoedema fat tissue is mainly localized in lower parts [30]. Alternatively, dysfunction of the lymphatic system might be evaluated by functional tests: lymphoscintigraphy, lymphography or fluorescence microlymphography [10, 17].
Follow-up
Follow-up should include measurement of the body mass index (BMI), waist-hip ratio, waist-height ratio, limb measurements of circumference and volume, and daily activity index. Furthermore, the VAS or the Schmeller questionnaire can help track the changes in the patient’s pain perception [6, 10]. DXA may be performed [16, 31-32]. Follow-up plays a crucial role in further management and in choice of the proper treatment [6].
Possible treatment options
The main aim of lipoedema treatment is the reduction of symptom severity, prevention of impaired functioning and progression of disease. The therapeutic approach is also focused on factors such as obesity and venous insufficiency and goals such as educating patients about the nature of lipoedema, treatment options and possible impact of a patient on the disease [6, 9-10] The role of weight control and appropriate dietary modifications should be emphasized [6, 10, 19]. An algorithm of potential diagnostic and therapeutic work‐up for patients with suspected lipoedema was proposed by Buso et al. [6]. It highlighted the role of conservative treatment based on information, education, amultidisciplinary approach to encourage an active lifestyle, elastic compression stocking, decongestive lymphatic therapy (DLT) and complex decongestive therapy (CDT, more details below). If these methods are not effective after follow-up, surgical methods such as tumescent liposuction or lipectomy should be considered [6, 33-34].
Medicaments
The role of pharmacological treatment in lipoedema has not been explained yet. Favorable results can be obtained with beta-adrenergic agonists, corticosteroids, diuretics, flavonoids and selenium [6, 19, 35].
Complex decongestive therapy
CDT is a part of conservative treatment which reduces pain and discomfort in the extremities. It consists of manual lymph drainage (MLD) associated with multilayered and multicomponent compression bandaging, meticulous skin care and physical exercise [6, 11]. MLD reduces the load of lymph stasis on the limb by directing the lymph into the non-edematous part. It can be combined with intermittent pneumatic compression (IPC) which improves venous flow and reduces edema [11, 17]. However, it is important to apply only mild pressure of IPC in the treatment of lipoedema, considering subsiding superficial lymphatic vessels [10].
Surgery
Surgery is the second line treatment. When symptoms are worsening and affecting the patient’s QoL, two options can be considered: liposuction and lipectomy [6, 10, 33, 36-37]. Those two methods result in better outcomes because of less lymphatic tissue damage than in traditional techniques [19, 37-38]. Although liposuction cannot cure lipoedema, it results in decrease in symptoms such as pain and tendency to swell as well as improves the patient’s mobility and well-being. Furthermore, it is safe, usually without late complications [9, 37, 39]. Unfortunately, liposuction usually requires multiple sessions related to the extensiveness of adipose tissue that should be removed. Compared to lipectomy, it is performed in the early stages of lipoedema and prevents clinical progression [9, 36]. Advanced stages of lipoedema with accompanying lymphedema usually require surgical debulking due to the presence of multiple fibrotic tissue [10]. Patients with early stages should use a postoperative compression garment for at least 2-3 months to manage postoperative edema, whereas those with advanced stages even for the rest of their life [18, 36].
Quality of life
At this time there are no established guidelines for the psychological care of patients with lipoedema, and there is a lack of data on the most frequently used diagnostic tools or treatments. However, with the growing focus on mental health, this matter should be explored in future research.
Dudek et al. conducted a survey among 130 Polish women aged 22 to 73 with lipoedema and found that 98 of them (75.38%) experienced varying degrees of depression, which depended on the intensity of lipoedema symptoms such as leg pain, heaviness, swelling, bruising, muscle and joint pain [5]. The respondents reported elevated levels of depressive symptoms and reduced QoL across various domains, including physical and psychological health, social relationships and even environment [5]. Another study by Dudek et al. has shown the importance of addressing appearance-related distress in patients with lipoedema [32]. Other studies have also emphasized the impact of this disease on mental health and QoL [4, 40] with a holistic approach. Additionally, confusion between lipoedema and obesity or dietary and lifestyle mistakes can further compound the issue [19].
The final diagnosis of lipoedema brings a relief for some patients, although younger women typically responded to the diagnosis with reduced well-being [7]. Specifically, these women often felt helpless, knowing that treatment might not alleviate their symptoms to the extent they hoped, leading to anxiety and even self-loathing [7, 41]. Regarding the inconvenience associated with the disease, women mentioned difficulties in finding properly fitting clothing [7, 12]. When assessing the level of life satisfaction, more than half of them rated their life satisfaction as low, and 59 individuals (60.1%) reported being dissatisfied or very dissatisfied [5].
In a Dutch study conducted in 2018 by Romejn et al., the QoL of lipoedema patients was analyzed using EQ-5D-3L and RAND-36 questionnaires, both used to evaluate health-related QoL [8]. Among lipoedema patients, the average EQ-5D- -3L index was 66.1/100, while the average score for the Dutch population was 85/100. Additionally, the RAND-36 score for lipoedema patients was 59.3/100, compared to the Dutch population’s average score of 74.9/100 [14]. Another challenge is difficulty in forming romantic relationships because patients often feel ashamed of their bodies [7].
Aesthetic issues (complexes) regarding the appearance and disproportion of the body may coexist with lipoedema, e.g. the problem of fat loss from the limb extremities area, a general feeling of discomfort (not accepting one’s own body, covering legs), reduced self-confidence, lowered self-esteem, disliking oneself, feeling of heavy lower extremities, problems with choosing the right size of clothes, the shame of showing lower limbs [1, 7, 19, 41-42].
Discussion
It is noteworthy that limited research is focused specifically on lipoedema among young women in their 20s and early 30s [7].
Lipoedema is a complex disease, which despite the increased amount of information about it, still remains an underestimated health problem [19]. Recent studies have increasingly shed light on the psychological aspect of lipoedema [5, 7]. Women often perceive themselves as overweight and try to improve their body’s appearance through restrictive diets and exercise which unfortunately cannot reduce the fatty swelling in areas affected by lipoedema [31, 41]. On the contrary, the achieved weight loss further underlines the disproportions of patient’s body [42]. The ineffectiveness of these measures reduces self-confidence and sense of selfworth [19, 41].
Most patients had relatives with lipoedema, therefore the hereditary basis of lipoedema is also being discussed more and more frequently [4]. In a genome-wide association study (GWAS) conducted by Yann C. Klimentidis et al., 18 loci across the genome were identified as potential genetic risk factors for lipoedema. Two of these loci (VEGFA and GRB14-COBLLI) were successfully replicated in another study with clinically diagnosed lipoedema cases. These findings could be the background for future studies about prevention strategies or treatment [1].
As revealed by Christoffersen and Tennfjord, awareness of lipoedema is limited not only among patients but also among healthcare professionals in Norway [7]. Moreover, in that study women between 21 and 47 years of age experienced stigmatization by healthcare workers (felt perceived as lazy and believed that their health problem was being dismissed). Stigmatization of lipoedema patients is widespread in all aspects of life, and patients are often blamed for their condition and health status. It is worth noting that lipoedema is often misdiagnosed as lymphedema, leading patients to pursue ineffective treatment [7, 12]. These studies highlight a lack of awareness about lipoedema among medical professionals and there is limited research on its occurrence in young people beyond what has been mentioned. A study by Dudek et al. shows that only 44.9% of participants were diagnosed with lipoedema by medical health professionals [5]. Another study found that a mean time from the first symptoms to the diagnosis was 10-15 years [4]. Thus, it is crucial for medical professionals (e.g. doctors, nurses, physiotherapists, dietitians and students) to gain knowledge and awareness about lipoedema more rapidly.
However, also differential diagnosis is a challenge, as up to 15-17% of women treated for lymphedema at that time had lipoedema [13]. Fortunately, awareness and knowledge of lipoedema have been increasing. Nowadays we can use the ultrasound criteria for diagnosis [21]. Furthermore, in the United States in 2021 Herbst et al. developed and published a standard of care for lipoedema [18]. In 2018 the diagnosis of lipoedema was included in the 11th version of International Classification of Diseases 11 (code EF02.2) [43]. The financial burden of lipoedema has not been estimated yet. Treating patients with lipoedema can be very expensive due to the need for a comprehensive approach that includes not only the causal treatment but also the support of multiple specialists.
Lipoedema often co-occurs with various other diseases, including obesity, as well as heart and vascular complications (for example venous varicose and secondary lymphedema) [14, 18, 44] These comorbidities can further exacerbate symptoms and negative impact on QoL [3, 14]. Moreover, hormonal alterations may play a significant role in the development and progression of lipoedema which frequently coexists with hypothyroidism, diabetes mellitus or sexual hormonal imbalances [1]. Numerous studies have shown that lipoedema can be also influenced by hormonal factors such as the use of contraception, menopause, puberty or pregnancy [2]. Further research in this area is needed to explore lipoedema’s association with other chronic diseases.
Conclusions
Lipoedema affects patients’ life clinically, psychologically and economically. Lipoedema is probably underdiagnosed and more studies are needed to reveal its prevalence, particularly among young women and teenagers. It is crucial to define the pathophysiology of lipoedema and find accurate, easily-available diagnostic markers. Clinical trials could help establish causal treatment. We need a holistic approach (with psychological support) to patients with lipoedema, standardization of patient care, improved differential diagnosis and awareness, not only among patients, but also in the training of future healthcare professionals. Promoting awareness (e.g. via the internet and social media) can contribute to increased self-acceptance among patients with lipoedema [5, 42].
Conflict of interests
None.
Funding
None.
References
| 1. |
Klimentidis YC, Chen Z, Gonzalez-Garay ML, Grigoriadis D, Sackey E, Pittman A, et al. Genome-wide association study of a lipedema phenotype among women in the UK Biobank identifies multiple genetic risk factors. Eur J Hum Genet [Internet]. 2023;31(3):338–44. Available from: https://www.nature.com/articles/s41431-022-01231-6.
|
| 2. |
Katzer K, Hill JL, McIver KB, Foster MT. Lipedema and the Potential Role of Estrogen in Excessive Adipose Tissue Accumulation. Int J Mol Sci [Internet]. 2021;22(21):11720. Available from: https://www.mdpi.com/1422-0067/22/21/11720.
|
| 3. |
Falck J, Rolander B, Nygårdh A, Jonasson L-L, Mårtensson J. Women with lipoedema: a national survey on their health, health-related quality of life, and sense of coherence. BMC Womens Health [Internet]. 2022;22(1):457. Available from: https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-022-02022-3.
|
| 4. |
Bauer A-T, von Lukowicz D, Lossagk K, Aitzetmueller M, Moog P, Cerny M, et al. New Insights on Lipedema: The Enigmatic Disease of the Peripheral Fat. Plast Reconstr Surg [Internet]. 2019;144(6):1475–84. Available from: https://journals.lww.com/10.1097/PRS.0000000000006280.
|
| 5. |
Dudek JE, Białaszek W, Gabriel M. Quality of life, its factors, and sociodemographic characteristics of Polish women with lipedema. BMC Womens Health [Internet]. 2021;21(1):27. Available from: https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-021-01174-y.
|
| 6. |
Buso G, Depairon M, Tomson D, Raffoul W, Vettor R, Mazzolai L. Lipedema: A Call to Action! Obesity [Internet]. 2019;27(10):1567–76. Available from: https://onlinelibrary.wiley.com/doi/10.1002/oby.22597.
|
| 7. |
Christoffersen V, Tennfjord MK. Younger Women with Lipedema, Their Experiences with Healthcare Providers, and the Importance of Social Support and Belonging: A Qualitative Study. Int J Environ Res Public Health [Internet]. 2023;20(3):1925. Available from: https://www.mdpi.com/1660-4601/20/3/1925.
|
| 8. |
Forner‐Cordero I, Szolnoky G, Forner‐Cordero A, Kemény L. Lipedema: an overview of its clinical manifestations, diagnosis and treatment of the disproportional fatty deposition syndrome – systematic review. Clin Obes [Internet]. 2012;2(3–4):86–95. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1758-8111.2012.00045.x.
|
| 9. |
Langendoen SI, Habbema L, Nijsten TEC, Neumann HAM. Lipoedema: from clinical presentation to therapy. A review of the literature. Br J Dermatol [Internet]. 2009;161(5):980–6. Available from: https://academic.oup.com/bjd/article/161/5/980/6642385.
|
| 10. |
Kruppa P, Georgiou I, Biermann N, Prantl L, Klein-Weigel P, Ghods M. Lipedema — Pathogenesis, Diagnosis, and Treatment Options. Dtsch Arztebl Int [Internet]. 2020; Available from: https://www.aerzteblatt.de/10.3238/arztebl.2020.0396.
|
| 11. |
Forner-Cordero I, Forner-Cordero A, Szolnoky G. Update in the management of lipedema. Int Angiol [Internet]. 2021;40(4). Available from: https://www.minervamedica.it/index2.php?show=R34Y2021N04A0345.
|
| 12. |
Fife CE, Maus EA, Carter MJ. Lipedema. Adv Skin Wound Care [Internet]. 2010;23(2):81–92. Available from: https://journals.lww.com/00129334-201002000-00010.
|
| 13. |
Földi M, Földi E, Strössenreuther RHK, Kubik S. Földi’s Textbook of Lymphology: For Physicians and Lymphedema Therapists [Internet]. Mosby; 2006. Available from: https://books.google.pl/books?id=b6VwL4eaGyIC.
|
| 14. |
Romeijn JRM, de Rooij MJM, Janssen L, Martens H. Exploration of Patient Characteristics and Quality of Life in Patients with Lipoedema Using a Survey. Dermatol Ther (Heidelb) [Internet]. 2018;8(2):303–11. Available from: http://link.springer.com/10.1007/s13555-018-0241-6.
|
| 15. |
Child AH, Gordon KD, Sharpe P, Brice G, Ostergaard P, Jeffery S, et al. Lipedema: An inherited condition. Am J Med Genet Part A [Internet]. 2010;152A(4):970–6. Available from: https://onlinelibrary.wiley.com/doi/10.1002/ajmg.a.33313.
|
| 16. |
Schook CC, Mulliken JB, Fishman SJ, Alomari AI, Grant FD, Greene AK. Differential Diagnosis of Lower Extremity Enlargement in Pediatric Patients Referred with a Diagnosis of Lymphedema. Plast Reconstr Surg [Internet]. 2011;127(4):1571–81. Available from: http://journals.lww.com/00006534-201104000-00022.
|
| 17. |
Poojari A, Dev K, Rabiee A. Lipedema: Insights into Morphology, Pathophysiology, and Challenges. Biomedicines [Internet]. 2022;10(12):3081. Available from: https://www.mdpi.com/2227-9059/10/12/3081.
|
| 18. |
Herbst KL, Kahn LA, Iker E, Ehrlich C, Wright T, McHutchison L, et al. Standard of care for lipedema in the United States. Phlebol J Venous Dis [Internet]. 2021;36(10):779–96. Available from: https://journals.sagepub.com/doi/10.1177/02683555211015887.
|
| 19. |
Buck DW, Herbst KL. Lipedema: A Relatively Common Disease with Extremely Common Misconceptions. Plast Reconstr Surg - Glob Open [Internet]. 2016;4(9):e1043. Available from: https://journals.lww.com/01720096-201609000-00012.
|
| 20. |
Keith L, Seo CA, Rowsemitt C, Pfeffer M, Wahi M, Staggs M, et al. Ketogenic diet as a potential intervention for lipedema. Med Hypotheses [Internet]. 2021;146:110435. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0306987720333260.
|
| 21. |
Amato ACM, Saucedo DZ, Santos K da S, Benitti DA. Ultrasound criteria for lipedema diagnosis. Phlebol J Venous Dis [Internet]. 2021;36(8):651–8. Available from: https://journals.sagepub.com/doi/10.1177/02683555211002340.
|
| 22. |
Ernst AM, Bauer H, Bauer H-C, Steiner M, Malfertheiner A, Lipp A-T. Lipedema Research — Quo Vadis? J Pers Med [Internet]. 2022;13(1):98. Available from: https://www.mdpi.com/2075-4426/13/1/98.
|
| 23. |
Goss JA, Greene AK. Sensitivity and Specificity of the Stemmer Sign for Lymphedema: A Clinical Lymphoscintigraphic Study. Plast Reconstr Surg - Glob Open [Internet]. 2019;7(6):e2295. Available from: https://journals.lww.com/01720096-201906000-00013.
|
| 24. |
Kucharz EJ, Kopeć-Mędrek M, Kramza J, Chrzanowska M, Kotyla P. Dercum’s disease (adiposis dolorosa): a review of clinical presentation and management. Rheumatology [Internet]. 2019;57(5):281–7. Available from: https://reu.termedia.pl/Dercum-s-disease-adiposis-dolorosa-a-review-of-clinical-presentation-and-management,112434,0,2.html.
|
| 25. |
Wold LE, Hines EA, Allen E V. Lipedema of the Legs: a Syndrome Characterized by Fat Legs and Edema. Ann Intern Med [Internet]. 1951;34(5):1243–50. Available from: https://www.acpjournals.org/doi/10.7326/0003-4819-34-5-1243.
|
| 26. |
Halk AB, Damstra RJ. First Dutch guidelines on lipedema using the international classification of functioning, disability and health. Phlebol J Venous Dis [Internet]. 2017;32(3):152–9. Available from: https://journals.sagepub.com/doi/10.1177/0268355516639421.
|
| 27. |
Hardy D, Williams A. Best practice guidelines for the management of lipoedema. Br J Community Nurs [Internet]. 2017;22(Sup10):S44–8. Available from: http://www.magonlinelibrary.com/doi/10.12968/bjcn.2017.22.Sup10.S44.
|
| 28. |
Marshall M, Schwahn-Schreiber C. Prävalenz des Lipödems bei berufstätigen Frauen in Deutschland. Phlebologie [Internet]. 2011;40(03):127–34. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0037-1621766.
|
| 29. |
Seo C. Prävalenz des Lipödems bei berufstätigen Frauen [Internet]. Lipedema Project. 2016 [cited 2024 Apr 13]. Available from: https://lipedemaproject.org/prvalenz-des-lipdems-bei-berufs-ttigen-frauen-in/.
|
| 30. |
Czerwińska M, Teodorczyk J, Hansdorfer-Korzon R. A Scoping Review of Available Tools in Measurement of the Effectiveness of Conservative Treatment in Lipoedema. Int J Environ Res Public Health [Internet]. 2022;19(12):7124. Available from: https://www.mdpi.com/1660-4601/19/12/7124.
|
| 31. |
Tuğral A, Bakar Y. An approach to lipedema: a literature review of current knowledge of an underestimated health problem. Eur J Plast Surg [Internet]. 2019;42(6):549–58. Available from: http://link.springer.com/10.1007/s00238-019-01519-9.
|
| 32. |
Dudek JE, Białaszek W, Ostaszewski P, Smidt T. Depression and appearance-related distress in functioning with lipedema. Psychol Health Med [Internet]. 2018;23(7):846–53. Available from: https://www.tandfonline.com/doi/full/10.1080/13548506.2018.1459750.
|
| 33. |
Anne Warren Peled A, Kappos E. Lipedema: diagnostic and management challenges. Int J Womens Health [Internet]. 2016;Volume 8:389–95. Available from: https://www.dovepress.com/lipedema-diagnostic-and-management-challenges-peer-reviewed-article-IJWH.
|
| 34. |
Goodliffe JM, Ormerod JOM, Beale A, Ramcharitar S. An under-diagnosed cause of leg swelling. BMJ Case Rep [Internet]. 2013;bcr2013009538. Available from: https://casereports.bmj.com/lookup/doi/10.1136/bcr-2013-009538.
|
| 35. |
Herbst KL. Rare adipose disorders (RADs) masquerading as obesity. Acta Pharmacol Sin [Internet]. 2012;33(2):155–72. Available from: https://www.nature.com/articles/aps2011153.
|
| 36. |
Warren Peled A, Slavin SA, Brorson H. Long-term Outcome After Surgical Treatment of Lipedema. Ann Plast Surg [Internet]. 2012;68(3):303–7. Available from: https://journals.lww.com/00000637-201203000-00017.
|
| 37. |
Rapprich S, Baum S, Kaak I, Kottmann T, Podda M. Treatment of lipoedema using liposuction. Phlebologie [Internet]. 2015;44(03):121–32. Available from: http://www.thieme-connect.de/DOI/DOI?10.12687/phleb2265-3-2015.
|
| 38. |
Stiefelhagen P. No lymphedema, no obesity. How can lipedema be treated? MMW Fortschr Med [Internet]. 2001;143(35–36):15. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11584522.
|
| 39. |
Rapprich S, Dingler A, Podda M. Liposuction is an effective treatment for lipedema–results of a study with 25 patients. JDDG J der Dtsch Dermatologischen Gesellschaft [Internet]. 2011;9(1):33–40. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1610-0387.2010.07504.x.
|
| 40. |
Greene A, Meskell P. The impact of lower limb chronic oedema on patients’ quality of life. Int Wound J [Internet]. 2017;14(3):561–8. Available from: https://onlinelibrary.wiley.com/doi/10.1111/iwj.12648.
|
| 41. |
Torre YS-D la, Wadeea R, Rosas V, Herbst KL. Lipedema: friend and foe. Horm Mol Biol Clin Investig [Internet]. 2018;33(1). Available from: https://www.degruyter.com/document/doi/10.1515/hmbci-2017-0076/html.
|
| 42. |
de Oliveira J. Lipedema, body-related emotional and disordered eating to cope. Surg Obes Relat Dis [Internet]. 2023;19(6):667–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1550728923001302.
|
| 43. |
ICD-11 for Mortality and Morbidity Statistics [Internet]. 2024 [cited 2024 Oct 22]. Available from: https://icd.who.int/browse/2024-01/mms/en.
|
| 44. |
Czerwińska M, Ostrowska P, Hansdorfer-Korzon R. Lipoedema as a Social Problem. A Scoping Review. Int J Environ Res Public Health [Internet]. 2021;18(19):10223. Available from: https://www.mdpi.com/1660-4601/18/19/10223.
|