Comparison of the use of non-antibiotic drugs with antibiotics in postoperative circumcision wound healing: a systematic review
Abstract
Circumcision is one of the most commonly performed operations. It is common to use of antibiotics to prevent complications after circumcision. However, as awareness of antibiotic resistance increases, it is necessary to consider using other prophylactic drugs. This review aims to evaluate non-antibiotic drugs for wound healing after circumcision. We conducted a literature search in accordance with the PRISMA guidelines using Google Scholar, PubMed, and ScienceDirect search engines to find treatment intervention studies comparing circumcision wound healing outcomes and adverse effects after non-antibiotic topical drugs and antibiotics. A total of 2 studies with 636 participants matched our inclusion criteria. 2-octyl cyanoacrylate and nanosilver gel (AgNPs) were used for post-circumcision wound treatment. The group with topical non-antibiotic drugs had a lower healing rate. There was no significant difference between wound healing and significant adverse effects between drug comparisons. Antibiotic resistance tests between intervention and control groups were not included in these studies. Data comparing non-antibiotic drugs and antibiotics for post-circumcision wound healing are still limited. Further studies conducted in various settings are needed to assess the efficacy of non-antibiotic topical agents for post-circumcision wound healing and reducing antibiotic resistance.
Citation
Kafalah U K, Adnan M L. Comparison of the use of non-antibiotic drugs with antibiotics in postoperative circumcision wound healing: a systematic review. Eur J Transl Clin Med. 2024;7(1):79-86Introduction
Circumcision, one of the most ancient surgical procedures known to humanity, has been performed for a variety of cultural, religious and medical reasons [1]. Circumcision is often performed on male children because of lower risks and costs, less postoperative discomfort and a shorter healing period compared to adults [1]. In the uncircumcised condition, the prepuce (commonly referred to as foreskin) is a warm and moist environment where pathogens can potentially survive and reproduce [1]. The foreskin can be subject to micro abrasion, which increases the risk of acquisition and transmission of pathogens [1]. Although circumcision can reduce the risk of infection in children, in adults this procedure can have an impact on sexual function and lead to male body dysmorphia [2]. More studies are needed regarding the benefits of circumcision in various background conditions [2].
Possible complications following circumcision include bleeding, infection, excessive skin removal, recurring phimosis, epithelial inclusion cysts, penile adhesions and meatal stenosis [3]. Some complication such as bleeding, ring device removal and infection are more common in non-therapeutic circumcision, while meatal stenosis and adhesion are common in therapeutic circumcision [4]. Effective approaches to reduce the risk of complications include strict asepsis during surgery, avoiding the risk of contact with non-communicable diseases, pre-operative and post-operative therapy after circumcision and providing a sterile and hygienic environment [3]. Circumcision is considered a clean surgical procedure with a low risk of wound infection, but in some parts of the world antibiotics are prescribed as prophylaxis despite the additional costs and lack of guidelines [5]. It is noteworthy that antibiotics are indicated for patients with urological abnormalities such as vesicoureteric reflux (VUR), who are undergoing circumcision [6].
While the surgical aspects of circumcision are well-documented and standardized, the post-operative care and the use of topical treatments for wound healing and prevent complications continue to be areas of ongoing research and clinical interest [4]. In recent years, there has been an increasing focus on the use of creams in post-circumcision care [7]. Nevertheless, there is a lack of specific data regarding the avoidance of topical antimicrobials after this procedure. Improper use of antibiotics can contribute to antibiotic resistance, therefore the use of non-antibiotic products has been explored [8]. This systematic review aims to thoroughly examine the existing body of literature to assess the effectiveness and safety of medication options for post-circumcision treatment, with a particular focus on both antibiotic and non-antibiotic creams. Through a critical analysis of available evidence, our goal is to offer insights for healthcare providers, patients and researchers.
Material and methods
We conducted a literature search using the PubMed, Google Scholar and ScienceDirect databases between September 2023 and October 2023, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta- -Analysis (PRISMA) guideline [9]. We used the following keywords: “ointment”, “wound healing,” “after circumcision”, “comparative studies” and “post circumcision”. Combine keywords using “AND” and “OR” to expand or narrow the search. The literature search was based on the following PICO framework: Patient (elective circumcision patients), Intervention (ointments other than antibiotics), Comparison (with antibiotic ointments) and Outcome (the wound healing outcomes reported in the particular study).
The inclusion criteria applied in this search were: intervention studies (randomized and non-randomized), full-text articles written in English language, published within the last 10 years, elective circumcision regardless of surgical method, a comparison of topical treatment for circumcision wounds and reporting relevant clinical outcomes (e.g. wound infection rates, wound closure time, wound complications and patient-reported outcomes). Conversely, the exclusion criteria were: review articles, systematic reviews, meta-analyses, lack of full-text articles, non-intervention studies, duplicate publications or overlapping data from the same study population and any other publications not in English, animal studies, lacking clear comparison between topical non-antibiotic drugs and antibiotics, treatment with oral antibiotics and insufficient data on wound healing outcomes.
We extracted the following data from the articles: study type, year of publish, study location, language, sample size, follow-up period, patients (sex, number, mean of age, inclusion-exclusion criteria, comorbidities), intervention (length of study, type of intervention and control, route of administration and dosage), comparison (antibiotic versus non-antibiotic drug) and outcome (time to recovery, quality of recovery, infection rate, closure time and patient-reported outcomes and adverse outcomes). After all data were extracted, we assessed the risk of bias of the study using Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB-2) [10]. When there were differing results, two authors discuss the study together.
Results
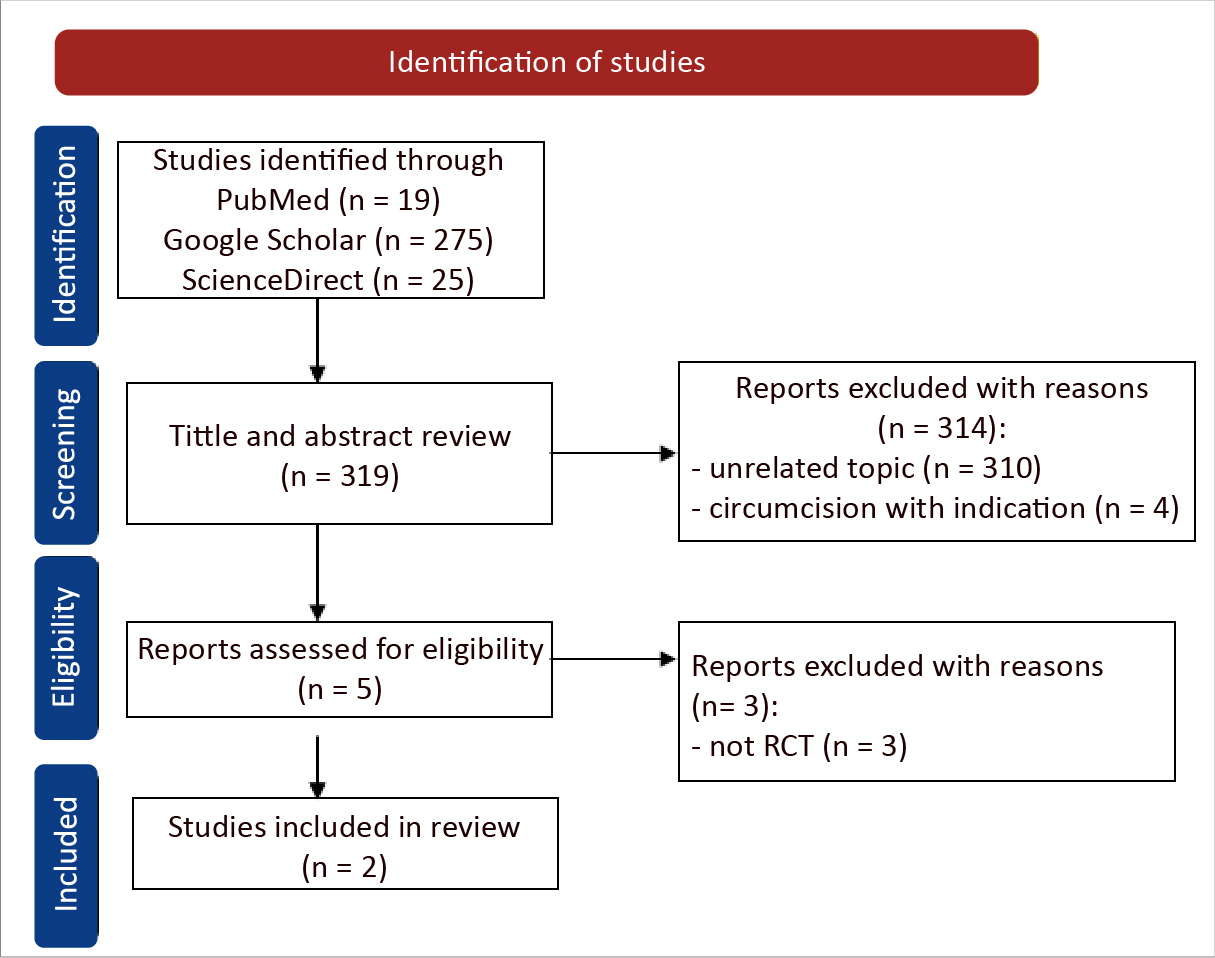
In the literature search we identified a total of 319 studies. Out of these, 314 studies were excluded due to various reasons, e.g. the unavailability of full-text articles, study type (reviews, systematic reviews, meta-analyses, case studies). Most of the studies retrieved were focused on human subjects and discussed the effects observed after the intervention. Following a comprehensive review, we found two studies that met the inclusion criteria (Figure 1).
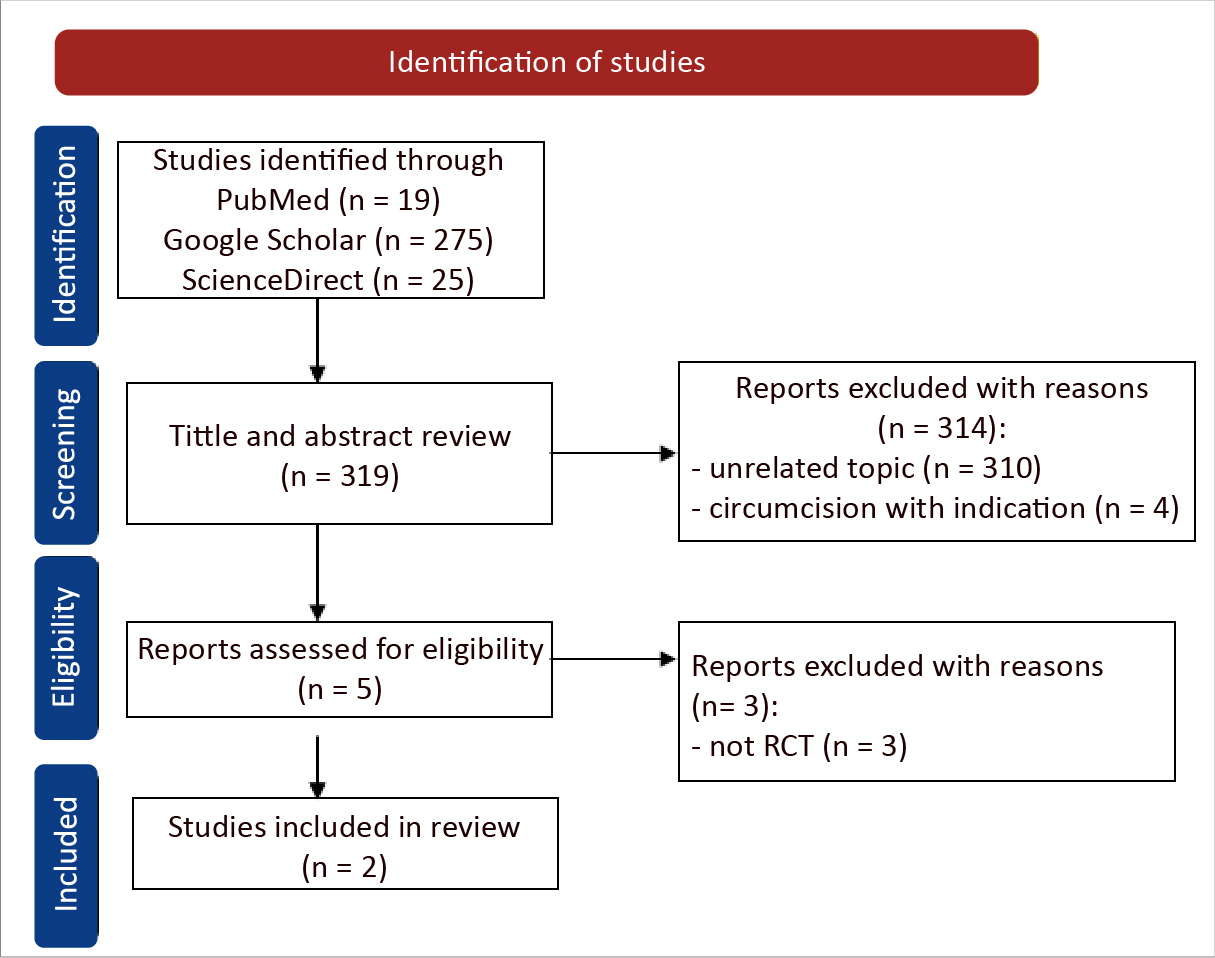
Figure 1. PRISMA flowchart of our systematic review
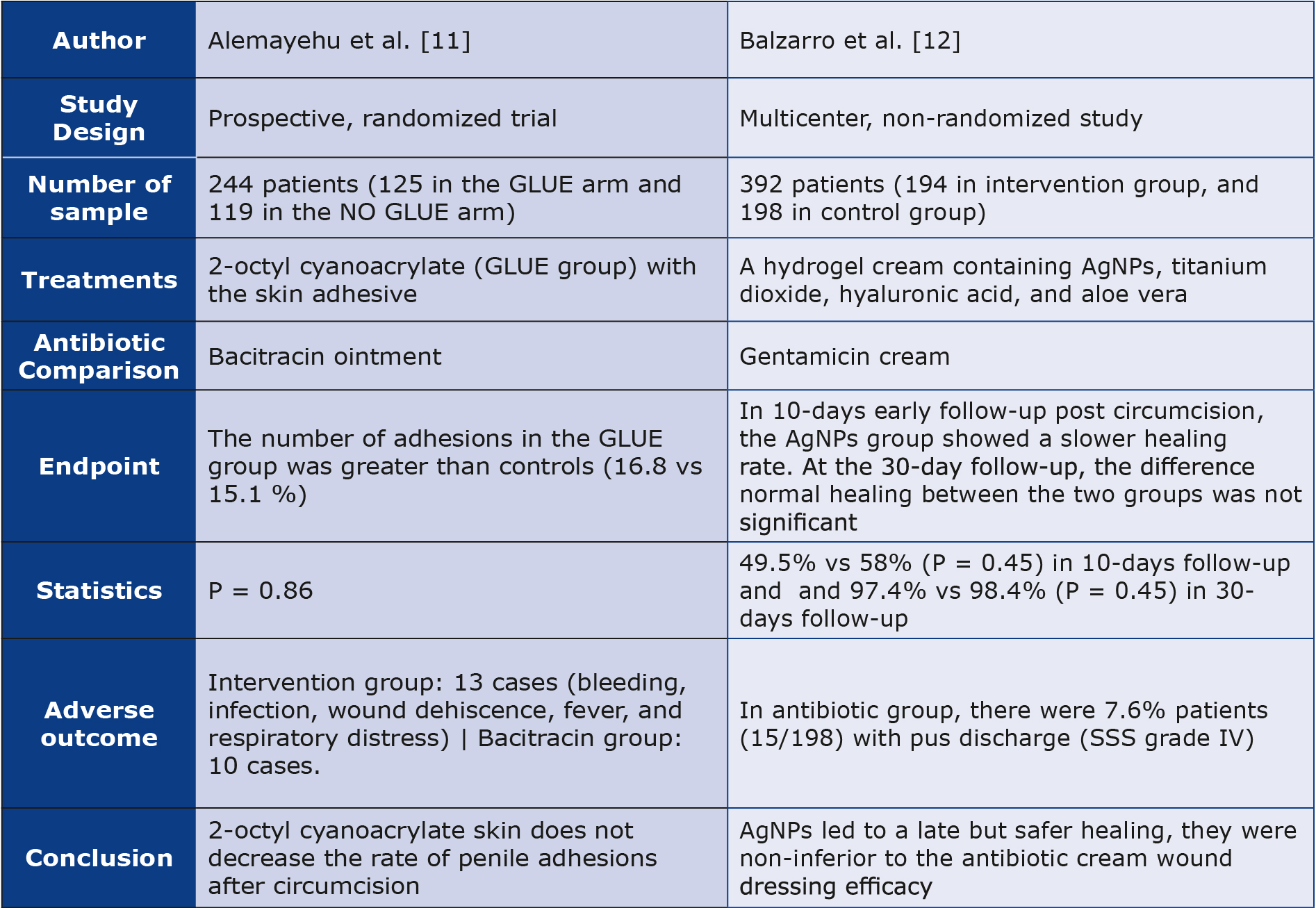
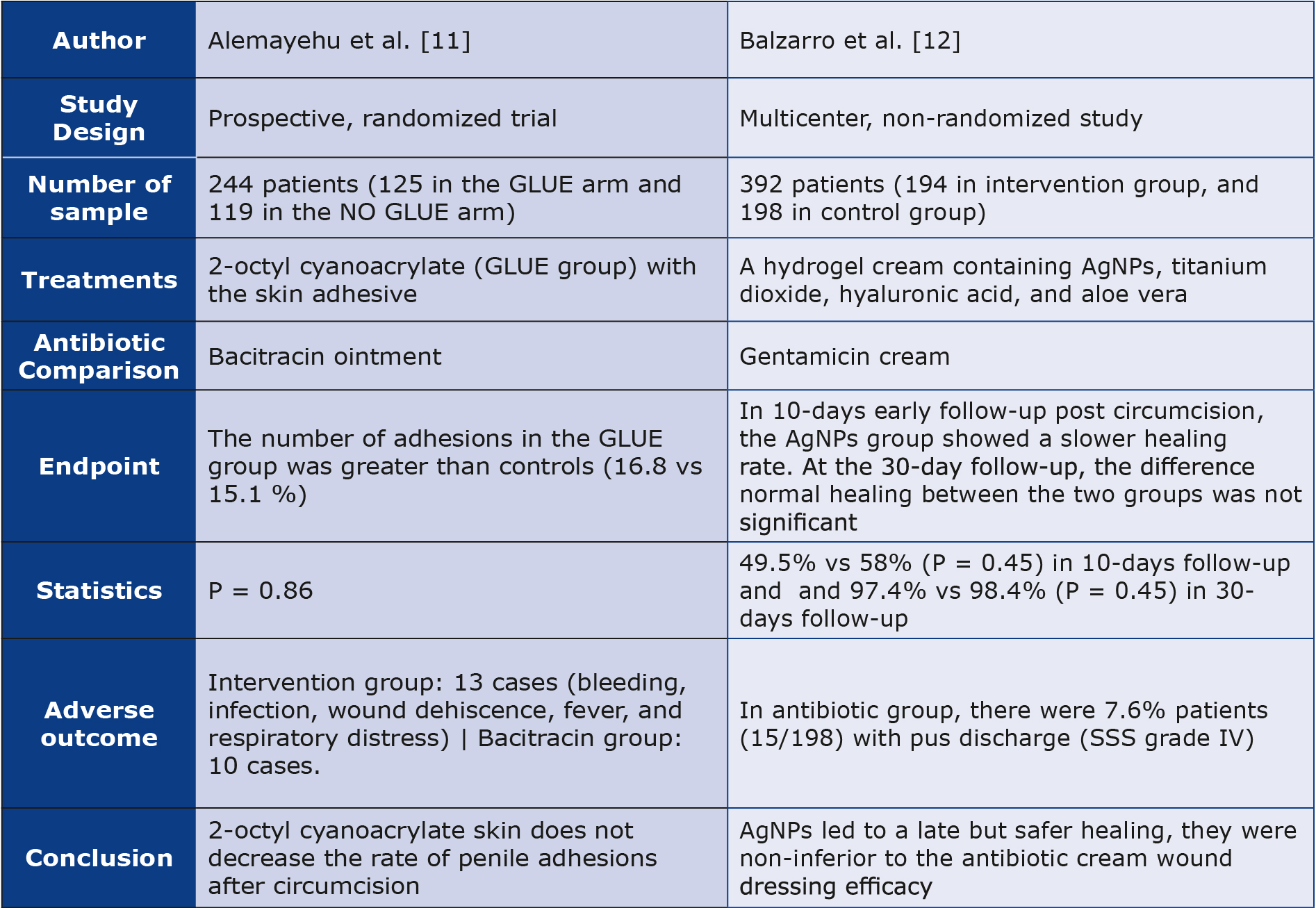
Of the 2 studies that were included, Alemayehu et al. compared 2-octyl cyanoacrylate in the United States [11] and Balzarro et al. compared nanosilver gel (AgNPs) in Italy [12]. Total 636 participants were included in the 2 studies. When examining the timeframe required for wound healing, no significant difference between control and intervention groups was reported. Characteristics and outcomes of each study are presented in Table 1.
Table 1. Summary of included studies
Adverse effects
Alemayehu et al. reported that the number of adverse effects using the 2-octyl cyanoacrylate group was greater than that of the antibiotic group (bacitracin), including the incidence of respiratory distress. Meanwhile, Balzarro et al., reported adverse effects in the antibiotic group (gentamicin) in the form of reactions to deep or severe wound infections with or without tissue damage accompanied by hematomas that required aspiration (Southampton Scoring System (SSS) Grade V).
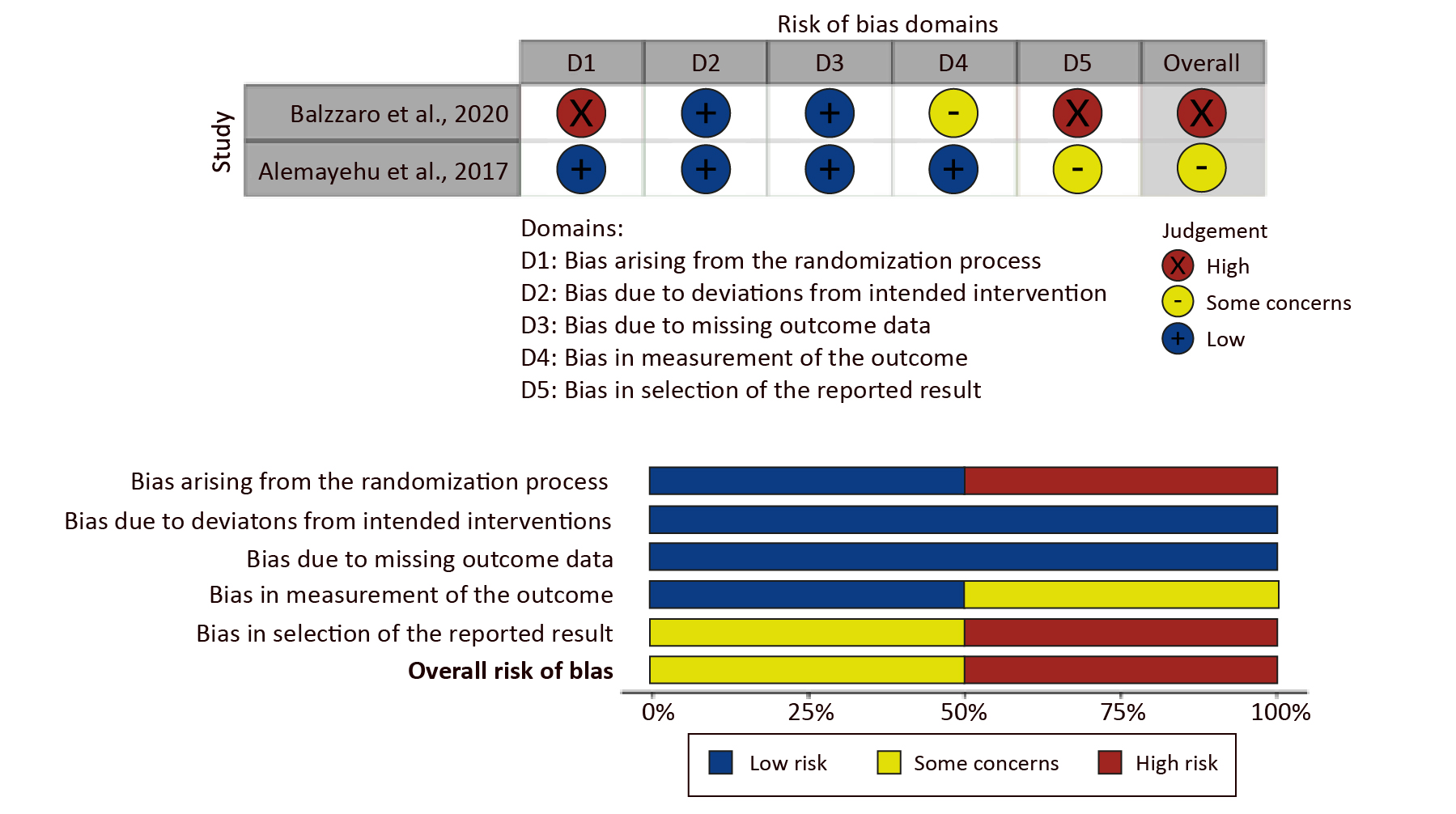
Risk of Bias
The results of the risk of bias assessment based on the RoB-2 tool are shown in Figures 2A and 2B. In study conducted by Balzarro et al., “high” concerns are related to the lack of randomization process and the measurement of outcomes. In the study by Alemayehu et al., “some” concerns are caused by the bias in reported results due to the loss of some of patients are loss to follow-up. The concerns reported in each of these studies are related to the outcomes reported in the existing studies.
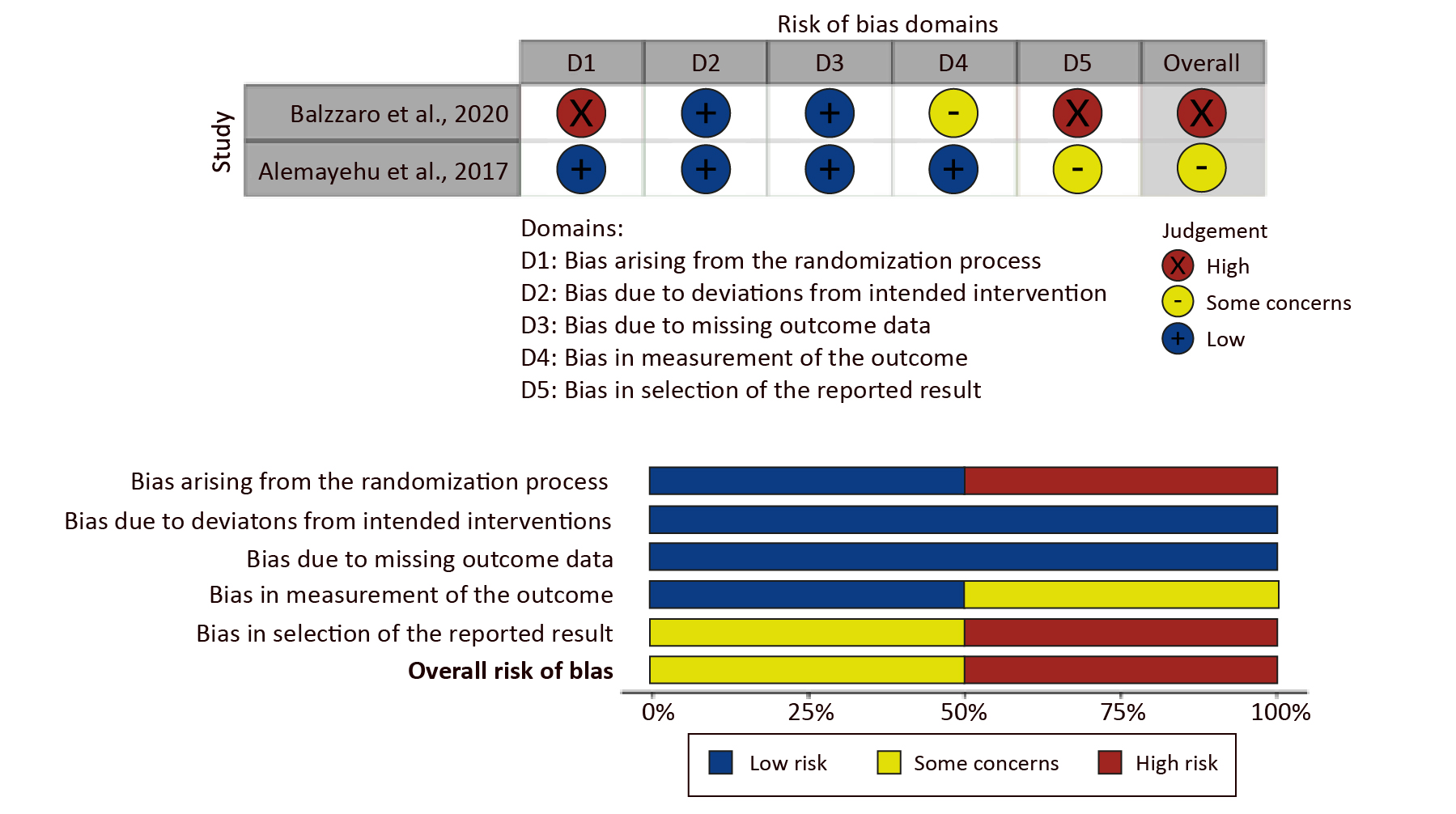
Figure 2. Domain of risk of bias assessment (A) and the overall result of risk of bias (B)
Discussion
Circumcision is generally a sterile surgical procedure, but topical antimicrobial agents may be indicated in some situations [13]. Increasing awareness of antimicrobial resistance resulting from decades of antibiotic overuse has made therapeutic options increasingly limited [14]. However, patients with poor hygiene and vulnerable socioeconomic conditions, antibiotics are still prescribed antibiotics as prophylaxis after surgical procedures with open wounds or with a high risk of exposure to infection [15]. In addition, antibiotics are an easy-touse and affordable prophylactic treatment for infections [16]. Therefore, alternative antimicrobial options need to be developed to reduce antibiotic use and antibiotic resistance.
Alemayehu et al. found that 2-octyl cyanoacrylate glue did not decrease the rate of recurrent penile adhesions after circumcision. This agent is composed of cyanoacetate and formaldehyde which can polymerize from exposed skin tissue and has the ability to bind strongly with water, blood and body tissues [17]. The development of 2-octyl cyanoacrylate makes it more bio-tolerant and induces less inflammation [17]. 2-octyl cyanoacrylate has been widely used in plastic surgery because it produces minimal wounds with a healing rate that is not much different from suturing [18]. This condition may be due to inadequate retraction of the foreskin after the glue sloughed off. However, most patients with adhesions were able to be treated with manual retractions. The use of 2-octyl cyanoacrylate is also reported to have minimal adverse effects compared to circumcision with suturing [19]. Therefore, the use of 2-octyl cyanoacrylate can be a better and safer choice than suturing for wound closure after surgery.
There was no significant difference between the adverse effects of using 2-octyl cyanoacrylate and bacitracin. Bacitracin works by targeting peptidoglycan inhibition and bacterial cell wall formation, thereby preventing bacterial adhesion on the surface [20]. Bacitracin is more effective against gram-positive bacteria, whereas the majority of infections in the pubic area are caused by gram-negative bacteria [21-22]. However, in vitro studies by Lemnaru (Popa) et al. also demonstrated the efficacy of bacitracin against gram-negative bacteria such as Escherichia coli [20]. 2-octyl cyanoacrylate has antimicrobial properties by forming an effective barrier against gram-positive and gram-negative bacteria [23]. Although the Park et al. (2021) study reported the risk of allergic contact dermatitis due to 2-octyl cyanoacrylate, such risk level tends to be low [24]. Due to few adverse effects and outcomes that are not significantly different, 2-octyl cyanoacrylate can be an alternative to antibiotics for circumcision wounds.
A study by Balzarro et al. found that AgNPs gel was effective in healing circumcision wounds, but that healing time was longer compared to gentamicin cream. Adibhesami et al. reported that administering gentamicin combined with AgNPs can accelerate the wound healing rate compared to AgNPs alone in an animal model [25]. Gentamicin is one of the most commonly used antibiotics for post-surgical wounds because it is effective against gram-positive and gram-negative bacteria, particularly in high infection-risk locations e.g. colorectal and perineal [26]. Also, gentamicin interacts with skin keratinocytes by increasing laminin α3 and β3 expression [27]. Although it is known that AgNPs can heal wounds by inhibiting the expression of pro-inflammatory cytokines such as tumor necrosis factor-α (TNF-α), tumor growth factor-β1 (TGFβ1) and IL-6, while the expression of anti-inflammatory cytokines such as IL-10, vascular endothelial growth factor (VEGF) and interferon-λ (IFN-λ) increases, thereby influencing inflammatory cytokines and proliferation of keratinocytes [25].
Existing literature demonstrates that silver nanoparticle (AgNPs) gel is an effective and safe alternative to antibiotic cream for wound healing after circumcision. While AgNPs gel may lead to a longer healing process, it is less likely to cause side effects compared to antibiotics. Components of antibiotics that interact mediated by the immune system can index hypersensitivity reactions that cause various symptoms such as angioedema, urticaria, or in more severe cases such as acute tubular necrosis [28]. Although AgNPs also have a risk of allergies, several approaches include modifying particle size, surface functionalization and preparing AgNPs components that have lower inflammatory effects to reduce the negative impact on cells [29]. In this study, the wound healing rate in the AgNPs group was lower, although Balzarro et al. also reported that the antibiotic group caused adverse effects. The healing rate in each group was also not significantly different. However, this difference in healing ability needs to be investigated further regarding their interaction at the cellular level so that AgNPs can be a safer alternative to antibiotics.
The prevalence of antibiotic use is decreasing along with increasing awareness of antibiotic resistance. Several programs have shown positive outcomes in reducing the over prescription of antibiotics [30]. Inappropriate use of antibiotics is most frequent in cases of upper respiratory tract infections (sore throat and cough), otitis media and sinusitis [31]. The prescription of antibiotics to patients undergoing obstetric and gynecological, gastrointestinal, and orthopedic surgery is reported to be far below the guidelines for antibiotic use [32]. Several studies show that continuation of postoperative antibiotics does not provide more benefits if compliance with antibiotic use was good according to the recommendations [33]. However, the prescription of antibiotics as prophylaxis still occurs, especially in outpatients [34]. Therefore, it is necessary to develop appropriate strategies for the prescribing antibiotics in various clinical situations, including circumcision. In our investigation, we encountered a lack of data regarding antibiotic resistance in postoperative circumcision cases. However, there were instances, such as those involving atopic dermatitis patients treated with bacitracin, where high levels of resistance were observed [35]. Additionally, there were 3 documented occurrences of gentamicin-resistant infections among patients undergoing peritoneal dialysis during each respective study period [36].
Our study has several limitations. The sample size we analyzed is limited due to the design and study centers we included, so studies with similar aims in broader and more diverse populations are needed. Our literature search strategy led us to exclude similar studies published in other languages. In addition, both of the analyzed studies were conducted in developed countries (USA and Italy) where hygiene conditions are different than in low- and middle-income countries. More data are needed before non-antibiotic treatment alternatives can be accepted in clinical settings to reduce the level of antimicrobial resistance. Neither of the studies provided data about bacterial resistance, thus highlighting the potential for future research to explore the implications of non-antibiotic drug utilization on resistance risk among circumcision and other postoperative patients. Furthermore, non-antibiotic ointments are typically more expensive compared to antibiotics, thus prompting questions about their cost-effectiveness.
Conclusions
The use of non-antibiotic drugs as a substitute for antibiotics for post-circumcision wound healing is still limited. Non-antibiotic agents have a more fewer adverse effects with no significant differences in healing rates. The included studies are limited to small sample size and high-income country settings that have good hygiene infrastructure. Larger studies are needed to determine the healing effectiveness and safety of non-antibiotic drugs as an alternative to antibiotic treatment after circumcision.
Acknowledgment
None.
Conflict of interest
None.
Funding
None.
References
| 1. |
Baskin LS. Neonatal circumcision: Risks and benefits [Internet]. UpToDate:Wolters Kluwer. 2015. p. 1–10. Available from: https://www.littlesproutings.com/wp-content/uploads/2015/07/Neonatal-circumcision_-Risks-and-benefits.pdf.
|
| 2. |
Bañuelos Marco B, García Heil JL. Circumcision in childhood and male sexual function: a blessing or a curse? Int J Impot Res [Internet]. 2021;33(2):139–48. Available from: https://www.nature.com/articles/s41443-020-00354-y.
|
| 3. |
Iacob SI, Feinn RS, Sardi L. Systematic review of complications arising from male circumcision. BJUI Compass [Internet]. 2022;3(2):99–123. Available from: https://bjui-journals.onlinelibrary.wiley.com/doi/10.1002/bco2.123.
|
| 4. |
Shabanzadeh DM, Clausen S, Maigaard K, Fode M. Male Circumcision Complications – A Systematic Review, Meta-Analysis and Meta-Regression. Urology [Internet]. 2021;152:25–34. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0090429521001138.
|
| 5. |
Chyi LS, San NS. Review of the prescribing pattern in post circumcision in Hospital Kanowit: retrospective cross sectional study. Sarawak J Pharm [Internet]. 2016;1:63–78. Available from: https://myjms.mohe.gov.my/index.php/spj/article/view/19415.
|
| 6. |
Dave S, Afshar K, Braga LH, Anderson P. Abridged version: CUA guideline on the care of the normal foreskin and neonatal circumcision in Canadian infants. Can Urol Assoc J [Internet]. 2017;12(2):18–28. Available from: https://cuaj.ca/index.php/journal/article/view/5034.
|
| 7. |
Many BT, Benyamen B, Moeckel CM, Sarkar A, Goldstein SD, Grabowski J, et al. To wrap or not to wrap: A retrospective review of circumcision dressing and post-procedural bleeding. J Pediatr Surg [Internet]. 2021;56(4):795–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022346820303195.
|
| 8. |
Kumar M, Sarma DK, Shubham S, Kumawat M, Verma V, Nina PB, et al. Futuristic Non-antibiotic Therapies to Combat Antibiotic Resistance: A Review. Front Microbiol [Internet]. 2021;12. Available from: https://www.frontiersin.org/articles/10.3389/fmicb.2021.609459/full.
|
| 9. |
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ [Internet]. 2021;n71. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.n71.
|
| 10. |
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ [Internet]. 2019;l4898. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.l4898.
|
| 11. |
Alemayehu H, Sharp NE, Gonzalez K, Poola AS, Snyder CL, St. Peter SD. The role of 2-octyl cyanoacrylate in prevention of penile adhesions after circumcision: A prospective, randomized trial. J Pediatr Surg [Internet]. 2017;52(12):1886–90. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022346817305493.
|
| 12. |
Balzarro M, Rubilotta E, Trabacchin N, Soldano A, Cerrato C, Migliorini F, et al. Early and Late Efficacy on Wound Healing of Silver Nanoparticle Gel in Males after Circumcision. J Clin Med [Internet]. 2020;9(6):1822. Available from: https://www.mdpi.com/2077-0383/9/6/1822.
|
| 13. |
Gillespie BM, Walker RM, McInnes E, Moore Z, Eskes AM, O’Connor T, et al. Preoperative and postoperative recommendations to surgical wound care interventions: A systematic meta-review of Cochrane reviews. Int J Nurs Stud [Internet]. 2020;102:103486. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0020748919302937.
|
| 14. |
Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf [Internet]. 2014;5(6):229–41. Available from: http://journals.sagepub.com/doi/10.1177/2042098614554919.
|
| 15. |
Sartelli M, C. Hardcastle T, Catena F, Chichom-Mefire A, Coccolini F, Dhingra S, et al. Antibiotic Use in Low and Middle-Income Countries and the Challenges of Antimicrobial Resistance in Surgery. Antibiotics [Internet]. 2020;9(8):497. Available from: https://www.mdpi.com/2079-6382/9/8/497.
|
| 16. |
Geta K. Factors, impacts and possible solutions of antibiotic resistance. World Sci News [Internet]. 2019;138(2):225–47. Available from: https://www.researchgate.net/profile/Kindu-Geta/publication/378304563_Factors_impacts_and_possible_solutions_of_antibiotic_resistance_Review_article/links/65d335dd476dd15fb3444ee5/Factors-impacts-and-possible-solutions-of-antibiotic-resistance-Review-article.pdf.
|
| 17. |
Bao Z, Gao M, Sun Y, Nian R, Xian M. The recent progress of tissue adhesives in design strategies, adhesive mechanism and applications. Mater Sci Eng C [Internet]. 2020;111:110796. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0928493118313006.
|
| 18. |
Dinakar D, Ellur S, Joseph V. A randomized trial comparing octyl cyanoacrylate tissue adhesive and sutures in the management of facial lacerations. Eur J Plast Surg [Internet]. 2019;42(6):597–602. Available from: http://link.springer.com/10.1007/s00238-019-01532-y.
|
| 19. |
Raut A. Sutureless versus sutured circumcision: A comparative study. Urol Ann [Internet]. 2019;11(1):87. Available from: https://journals.lww.com/10.4103/UA.UA_12_18.
|
| 20. |
Lemnaru (Popa) G-M, Truşcă RD, Ilie C-I, Țiplea RE, Ficai D, Oprea O, et al. Antibacterial Activity of Bacterial Cellulose Loaded with Bacitracin and Amoxicillin: In Vitro Studies. Molecules [Internet]. 2020;25(18):4069. Available from: https://www.mdpi.com/1420-3049/25/18/4069.
|
| 21. |
Hoffmann JP, Friedman JK, Wang Y, McLachlan JB, Sammarco MC, Morici LA, et al. In situ Treatment With Novel Microbiocide Inhibits Methicillin Resistant Staphylococcus aureus in a Murine Wound Infection Model. Front Microbiol [Internet]. 2020;10(January):1–13. Available from: https://www.frontiersin.org/article/10.3389/fmicb.2019.03106/full.
|
| 22. |
Morris BJ, Hankins CA, Banerjee J, Lumbers ER, Mindel A, Klausner JD, et al. Does Male Circumcision Reduce Women’s Risk of Sexually Transmitted Infections, Cervical Cancer, and Associated Conditions? Front Public Heal [Internet]. 2019;7(January):1–21. Available from: https://www.frontiersin.org/article/10.3389/fpubh.2019.00004/full.
|
| 23. |
Rushbrook JL, White G, Kidger L, Marsh P, Taggart TFO. The antibacterial effect of 2-octyl cyanoacrylate (Dermabond®) skin adhesive. J Infect Prev [Internet]. 2014;15(6):236–9. Available from: http://journals.sagepub.com/doi/10.1177/1757177414551562.
|
| 24. |
Park YH, Choi JS, Choi JW, Kim HJ. Incidence and risk factor of allergic contact dermatitis to 2-octyl cyanoacrylate and n-butyl cyanoacrylate topical skin adhesives. Sci Rep [Internet]. 2021;11(1):23762. Available from: https://www.nature.com/articles/s41598-021-03319-3.
|
| 25. |
Majeed HM, Wadee SA, Hasan WA. Effect of Nickle Nanoparticles Solution on Staphylococcus aureus Contaminated Open Wounds Healing in Mice. J Pure Appl Microbiol [Internet]. 2020;14(4):2637–48. Available from: https://microbiologyjournal.org/effect-of-nickle-nanoparticles-solution-on-staphylococcus-aureus-contaminated-open-wounds-healing-in-mice/.
|
| 26. |
Musters GD, Burger JWA, Buskens CJ, Bemelman WA, Tanis PJ. Local Application of Gentamicin in the Prophylaxis of Perineal Wound Infection After Abdominoperineal Resection: A Systematic Review. World J Surg [Internet]. 2015;39(11):2786–94. Available from: https://onlinelibrary.wiley.com/doi/10.1007/s00268-015-3159-5.
|
| 27. |
Kwong A, Cogan J, Hou Y, Antaya R, Hao M, Kim G, et al. Gentamicin Induces Laminin 332 and Improves Wound Healing in Junctional Epidermolysis Bullosa Patients with Nonsense Mutations. Mol Ther [Internet]. 2020;28(5):1327–38. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1525001620301404.
|
| 28. |
Blumenthal KG, Peter JG, Trubiano JA, Phillips EJ. Antibiotic allergy. Lancet [Internet]. 2019;393(10167):183–98. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673618322189.
|
| 29. |
Menichetti A, Mavridi-Printezi A, Mordini D, Montalti M. Effect of Size, Shape and Surface Functionalization on the Antibacterial Activity of Silver Nanoparticles. J Funct Biomater [Internet]. 2023;14(5):244. Available from: https://www.mdpi.com/2079-4983/14/5/244.
|
| 30. |
Köchling A, Löffler C, Reinsch S, Hornung A, Böhmer F, Altiner A, et al. Reduction of antibiotic prescriptions for acute respiratory tract infections in primary care: a systematic review. Implement Sci [Internet]. 2018;13(1):47. Available from: https://implementationscience.biomedcentral.com/articles/10.1186/s13012-018-0732-y.
|
| 31. |
Smieszek T, Pouwels KB, Dolk FCK, Smith DRM, Hopkins S, Sharland M, et al. Potential for reducing inappropriate antibiotic prescribing in English primary care. J Antimicrob Chemother [Internet]. 2018;73(suppl_2):ii36–43. Available from: https://academic.oup.com/jac/article/73/suppl_2/ii36/4841818.
|
| 32. |
Alemkere G. Antibiotic usage in surgical prophylaxis: A prospective observational study in the surgical ward of Nekemte referral hospital. Hawryluk GWJ, editor. PLoS One [Internet]. 2018;13(9):e0203523. Available from: https://dx.plos.org/10.1371/journal.pone.0203523.
|
| 33. |
de Jonge SW, Boldingh QJJ, Solomkin JS, Dellinger EP, Egger M, Salanti G, et al. Effect of postoperative continuation of antibiotic prophylaxis on the incidence of surgical site infection: a systematic review and meta-analysis. Lancet Infect Dis [Internet]. 2020;20(10):1182–92. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1473309920300840.
|
| 34. |
Durkin MJ, Jafarzadeh SR, Hsueh K, Sallah YH, Munshi KD, Henderson RR, et al. Outpatient Antibiotic Prescription Trends in the United States: A National Cohort Study. Infect Control Hosp Epidemiol [Internet]. 2018;39(5):584–9. Available from: https://www.cambridge.org/core/product/identifier/S0899823X18000260/type/journal_article.
|
| 35. |
Bessa GR, Quinto VP, Machado DC, Lipnharski C, Weber MB, Bonamigo RR, et al. Staphylococcus aureus resistance to topical antimicrobials in atopic dermatitis. An Bras Dermatol [Internet]. 2016;91(5):604–10. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962016000500604&lng=en&tlng=en.
|
| 36. |
Chen SS, Sheth H, Piraino B, Bender F. Long-Term Exit-Site Gentamicin Prophylaxis and Gentamicin Resistance in a Peritoneal Dialysis Program. Perit Dial Int J Int Soc Perit Dial [Internet]. 2016;36(4):387–9. Available from: http://journals.sagepub.com/doi/10.3747/pdi.2015.00162.
|