Awareness and knowledge of drug-drug and food-drug interactions among adults in Poland – a questionnaire-based survey
Abstract
Background: Drug-drug and food-drug interactions can affect the pharmacokinetic and pharmacodynamic properties of drugs, significantly impacting their efficiency and safety profile. Patient awareness of these interactions is vital for their ability to avoid potential risks.
Material and methods: A total of 127 patients participated in the study and completed the questionnaire designed to assess their awareness of drug-drug and food-drug interactions, as well as their habits of medicine administration and the sources of information they relied on regarding drug usage.
Results: Factors such as young age, female sex, higher education and urban living were linked to a greater awareness of drug-drug and food-drug interactions. Most patients reported using water to swallow pills, while some admitted to using tea or juice. Tea consumption was more prevalent among men and elderly individuals. Moreover, a higher level of education was associated with a decreased likelihood of patient consuming tea with prescribed medicines.
Conclusions: Effective education regarding drug-drug and food-drug interactions is essential to increase patients’ awareness and mitigate the potential consequences of these interactions. Initiating education on safe pharmacotherapy at the primary school level and emphasizing its significance in the training of future pharmacists and doctors is imperative.
Citation
Kuźbicka K, Pawłowska I J, Pawłowski L, Kocić I. Awareness and knowledge of drug-drug and food-drug interactions among adults in Poland – a questionnaire-based survey. Eur J Transl Clin Med. 2024;7(2):40-49Introduction
Proper administration of medications is crucial for ensuring their effectiveness and safety in therapy. One critical aspect of drug usage is the potential for interactions. Drug-drug or drug-food interactions can significantly change the pharmacokinetic and pharmacodynamic properties of medications, potentially leading to reduced efficacy or increased adverse effects [1-2]. These interactions are relatively common, for instance 166 drug-drug interactions among 76 patients were identified in a study from Crete, with 12% of these interactions classified as serious [3]. The drugs most frequently associated with these interactions include anti-bacterial and antiretroviral agents. Additionally, over-the-counter medications are often involved in such interactions, particularly non-steroidal anti-inflammatory drugs (NSAIDs), antacids, proton pump inhibitors and diet supplements [4]. In addition to interactions with other drugs medications can also interact with food or specific food components, thus changing the effectiveness of therapy by either enhancing or diminishing the drug’s action, e.g. by reducing drug bioavailability of altering drug metabolism [5-7]. Therefore, it is important to avoid combining certain drugs with particular foods [8].
Drugs, particularly solid formulations (tablets and capsules) and liquid formulations (syrups and elixirs) should never be swallowed without water. Undoubtedly, water is essential for taking medications safely and effectively. Using tea or juice to swallow drugs can alter drug’s bioavailability or onset of action. For instance, catechin found in green tea inhibits the CYP3A4 enzyme, which changes the metabolism of sildenafil, potentially leading to dangerous adverse effects (e.g. hypotension, priapism) [9]. Additionally, animal studies showed that green tea extract can exacerbate hepatotoxicity when administered after paracetamol [10]. Mixing drugs with fruit juices can also result in potentially harmful interactions. Grapefruit juice, well-known inhibitor of the CYP3A4 enzyme, can interact with at least 20 different drugs, e.g. terfenadine, saquinavir, cyclosporin, midazolam, triazolam and verapamil [11]. Apple can decrease the bioavailability of fexofenadine, atenolol and aliskiren, while orange juice can decrease the bioavailability of aliskiren, atenolol, celiprolol, montelukast, fluoroquinolones and alendronate. On the other hand, orange juice can enhance the bioavailability of aluminium-containing antacids [12]. Moreover, orange juice containins vitamin C, therefore it can improve the absorption of iron, which can be beneficial for patients with iron deficiency [12].
Food can also influence drug’s bioavailability and in most cases it is reduced after meals [5]. For example, it was demonstrated that food intake delayed the absorption rate and decreased the bioavailability of levocetirizine [13]. Similarly, the bioavailability of esomeprazole was reduced when taken with food compared to when taken on an empty stomach [14]. Whereas, food can also enhance the drug’s bioavailability, as seen with propranolol [15]. Additionally, the presence of food can delay the onset of action of certain drugs, e.g. nonsteroidal anti-inflammatory drugs (NSAIDs), which can be crucial when the rapid relief is needed [16]. Rarely food can expedite the onset of action of certain drugs, e.g. theophylline or griseofulvin taken with a high fat meal.
It is evident that understanding the potential drug-drug and food-drug interactions is essential to avoid adverse effects. Patients should be informed about the possibility of such interactions before starting a new medication regimen. The aim of this study was to assess the patients’ awareness and knowledge of drug-drug and drug-food interactions that may occur during drug therapy. In addition, we investigated the medications taken by patients and their administration habits.
Materials and methods
Study design
We conducted a qualitative questionnaire-based, cross-sectional survey among adult patients from a public outpatient clinic during a consultation with a dietitian (as part of diabetes prevention) in the Pomeranian region (Northern part of Poland). Approval for the study was obtained from the Ethical Committee of the Medical University of Gdańsk (approval number NKBBN/316/2021) and all participants provided written consent to participate. Data collection took place between November 2021 and January 2023.
The questionnaire
The research tool utilized was an original questionnaire developed by the researchers from the Medical University of Gdańsk (Poland). Professionals with expertise in pharmacology reviewed the questionnaire and based on their suggestions, it was revised to its final version. The questionnaire included inquiries about their medications and related habits. It consisted of 3 parts and a total of 34 questions. Most of the questions were close-ended predefined (answer options such as ‘Yes’, ‘No’, ‘I don’t know’), however the participants also had the opportunity to select ‘Other’ or write their own answers.
The first part of the questionnaire (15 questions) aimed at gathering information about the respondents’ characteristics, e.g. age, sex, place of residence (urban, suburban, rural), educational background, chronic diseases. Participants were also asked about their use of medication (on a regular and occasional basis), including any over-the-counter (OTC) drugs or dietary supplements. Furthermore, responders were queried about their basic knowledge regarding potential interactions between different drugs and between food and drugs. The second part of the questionnaire (4 questions) was intended for patients who reported taking OTC drugs and/or dietary supplements and focused on their administration (e,g. “Do you read the leaflet before use of the new drug/supplement?”, “Do you follow the advice of medical staff?”, “What do you drink to swallow the drug/supplement?”). The third part of the questionnaire (6 questions) concerned the use of prescribed medications (e.g. “Do you read the leaflet before use of the new drug?”, “Do you follow the medical staff advices?”, “What do you drink to swallow the drug?”). Additionally, this section included more specific questions for patients who took proton pump inhibitors, fibrates and levothyroxine.
The questionnaire was prepared in the national language (Polish) and presented in a clear and simple layout. Participants received instructions on how to complete it. The questionnaire was completed during a consultation with a dietitian, either independently by the patient or with the assistance of consulting dietitian. If necessary, the dietitian read the questions aloud to the participants. After completing the questionnaire, the dietitian discussed specific aspects of fooddrug interactions with each patient, particularly when the patient completed the final section regarding specific medications or reported taking multiple OTC drugs and/or dietary supplements. The dietitian provided advice on how to take these medications and supplements to avoid potential interactions. Patients with limited cognitive function (e.g. with dementia) were excluded from this study. All patients participated voluntarily and did not receive any compensation for their involvement in the study.
Statistical analyses
We aimed to achieve a 90% confidence level with a 7% margin of error, thus we calculated that the sample size should be 139 respondents. The questionnaires were collected by a single researcher within a limited timeframe, therefore such sample size provided a balance between statistical validity and practical feasibility. Pearson’s chi-squared test and descriptive statistics were applied to the data. The Chi square test was employed to examine correlations between the knowledge of interactions, dietary supplement use and sex, age, level of education and the presence of chronic diseases. All statistical analyses were performed using the Statistica software version 10 (TIBCO Software Inc, Palo Alto, USA).
Results
Study population
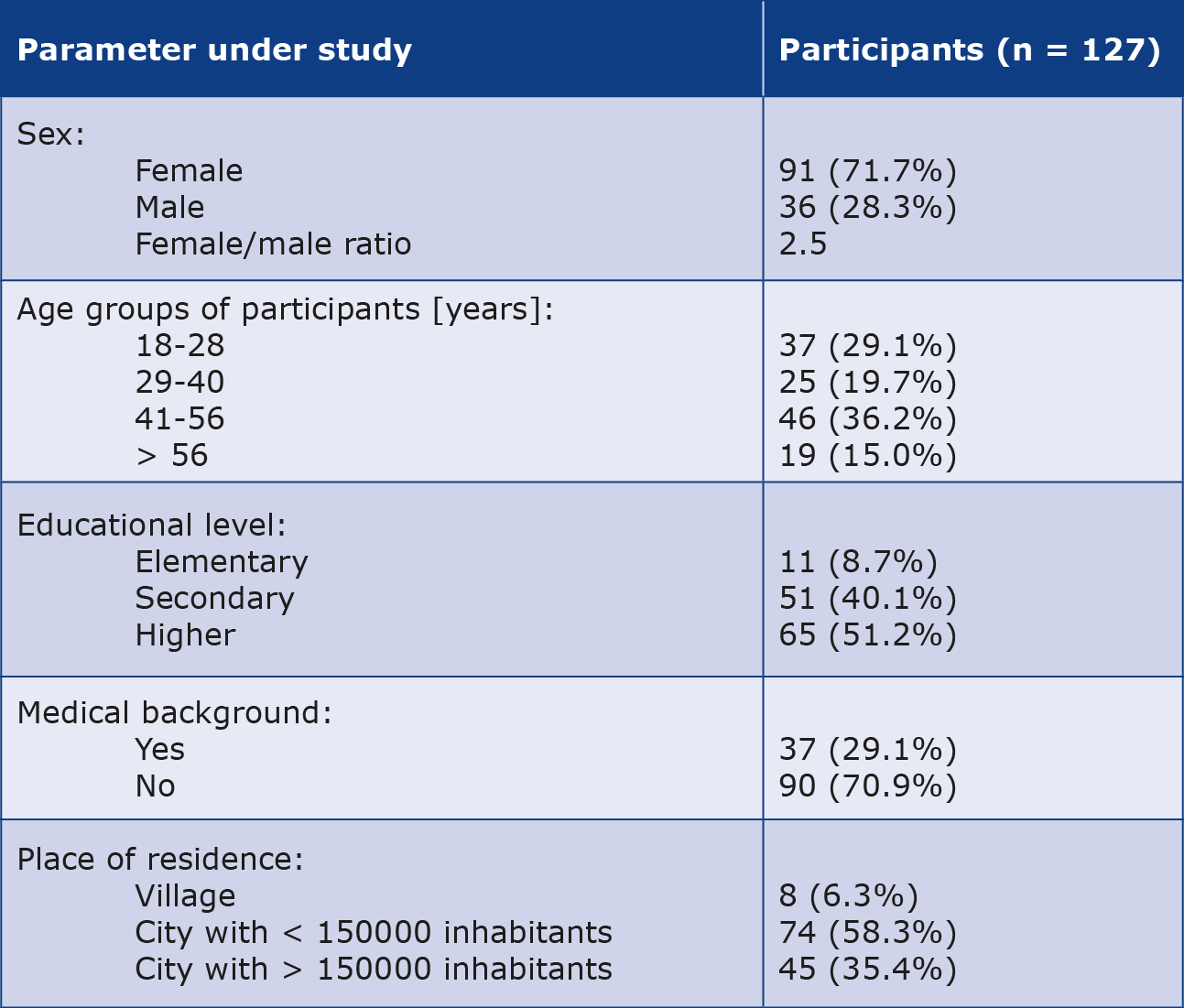
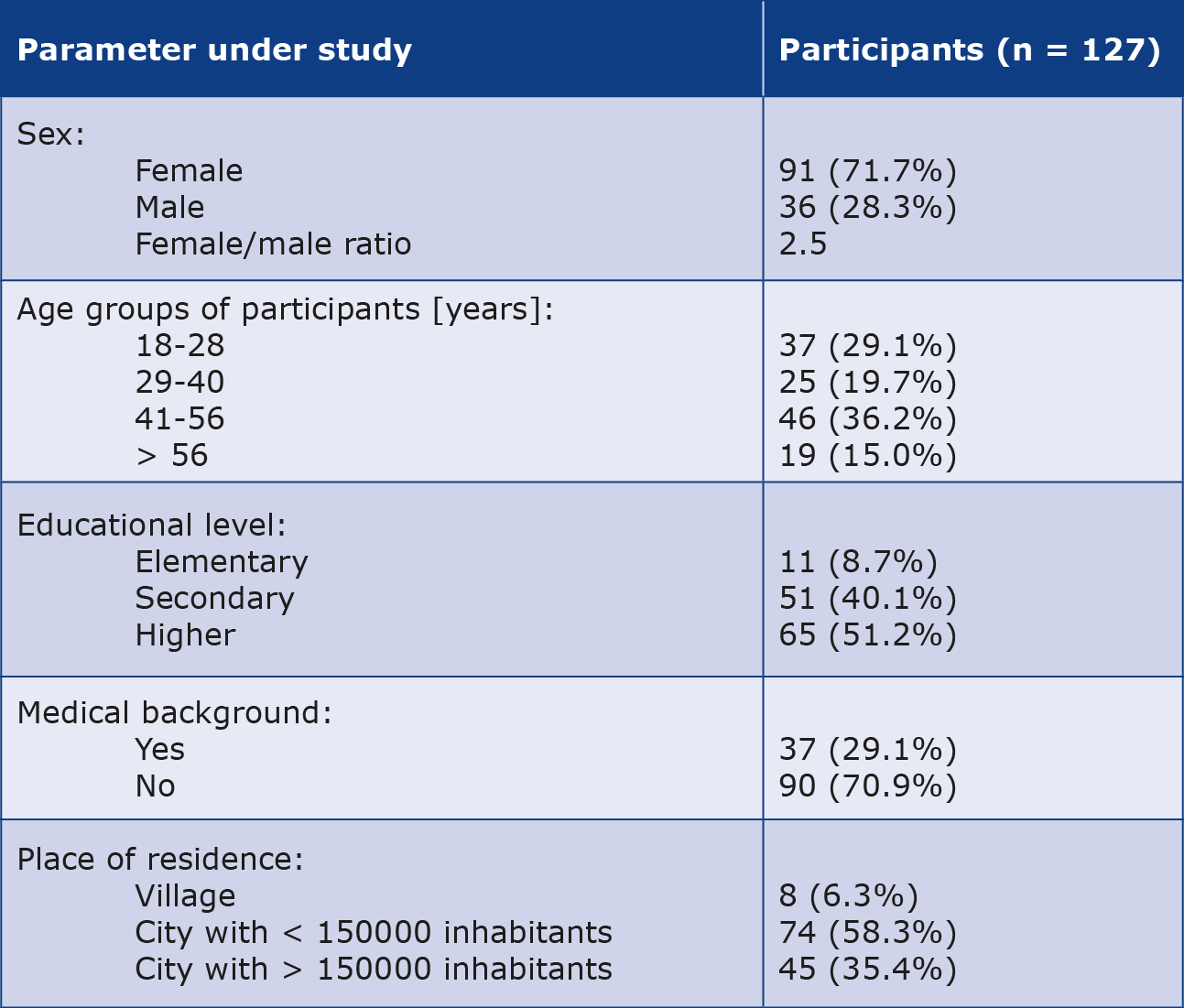
A total of 127 patients agreed to participate and complete the questionnaire. The majority of participants were female (71.7%, n = 91), with the highest proportion within the 41- 50 years of age range (36.2%, n = 46). Furthermore, more than half of the participants had higher education (51.2%, n = 65) and a notable 29% (n = 37) had a medical background, they were either graduates or current students of medical universities. Additional demographic details are provided in Table 1.
Table 1. Background characteristics of respondents
Drugs and diet supplements taken by the participants
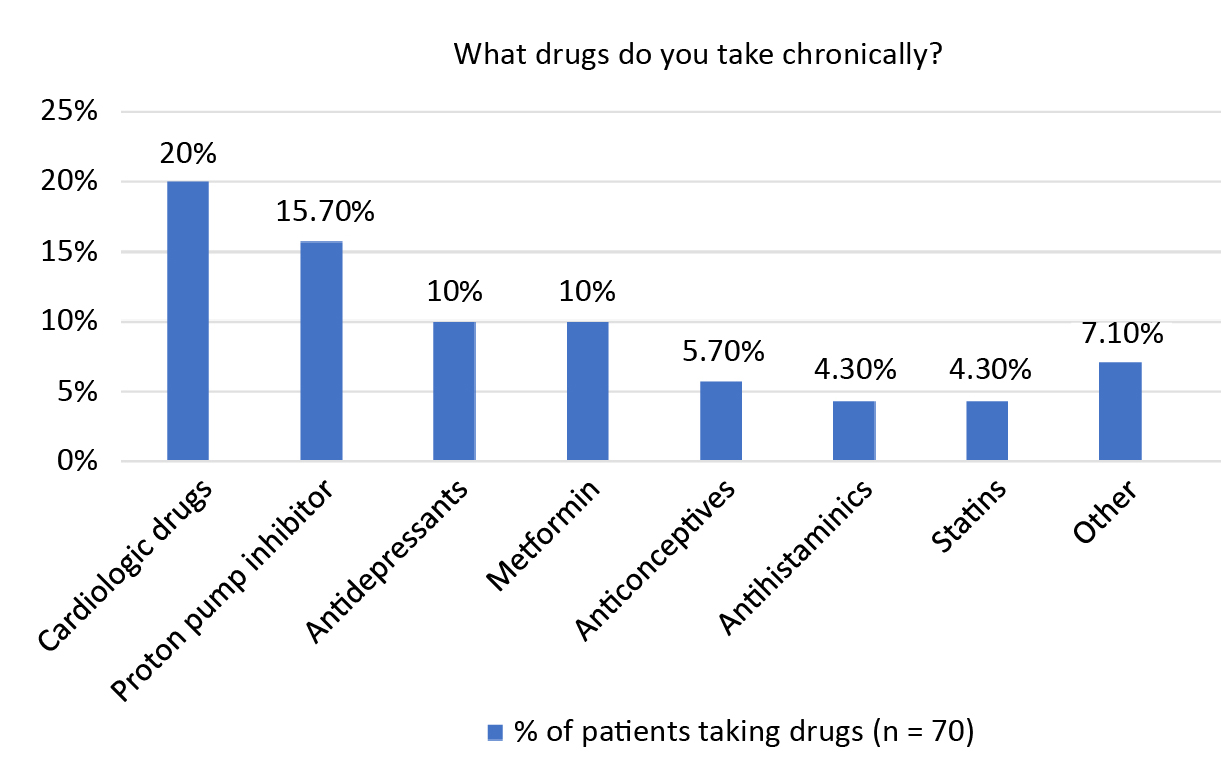
Patients were asked about their chronic illnesses and the prescription medications which they take chronically (> 1 month). Among the respondents, 55% (n = 70) admitted to using prescription drugs regularly (Figure 1). Additionally, 42% of participants (n = 53) acknowledged regular use of OTC drugs and/or dietary supplements. Interestingly, OTC medication and supplement use was more prevalent among younger adults ((78% of the 18-28 years of age group), compared to the rest of the population (p = 0.00000). Moreover, women were found to use OTC drugs and/or dietary supplements more frequently than men (p = 0.00000). The most commonly used supplements included vitamin D (75.5%, n = 40), supplements for hair and nails (18.9%, n = 10) and magnesium (13.2%, n = 7). A notable correlation was observed between sex and specific supplement usage. Specifically, women were more likely than men to take vitamin D (41% versus 8%) (p = 0.00041) and supplements aimed at improving nail and hair the condition (exclusive to women) (p = 0.03824). Furthermore, younger adults aged 18-28 were more likely (70% of this group) to take vitamin D compared to other age groups.
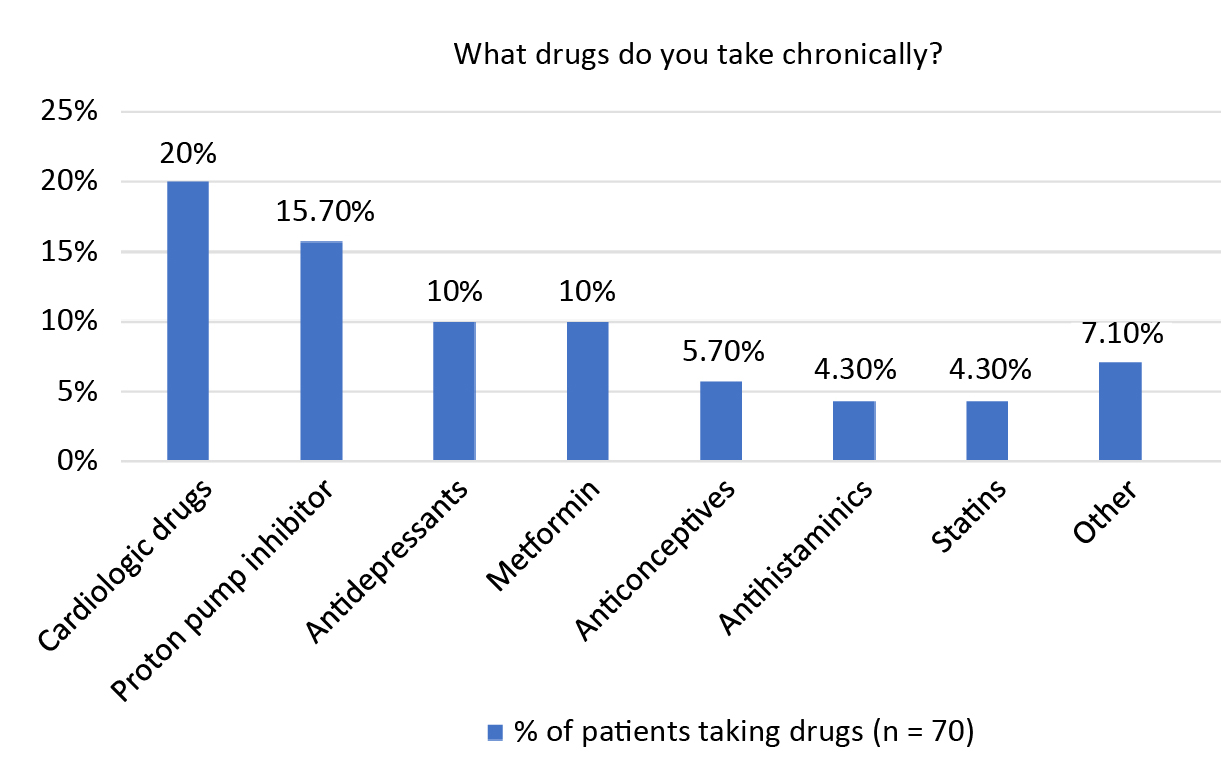
Figure 1. Most common drugs taken chronically by patients
The majority of the patients who took prescription drugs chronically (61.4%, n = 43/70) reported reading the drug leaflet (also known as summary of product characteristics or drug monograph) before use and nearly all patients (99%, n = 69/70) stated that they followed the doctor’s instructions regarding medication intake. Among patients taking OTC or/ and dietary supplements, 70% (n = 37/53) claimed to read the drug’s leaflet before use and all of them (n = 53/53) indicated adherence to either doctor’s or pharmacists’ instructions. Interestingly, women (71%) were more likely than men (39%) to read the leaflets (p = 0.00073).
Drug administration
The vast majority of participants used water to swallow pills: 99% of those taking prescribed drugs (n = 69/70) and 100% of those taking OTC or/and diet supplements (n = 53/53). A small group admitted to using tea (17.1%, n = 12/70 of those taking prescribed drugs and 13.2%, n = 7/53 of those taking OTC or/and dietary supplements) or juice (5.7%, n = 4/70 of those taking prescribed drugs and 9.4%, n = 5/53 of those taking OTC or/and dietary supplements). Interestingly, men were more likely than women to drink tea while taking prescribed drugs (p = 0.01390), although there was no such correlation in the group taking OTC drugs or/and dietary supplements. Furthermore, there was no correlation between sex and drinking juice in either group. Additionally, 45.5% of people > 56 years of age admitted to drinking tea to swallow prescribed pills (p = 0.03499), compared to 13.3% in the 41-56 age group, 0%, in the 29-40 age group and 15.8% in the 18-28 age group. However, there was no such correlation in the group of patients taking OTC or/and dietary supplements. Moreover, there was no correlation between age and drinking juice in either group. Additionally, there was a correlation between the patients’ level of education and their approach to prescribed drug administration. Among patients taking prescribed drugs, 85.7% of respondents with higher education exclusively used water to swallow their medications, while this figure was 81.8% for those with secondary education and only 16.7% for those with primary education (p = 0.00053). Notably, individuals with primary education were more likely to use a different beverage than water to swallow medicines (p = 0.00447). Furthermore, it was found that higher education was associated with a lower likelihood of patients drinking tea with prescribed medications (p = 0.00302).
Interestingly, 30.5% of individuals taking prescription drugs or OTC drugs or dietary supplements (n = 29/95) admitted that they sometimes they took their medication differently than recommended by their doctor or written in the leaflet. This change was primarily driven by convenience (48.3%, n = 14/29) or previous experience with taking medication (48.3%, n = 14/29). However, such behaviour was not associated with sex, age, education level or place of residence.
Knowledge about interactions
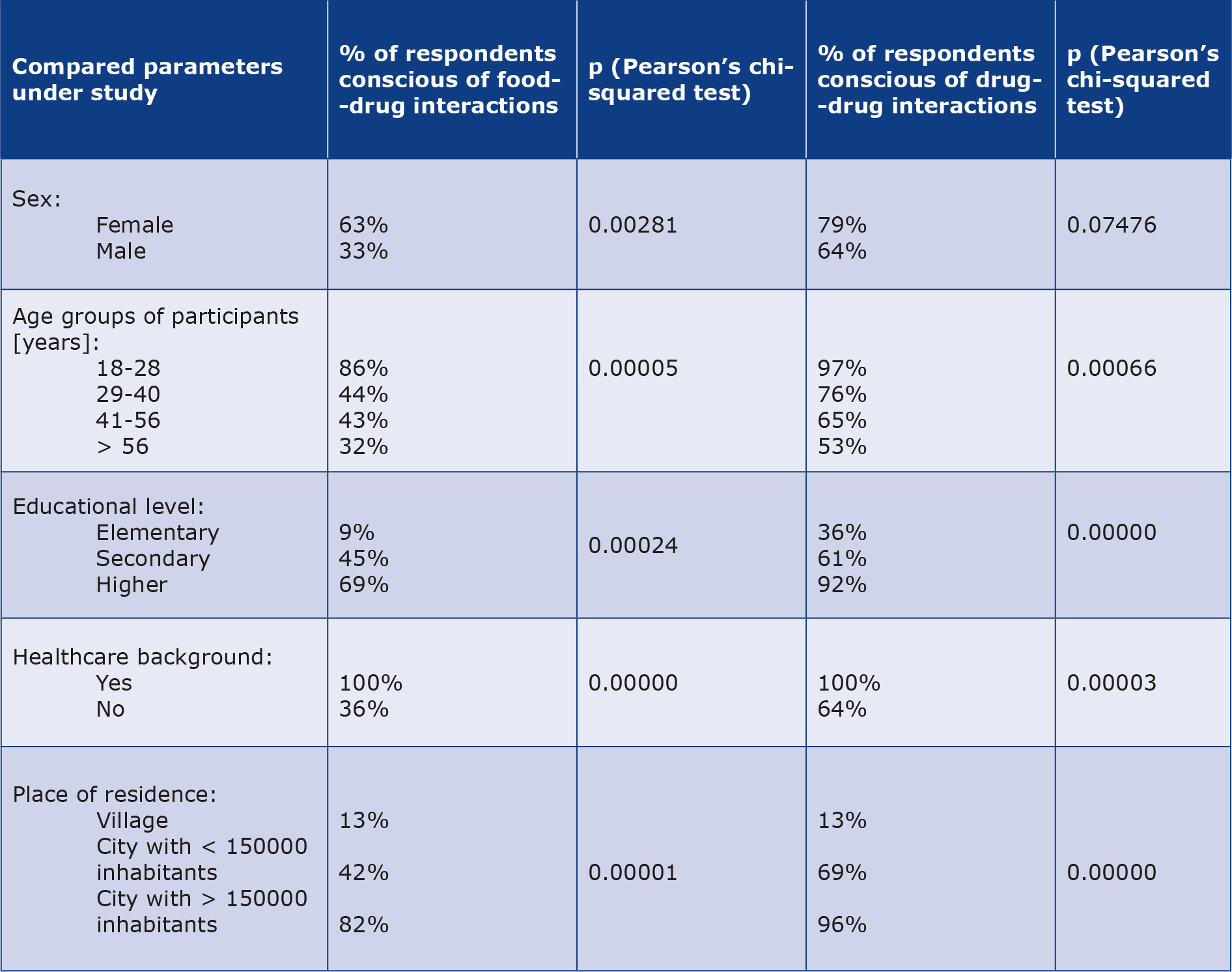
The next segment of the survey focused on participants’ awareness of potential drug-drug and food-drug interactions. It was noted that age, sex, education level and place of residence could influence the patients’ knowledge of these interactions (see Table 2).
Table 2. Awareness of drug-drug and drug-food interactions in selected groups of respondents
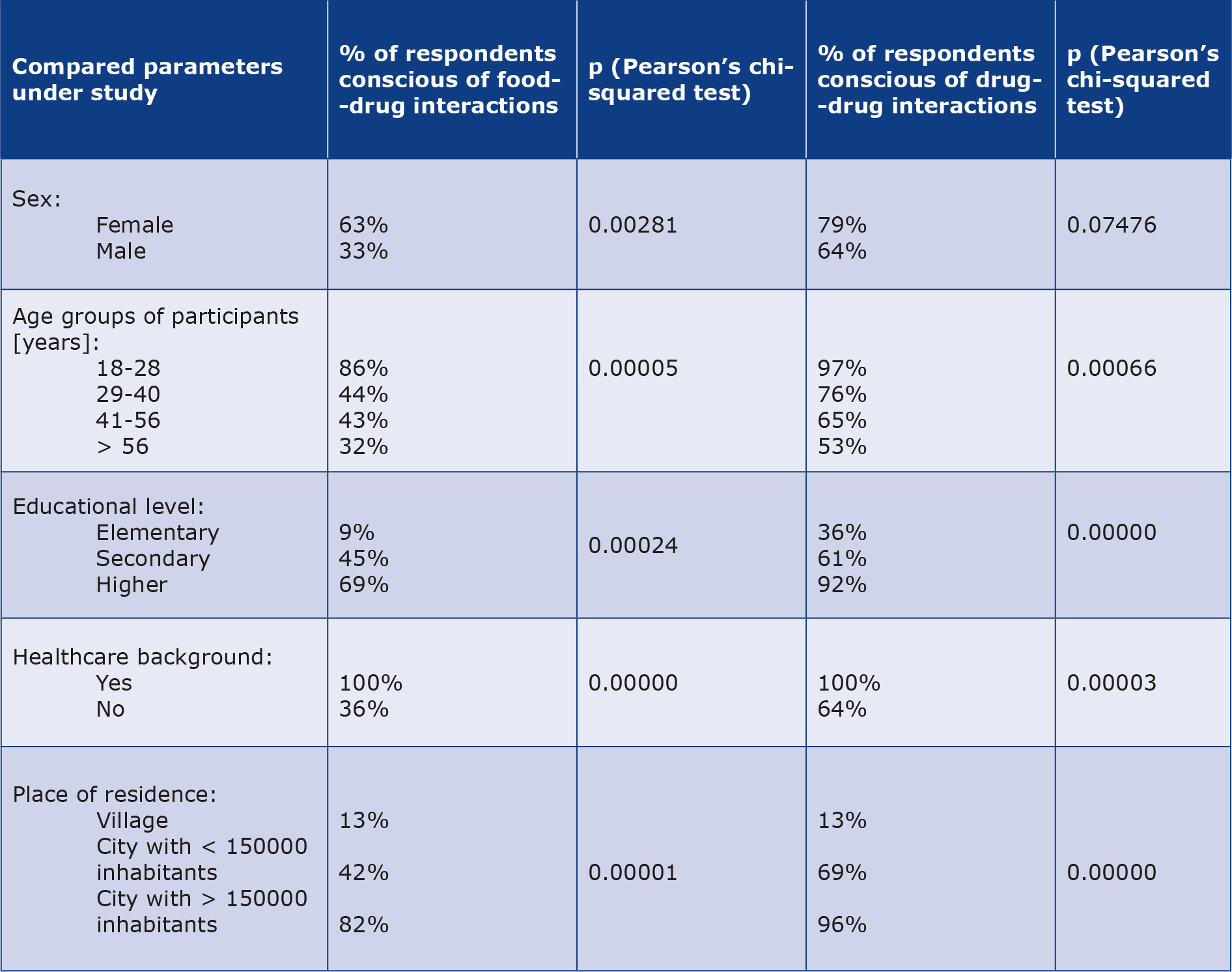
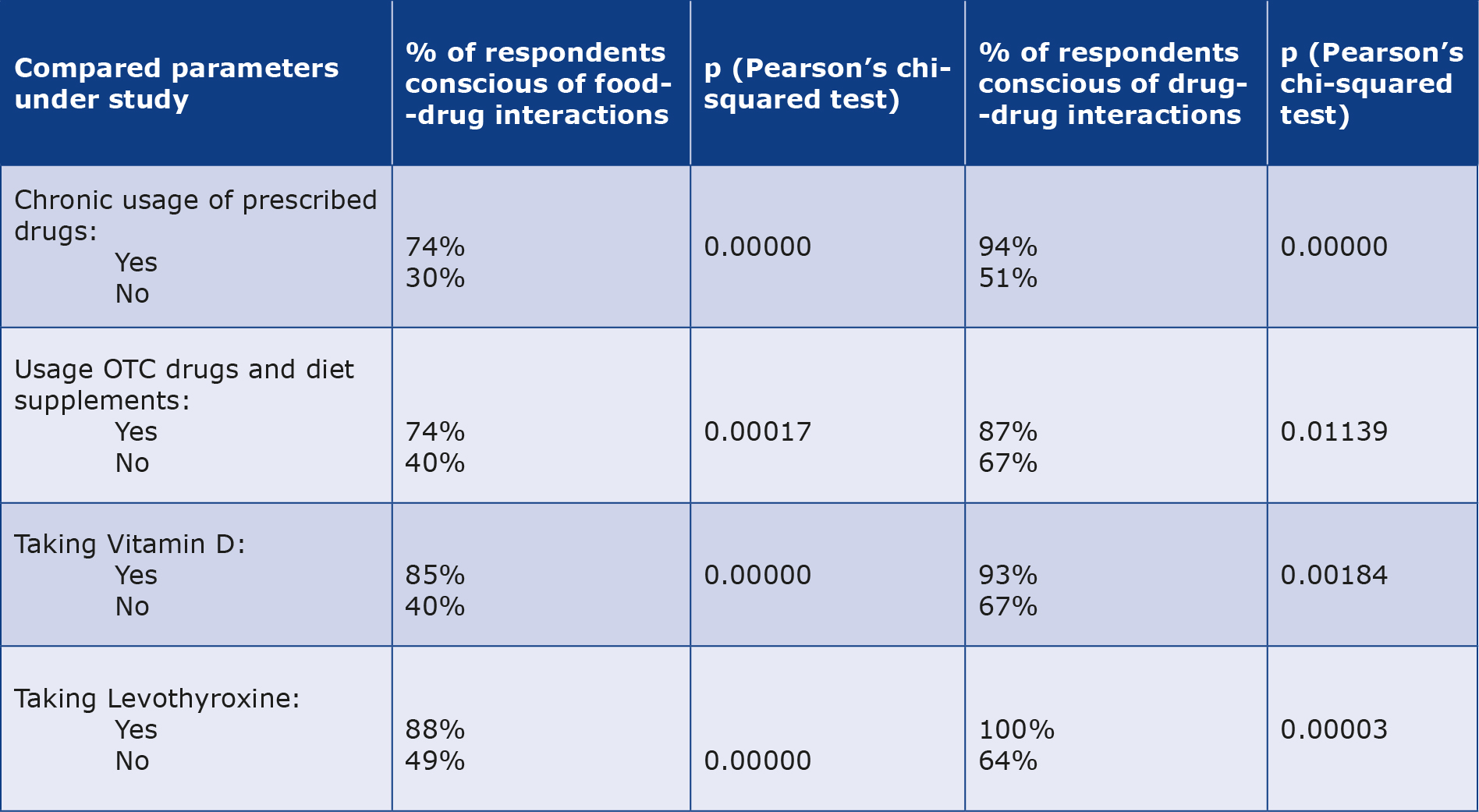
Furthermore, among the respondents who were aware of drug-drug interactions, 72% were also knowledgeable about the potential interactions between drugs and food (p = 0.00000). Interestingly, larger proportions of participants were aware of possible drug-drug interactions compared to interactions between drugs and food (74.8%, n = 95 vs. 54.3%, n = 69). The use of drugs and dietary supplements regularly could enhance the patients’ awareness of both drug-drug and food-drug interactions. For more detailed information, please refer to Table 3.
Table 3. Awareness of drug-drug and drug-food interactions in groups of respondents using various drugs and dietary supplements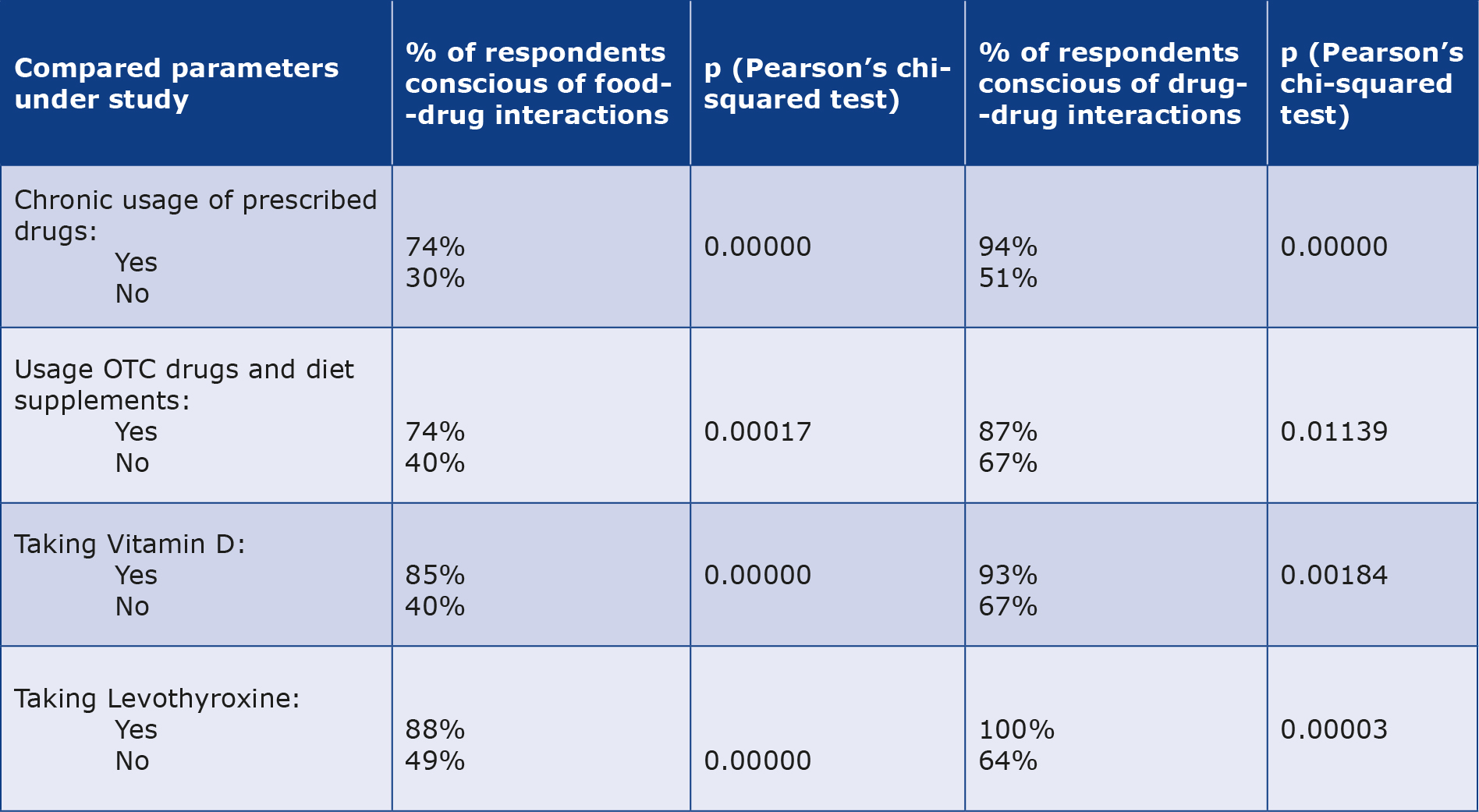
Interestingly, only 7% of the participants who were aware of potential drug-food interactions, admitted to drinking tea while taking pills, compared to 43% in the group lacking this knowledge (p = 0.00000). Additionally, a significant difference was observed in the use of juice with drugs between those who were aware and unaware of drug-food interactions (p = 0.00033), specifically, only 3% of individuals who were aware of the drug-food interactions drank juice with their medication.
Discussion
The primary objective of this study was to evaluate patients’ awareness of potential drug-drug and food-drug interactions. We discovered that such awareness is associated with various demographic factors including age, sex, education level, place of residence and the use of different medications and dietary supplements. In our study 55% of the participants reported taking prescription drugs on a chronic basis and 42% of them claimed taking OTC drugs or/and dietary supplements. The most commonly used medications were cardiovascular drugs (statins and beta-blockers) and proton pump inhibitors, both of which are associated with numerous potential interactions [17].
Interestingly, we found that OTC drug or/and dietary supplement use was more prevalent among the youngest participants (18-28 years of aged). Moreover, a significant majority (70%) of this age group reported taking vitamin D, which was notably more common than in other age groups. Additionally, OTC drugs and/or dietary supplements were more commonly used by women compared to men, mirroring findings of Burnett et al. In their study involving 4895 volunteers in Australia, by 47% of women used supplements, compared to 34% of men [18]. Contrary to our observations, the use of dietary supplements was found to be higher among older individuals and those with higher levels of education [18]. A study conducted in China revealed that only 0.71% of population > 6 years of age admitted to using a dietary supplement [19]. Similarly to the findings of Burnett et al., the prevalence of supplement intake correlated with age and educational level of participants [18]. Interestingly, in our study there we did not observe any statistically significant correlation between the use of OTC drugs and/or dietary supplements and the level of education. A study conducted among medical students in India found that 45.3% of participants (notably more females than males) consumed multivitamin supplements [20]. Similarly, in our study women were more inclined to use supplements for nail and hair health as well as vitamin D. This heightened usage of nail and hair supplements seems to be in line with the common perception that women tend to be more concerned about their appearance than men. The vitamin D supplementation could be linked to the widely announced recommendations for its use in prevention of osteoporosis, a condition more prevalent among women [21].
It is typically the responsibility of the prescribing physician to provide the patients not only with dosage instructions but also to advise on the timing of administration in relation to meals and take into account potential interactions with food and beverages. In our study nearly all (99%) patients who reported taking prescription drugs chronically also stated that they adhered to their doctor’s instructions regarding medication administration. When it comes to OTC drugs or dietary supplements, pharmacist may play a crucial role in clarifying the above-mentioned matters and discussing potential interactions. In our study cohort of patients taking OTC drugs and/ or dietary supplements, all participants indicated that they followed the instructions provided by doctors or pharmacists for medication intake. However, some studies highlighted the inadequate knowledge about drug-drug and drug-food interactions among health care providers. For instance, in the United States, only 18.2% of the 950 surveyed prescribers were able to identify the pairs of drugs that should not be used together [22]. Therefore, it is plausible that information about drug interactions is not consistently conveyed to patients.
In addition to following the instructions provided by a physician or pharmacist, it is important for patients to read the leaflet included with their medication. The information in these leaflets (e.g. details about proper drug administration, correct dosages, contraindications and potential interactions with other drugs or certain foods) should be clear and easy to understand [23]. In our study, the majority of the patients taking prescribed drugs (61.4%) and those using OTC drugs or/and dietary supplements (70%) reported reading the leaflet before starting new medication. Our findings align closely with those reported by Nathan et al. that 70.4% of patients in New York City acknowledged reading a leaflet before using of the new drug (49.2% marked that they “always” read and 21.2% marked “often”). Additionally, 98.8% of patients claimed that reading the leaflet was “very” or “somewhat” useful [24]. In contrast, researchers from Lebanon noted that 61.2% of patients admitted to not reading the leaflets before using drugs [25]. These discrepancies may arise from the fact that in our study we asked patients about reading drug’s leaflets in general, rather than specifically focusing on the leaflets about new drugs. Interestingly, in our study women (71%) were more likely than men (39%) to read the leaflets. However, we did not find any other reports about the correlation between sex and leaflet reading.
We observed that men and particularly more often elderly people drank tea while taking prescribed medications. This can be attributed to the fact that in Poland tea is generally a more popular beverage among the older generation. It is noteworthy that black tea contains caffeine and can potentially interact with many drugs, e.g. psychiatric medications, antiarrhythmics, bronchodilators and antibiotics [26]. These interactions occur because caffeine is metabolised by the same enzyme (cytochrome P450 1A2) as many drugs. Similarly, green tea can interact with drugs such as statins, beta-blockers, warfarin or sildenafil [9]. Therefore, patients should be informed about the potential interactions between drugs and beverages such as coffee, tea or juice. Our study revealed that individuals with higher education levels were less likely to drink tea with prescribed medicines. This highlights the need to educate patients about drug-beverage interactions to avoid adverse effects.
We observed that women, younger adults (aged 18-28), individuals with higher education level and those residing in urban areas exhibited greater awareness of potential drugdrug and food-drug interactions. Moreover, awareness regarding drug interactions, both with other medications and with food, was higher among the patients who chronically took medications, regardless if these were prescribed (particularly levothyroxine), OTC drugs or dietary supplements (particularly vitamin D). Additionally, participants with background in healthcare (e.g. healthcare workers or medical university students) demonstrated greater awareness of drugdrug and food-drug interactions, which may be attributed to their basic knowledge of biochemistry and pharmacology.
Indeed, enhancing patient knowledge about medications can significantly improve treatment compliance. In our study, we found than only 7% of individuals aware of potential drug-food interactions consumed tea while swallowing pills, compared to 43% of those who were unaware of such interactions. This underscores the importance of educating patients about potential interactions in order to mitigate the risk of adverse effects. Numerous studies in the literature support the positive impact of patient education on medication management. For instance, Detry-Morel reported that improved efforts to inform patients with open-angle glaucoma or ocular hypertension led to better compliance and persistence with therapy resulting in fewer medication errors and improved efficacy [27]. Similarly, Micheli et al. concluded that patients with better understanding of why they were taking a particular medication were less likely to discontinue treatment [28]. Kristensson et al. highlighted the critical importance of informing patients about their prescribed medications, even in acute care settings [29]. Furthermore, it is essential that the information provided to patients is clear and understandable. Gustafsson et al. found that while most information was well understood by patients, the sections concerning ‘risks of interactions’ and ‘contraindications’ were challenging, particularly for the elderly patients [30]. This underscores the fact that in order to mitigate the risk of interactions, patients must have a comprehensive understanding of their medications. First, patients must be aware that such interactions are possible, which empowers them to inquire about this with their physicians and consequently, they can actively participate in their own healthcare decisions. However, a study from Lebanon revealed that 38.7% of participants did not regularly discuss their medications with physicians and 53.9% did not enquire about potential interactions with pharmacist. In our research, a better understanding of both drug-drug and food-drug interactions was associated with female sex, higher education, medical background and chronic medication use. These findings are consistent with the survey conducted in Saudi Arabia, which reported the participants’ knowledge of food-drug interactions as moderate, with higher knowledge linked to female sex, healthcare-related occupations with and the presence of chronic disease [31]. Similarly, in a study conducted in South Africa, only 30-50% of patients were able to identify potential food-drug interactions [32]. The patients in that study had a secondary or lower level of education, which aligns with our findings, where only 45% of respondents with secondary education and 9% of those with elementary education were aware of food-drug interactions.
Our study has some limitations. The study group was relatively small and homogenous (participants come from only one region of one country). Moreover, some patients missed their appointments, resulting in a smaller number of participants and completed questionnaires than we intended (based on our calculations of optimal sample size). Additionally, as with most questionnaire-based studies, there is a risk that respondents provided answers based on what they believed to be correct rather than on their true knowledge. To obtain more representative data and a deeper understanding of public’s knowledge about this subject, it would be beneficial to conduct similar surveys across various regions with more detailed questions. Furthermore, longitudinal studies that include consultations on food-drug interactions could help track changes in awareness and behaviour over time, as well as evaluate the effectiveness of patient education.
Conclusion
Our study revealed a moderate level of awareness regarding drug-drug and food-drug interactions among Polish adults, with notable correlations observed with sex, educational level and chronic medication usage. It is worth to emphasise the role of patients’ education as the best way to enhance the awareness of drug interactions and to mitigate potential health risks associated with improper medication use. Introducing basic knowledge about medication usage into primary and secondary school curricula could help to educate future adults, while medical university students should receive more comprehensive training on this topic. Furthermore, eHealth platforms and applications could be introduced to improve both the awareness and knowledge about potential drug interactions [33].
Acknowledgement
We would like to acknowledge and thank all the patients who participated in our survey study.
Conflicts of interest
The authors declare that no conflicts of interest exist.
Funding
None.
Availability of data and materials
The corresponding author is committed to share collected data upon request. All data are anonymized to respect the privacy of patients who participated in this study.
Supplementary materials
The questionnaire developed for this study (in Polish language).
References
| 1. |
Benet LZ, Bowman CM, Koleske ML, Rinaldi CL, Sodhi JK. Understanding drug–drug interaction and pharmacogenomic changes in pharmacokinetics for metabolized drugs. J Pharmacokinet Pharmacodyn [Internet]. 2019;46:155–63. Available from: https://pubmed.ncbi.nlm.nih.gov/30911879/.
|
| 2. |
Zhang T, Leng J, Liu Y. Deep learning for drug-drug interaction extraction from the literature: a review. Brief Bioinform [Internet]. 2020;21:1609–27. Available from: https://doi.org/10.1093/bib/bbz087.
|
| 3. |
Spanakis M, Melissourgaki M, Lazopoulos G, Patelarou AE, Patelarou E. Prevalence and Clinical Significance of Drug-Drug and Drug-Dietary Supplement Interactions among Patients Admitted for Cardiothoracic Surgery in Greece. Pharmaceutics [Internet]. 2021;13:239. Available from: https://www.mdpi.com/1999-4923/13/2/239.
|
| 4. |
Scherf-Clavel O. Drug-Drug Interactions With Over-The-Counter Medicines: Mind the Unprescribed. Ther Drug Monit [Internet]. 2022;44:253–74. Available from: https://journals.lww.com/10.1097/FTD.0000000000000924.
|
| 5. |
Schmidt LE, Dalhoff K. Food-Drug Interactions. Drugs [Internet]. 2002;62:1481–502. Available from: http://link.springer.com/10.2165/00003495-200262100-00005.
|
| 6. |
Bailey DDG, Dresser GK. Interactions Between Grapefruit Juice and Cardiovascular Drugs. Am J Cardiovasc Drugs [Internet]. 2004;4:281–97. Available from: https://doi.org/10.2165/00129784-200404050-00002.
|
| 7. |
Boullata JI, Hudson LM. Drug-Nutrient Interactions: A Broad View with Implications for Practice. J Acad Nutr Diet [Internet]. 2012;112:506–17. Available from: https://www.sciencedirect.com/science/article/pii/S0002822311015446.
|
| 8. |
Pawłowska I, Kuźbicka K, Krzyżaniak N, Kocić I. Interactions between selected over-the-counter drugs and food: clinical relevance and prevention. Int J Food Sci Nutr. Int J Food Sci Nutr; 2022;73:1005–18.
|
| 9. |
Werba JP, Misaka S, Giroli MG, Shimomura K, Amato M, Simonelli N, et al. Update of green tea interactions with cardiovascular drugs and putative mechanisms. J Food Drug Anal [Internet]. J Food Drug Anal; 2018;26:S72–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S102194981830036X.
|
| 10. |
Salminen WF, Yang X, Shi Q, Greenhaw J, Davis K, Ali AA. Green tea extract can potentiate acetaminophen-induced hepatotoxicity in mice. Food Chem Toxicol [Internet]. 2012;50:1439–46. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0278691512000543.
|
| 11. |
Bailey DG, Malcolm J, Arnold O, David Spence J. Grapefruit juice-drug interactions. Br J Clin Pharmacol [Internet]. Br J Clin Pharmacol; 1998;46:101–10. Available from: https://bpspubs.onlinelibrary.wiley.com/doi/10.1046/j.1365-2125.1998.00764.x.
|
| 12. |
Chen M, Zhou S, Fabriaga E, Zhang P, Zhou Q. Food-drug interactions precipitated by fruit juices other than grapefruit juice: An update review. J Food Drug Anal [Internet]. 2018;26:S61–71. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1021949818300371.
|
| 13. |
Cheng Y, Lin B-J, Guo J-H, Huang B-L, Fang L-P, Que W-C, et al. The Effect Of Food On The Pharmacokinetic Properties And Bioequivalence Of Two Formulations Of Levocetirizine Dihydrochloride In Healthy Chinese Volunteers. Drug Des Devel Ther [Internet]. 2019;Volume 13:3625–34. Available from: https://www.dovepress.com/the-effect-of-food-on-the-pharmacokinetic-properties-and-bioequivalenc-peer-reviewed-article-DDDT.
|
| 14. |
Sostek MB, Chen Y, Andersson T. Effect of timing of dosing in relation to food intake on the pharmacokinetics of esomeprazole. Br J Clin Pharmacol [Internet]. 2007;64:386–90. Available from: https://bpspubs.onlinelibrary.wiley.com/doi/10.1111/j.1365-2125.2007.02889.x.
|
| 15. |
Walle T, Fagan TC, Walle UK, Oexmann M-J, Conradi EC, Gaffney TE. Food-induced increase in propranolol bioavailability – Relationship to protein and effects on metabolites. Clin Pharmacol Ther [Internet]. Clin Pharmacol Ther; 1981;30:790–5. Available from: http://doi.wiley.com/10.1038/clpt.1981.239.
|
| 16. |
Rainsford KD, Bjarnason I. NSAIDs: take with food or after fasting? J Pharm Pharmacol [Internet]. 2012;64:465–9. Available from: https://academic.oup.com/jpp/article/64/4/465-469/6135247.
|
| 17. |
Stark JE, Montgomery CM. Administering a Soda Beverage With the Hepatitis C Treatment Sofosbuvir/Velpatasvir and the Proton-Pump Inhibitor Pantoprazole: A Case Report. J Pharm Pract [Internet]. 2024;37:1011–4. Available from: https://journals.sagepub.com/doi/10.1177/08971900231183036.
|
| 18. |
Burnett A, Livingstone K, Woods J, McNaughton S. Dietary Supplement Use among Australian Adults: Findings from the 2011–2012 National Nutrition and Physical Activity Survey. Nutrients [Internet]. Nutrients; 2017;9:1248. Available from: https://www.mdpi.com/2072-6643/9/11/1248.
|
| 19. |
Gong W, Liu A, Yao Y, Ma Y, Ding C, Song C, et al. Nutrient Supplement Use among the Chinese Population: A Cross-Sectional Study of the 2010-2012 China Nutrition and Health Surveillance. Nutrients [Internet]. Nutrients; 2018;10:1733. Available from: https://www.mdpi.com/2072-6643/10/11/1733.
|
| 20. |
Joseph N, Kumar A, Singh H, Shaheen M, Das K, Shrivastava A. Nutritional Supplement and Functional Food Use Among Medical Students in India. J Diet Suppl [Internet]. J Diet Suppl; 2018;15:951–64. Available from: https://www.tandfonline.com/doi/full/10.1080/19390211.2017.1407384.
|
| 21. |
Poirier J-L, Wurtz LD, Collier CD. Increased Number of Medical Comorbidities Associated With Increased Risk of Presenting With Pathological Femur Fracture in Metastatic Bone Disease. Iowa Orthop J [Internet]. University of Iowa; 2023;43:87–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/37383878.
|
| 22. |
Ko Y, Malone DC, Skrepnek GH, Armstrong EP, Murphy JE, Abarca J, et al. Prescribers??? Knowledge of and Sources of Information for Potential??Drug-Drug Interactions. Drug Saf [Internet]. Drug Saf; 2008;31:525–36. Available from: http://link.springer.com/10.2165/00002018-200831060-00007.
|
| 23. |
Tran MT, Grillo JA. Translation of Drug Interaction Knowledge to Actionable Labeling. Clin Pharmacol Ther [Internet]. Clin Pharmacol Ther; 2019;105:1292–5. Available from: https://ascpt.onlinelibrary.wiley.com/doi/10.1002/cpt.1427.
|
| 24. |
Nathan JP, Zerilli T, Cicero LA, Rosenberg JM. Patients’ Use and Perception of Medication Information Leaflets. Ann Pharmacother [Internet]. Ann Pharmacother; 2007;41:777–82. Available from: https://journals.sagepub.com/doi/10.1345/aph.1H686.
|
| 25. |
Ramia E, Zeenny RM, Hallit S, Salameh P. Assessment of patients’ knowledge and practices regarding their medication use and risks in Lebanon. Int J Clin Pharm [Internet]. Int J Clin Pharm; 2017;39:1084–94. Available from: http://link.springer.com/10.1007/s11096-017-0517-4.
|
| 26. |
Carrillo JA, Benitez J. Clinically Significant Pharmacokinetic Interactions Between Dietary Caffeine and Medications. Clin Pharmacokinet [Internet]. Clin Pharmacokinet; 2000;39:127–53. Available from: http://link.springer.com/10.2165/00003088-200039020-00004.
|
| 27. |
Detry-Morel M. Compliance et persistance. J Fr Ophtalmol [Internet]. J Fr Ophtalmol; 2006;29:216–25. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0181551206737755.
|
| 28. |
Micheli P, Gerstel E. Patients’ knowledge of drug treatments after hospitalisation: the key role of information. Swiss Med Wkly [Internet]. Swiss Med Wkly; 2007;137:614–20. Available from: https://smw.ch/index.php/smw/article/view/790.
|
| 29. |
Kristensson J, Modig S, Midlöv P, Hallberg IR, Jakobsson U. Healthcare utilisation and knowledge concerning prescribed drugs among older people. Eur J Clin Pharmacol [Internet]. Eur J Clin Pharmacol; 2010;66:1047–54. Available from: http://link.springer.com/10.1007/s00228-010-0837-y.
|
| 30. |
Gustafsson J, Kälvemark S, Nilsson G, Nilsson JLG. Patient information leaflets — patients’ comprehension of information about interactions and contraindications. Pharm World Sci [Internet]. Pharm World Sci; 2005;27:35–40. Available from: http://link.springer.com/10.1007/s11096-005-1413-x.
|
| 31. |
Zaidi SF, Mgarry R, Alsanea A, Almutairi SK, Alsinnari Y, Alsobaei S, et al. A Questionnaire-Based Survey to Assess the Level of Knowledge and Awareness about Drug–Food Interactions among General Public in Western Saudi Arabia. Pharmacy [Internet]. Multidisciplinary Digital Publishing Institute (MDPI); 2021;9:76. Available from: https://www.mdpi.com/2226-4787/9/2/76.
|
| 32. |
Osuala EC, Tlou B, Ojewole EB. Knowledge, attitudes, and practices towards drug-food interactions among patients at public hospitals in eThekwini, KwaZulu-Natal, South Africa. Afr Health Sci [Internet]. 2022;22:681–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/36032453.
|
| 33. |
Spanakis M, Sfakianakis S, Kallergis G, Spanakis EG, Sakkalis V. PharmActa: Personalized pharmaceutical care eHealth platform for patients and pharmacists. J Biomed Inform [Internet]. 2019;100:103336. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1532046419302552.
|