Edmonton Frail Scale – caregiver is a reliable source of information about the functional status of a hospitalized elderly patient
Abstract
Background: The success of geriatric care requires cooperation with the patient’s caregivers. This study aims to compare the perspectives of elderly patients and their caregivers on functional efficiency, as measured by the Edmonton Frail Scale. By examining the discrepancies in these assessments, we hope to better understand perceptions of frailty-related functional limitations and improve the personalized approaches in geriatric care.
Material and methods: This cross-sectional study enrolled a sample of hospitalized patients, based on availability of researchers. Exclusion criteria involved: age < 65, communication barriers, manual disability, exacerbation of a chronic disease or acute condition, no contact to the caregiver, lack of consent. The McNemar-Bowker test and the Wilcoxon signed-rank test were used to compare patients’ and their caregivers’ responses.
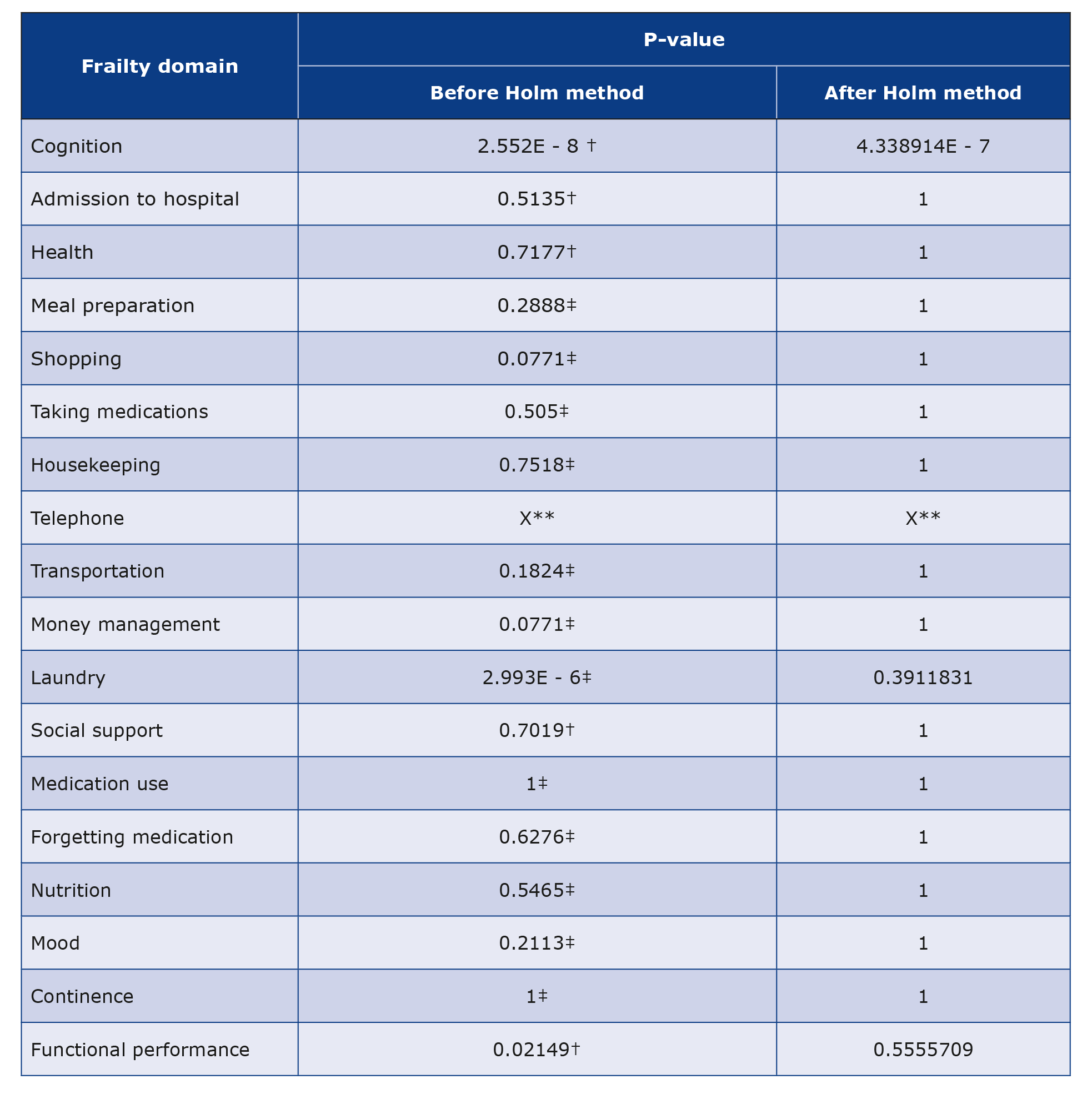
Results: Forty five patients were enrolled. The answers concerning cognitive functions, laundry, and functional performance were statistically different (p < 0.001). Whereas after applying the Holm-Bonferroni method for multiple testing only the judgment of cognitive functions remained statistically different. Other domains showed no statistical differences.
Conclusions: Our results may in general confirm the credibility of caregivers’ perspective in the patients’ functional assessment.
Citation
Stolc B, Kleczewska A, Kulak M, Mierzejewska M, Łyczek W, Zęgota T, Wierzba K. Edmonton Frail Scale – caregiver is a reliable source of information about the functional status of a hospitalized elderly patient. Eur J Transl Clin Med. 2024;7(1):16-21Abbreviations
- EFS – Edmonton Frail Scale
- AMTS – Abbreviated Mental Test Score
- CGA – Comprehensive Geriatric Assessment
Introduction
The dynamic progress of medicine contributes to the extension of the average life expectancy, which results in a constant increase in the population of the elderly. In Poland, this trend is expected to continue until at least the middle of the 21st century [1]. One of the most important problems in the field of geriatrics is frailty. It is described as a decrease in the body’s physiological reserves and is associated with a longer (or inability to) return to balance in the event of a stress factor. It is a multidimensional problem, involving a disorder of the patient’s functioning in the physical, mental and social dimensions [2]. There is evidence that self-reported exponents of this syndrome (e.g. weight loss, slow gait pace, fatigue and lack of physical activity) are predictors of adverse outcomes of greater predictive power and discrimination compared to the assessment of objective exponents [3].
The aims of our study were to investigate differences in the responses of patients and their caregivers to the questions regarding functional status included in the Edmonton Frail Scale (EFS) and to compare their perspective on gait and cognitive status.
Material and methods
The study was conducted at the Department of Rheumatology, Clinical Immunology, Geriatrics and Internal Medicine of the Medical University of Gdańsk, Poland. The research group was recruited from among the patients hospitalized from January to June 2022. Data collection process depended on the organizational accessibility of the researchers.
The exclusion criteria were: aged < 65, cognitive deficits unabling logical communication or other communication barriers (visual or hearing impairment), manual disability, exacerbation of a chronic disease or acute condition at the time of the examination, isolation due to infectious disease, absence or lack of opportunity to contact the caregiver, and lack of consent of the patient or the caregiver/family member to participate in the study. Presence of cognitive deficits were assessed on the basis of the Abbreviated Mental Test Score (AMTS) [4], which was performed by each participant before qualifying for the study. Participants who scored < 7 points on the AMTS were excluded.
The study consisted of two parts. First, we used the EFS to assess the severity of frailty syndrome among patients. The EFS assesses 10 domains of life in a mixed way: subjectively and objectively. The survey questions concern the subjective assessment of general health, functional independence, social support, medication intake, nutrition, mood and urinary continence. In addition, the EFS includes two performance tests assessing cognitive abilities and the risk of fall. The overall score can range from 0 to 17 points. Higher score represents a greater severity of the frailty syndrome [5-6]. The EFS was chosen because of its feasibility of use at the bedside and short examination time compared to a full comprehensive geriatric assessment (CGA). Moreover, EFS was validated to be used by non-specialists without background and experience in geriatric care [5].
In the second part of our study we contacted (by phone or in person) the caregiver or family member, who was previously authorized by the patient, and used the questionnaire part of the EFS in order to evaluate their perspective on the presence of frailty syndrome features in the examined patient.
Furthermore, we asked about the type of relationship with the senior (child, spouse, sibling, other relative, friend or social worker), whether they live together with the patient, their acquaintance with the senior’s everyday life, the frequency of mutual contacts, and the senior’s cognitive and gait abilities from the caregivers’ point of view. For these last two examined items we suggested two original questions, possibly accurate for an average caregiver’s assessment of a patient’s health.
“Do you think your relative needs help while walking?”
Three possible answers were given to the responder, in relation to the values that could be obtained from the functional performance test:
1) “No”, considered as a value of ‘0’;
2) “Yes, they need slight support from time to time”, considered as ‘1’;
3) “Yes, they are unable to walk without assistance of another person or supportive devices such as cane or walking frame”, considered as ‘2’.
“Do you think your relative suffers from dementia?”
Three possible answers were given as well:
1) “No” considered as a value of ‘0’;
2) “Yes, mild stage”, considered as ‘1’;
3) “Yes, advanced stage”, considered as ‘2’.
Results
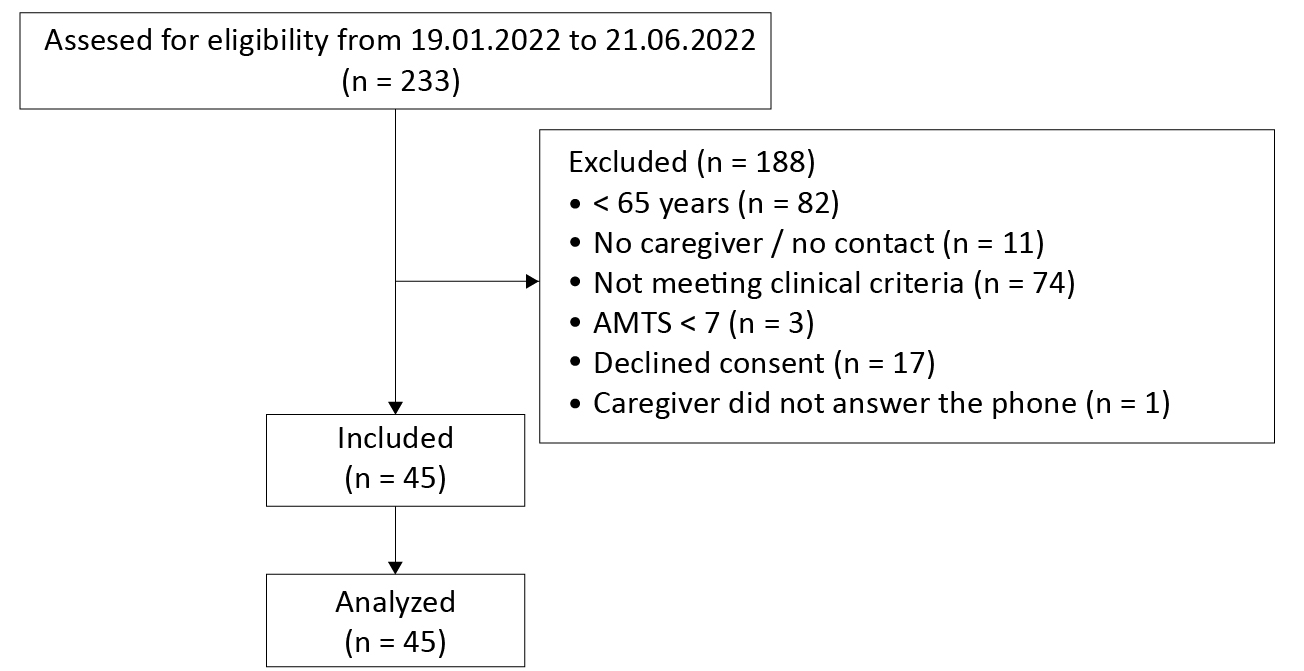
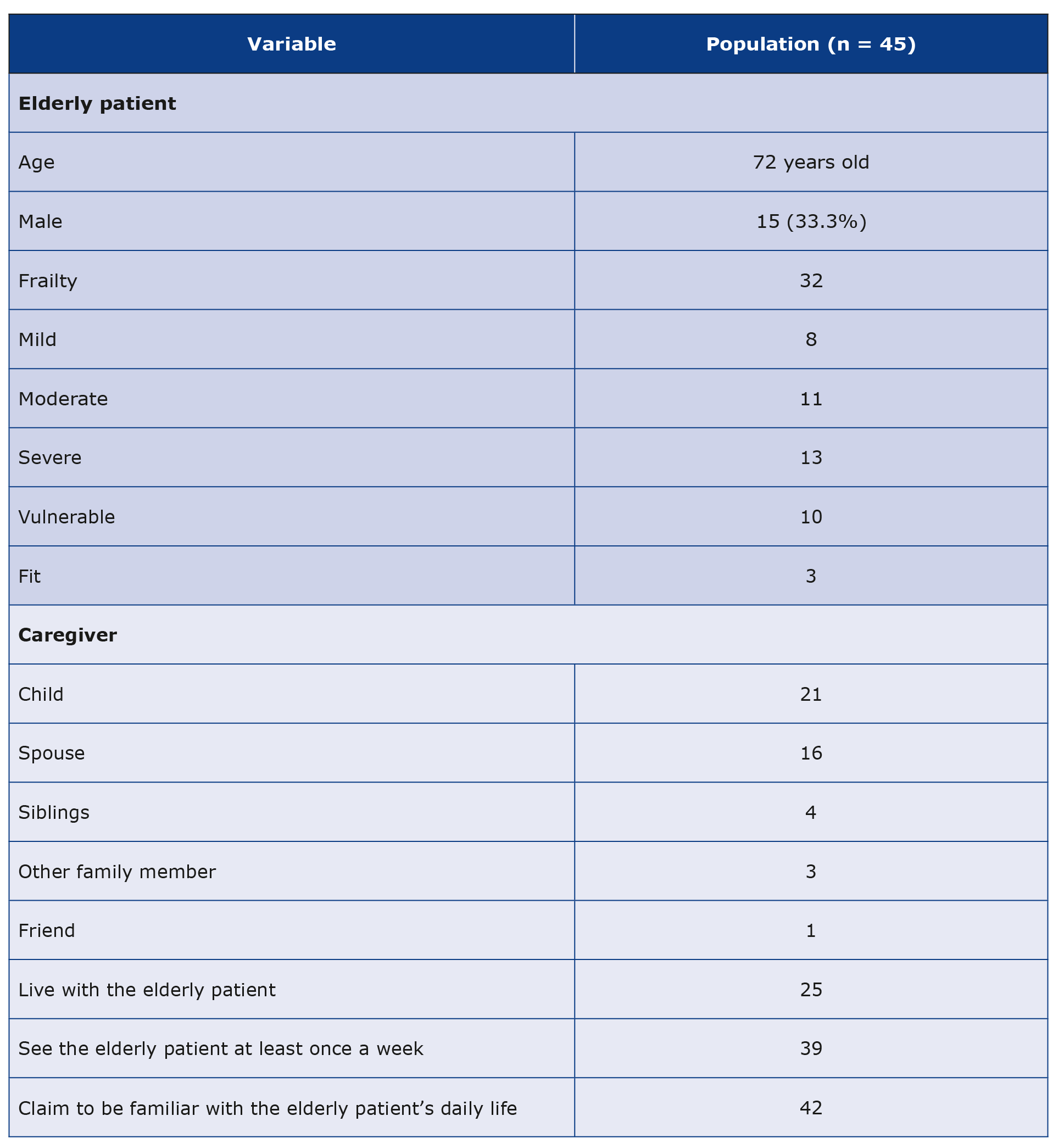
During the 6-month study period 233 patients were screened to participate in the study. The final number of eligible patients was 45 (Figure 1). The characteristics of seniors and their caregivers are presented in Table 1.
Figure 1. Study flow diagram
Table 1. Characteristics of the study group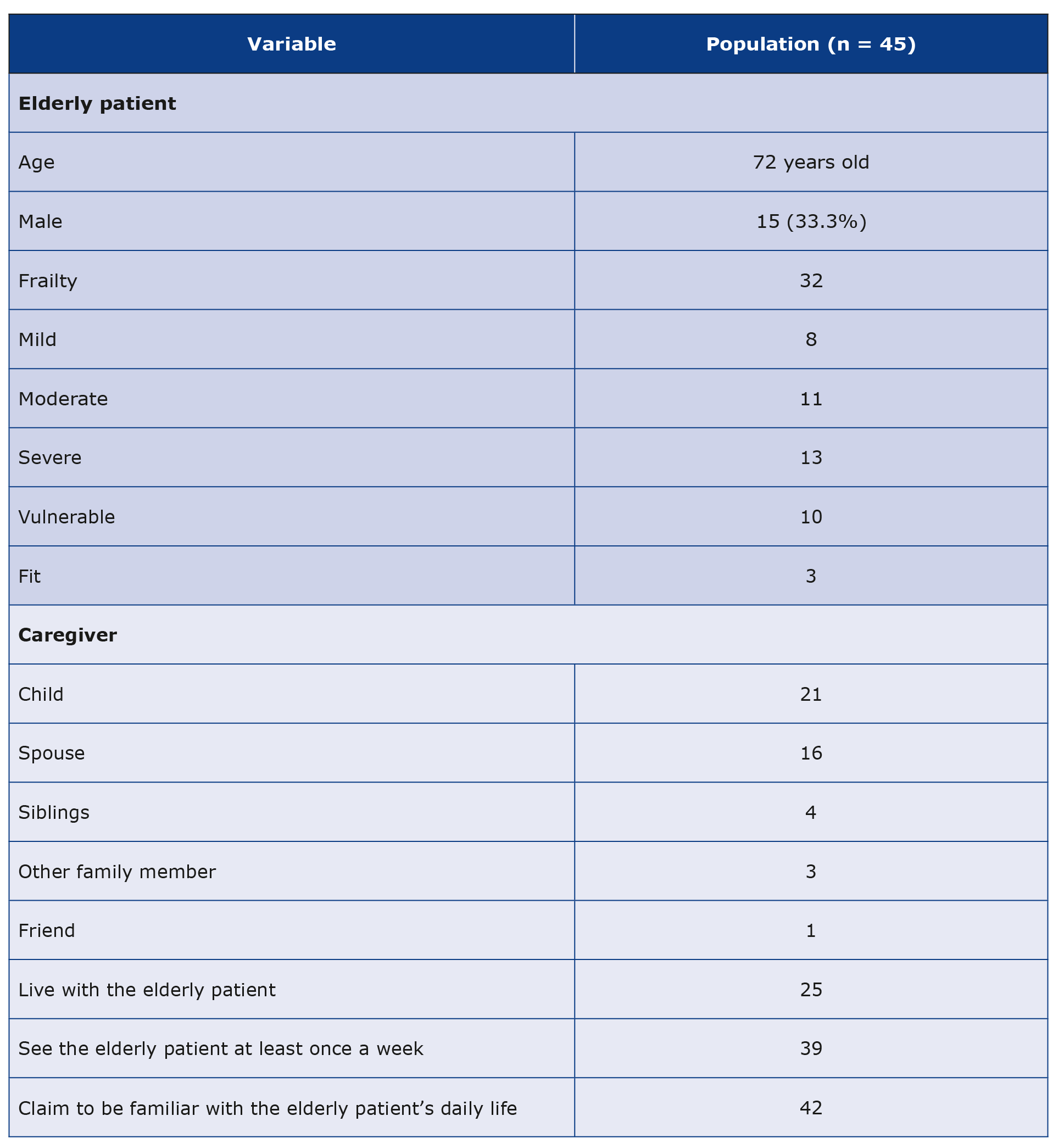
EFS results were normally distributed, 71% (n = 32) of patients met the frailty criteria. The EFS score did not correlate with age. People living with a caregiver showed, on average, a higher severity of frailty syndrome (mean EFS score 8.28 compared to 6.75).
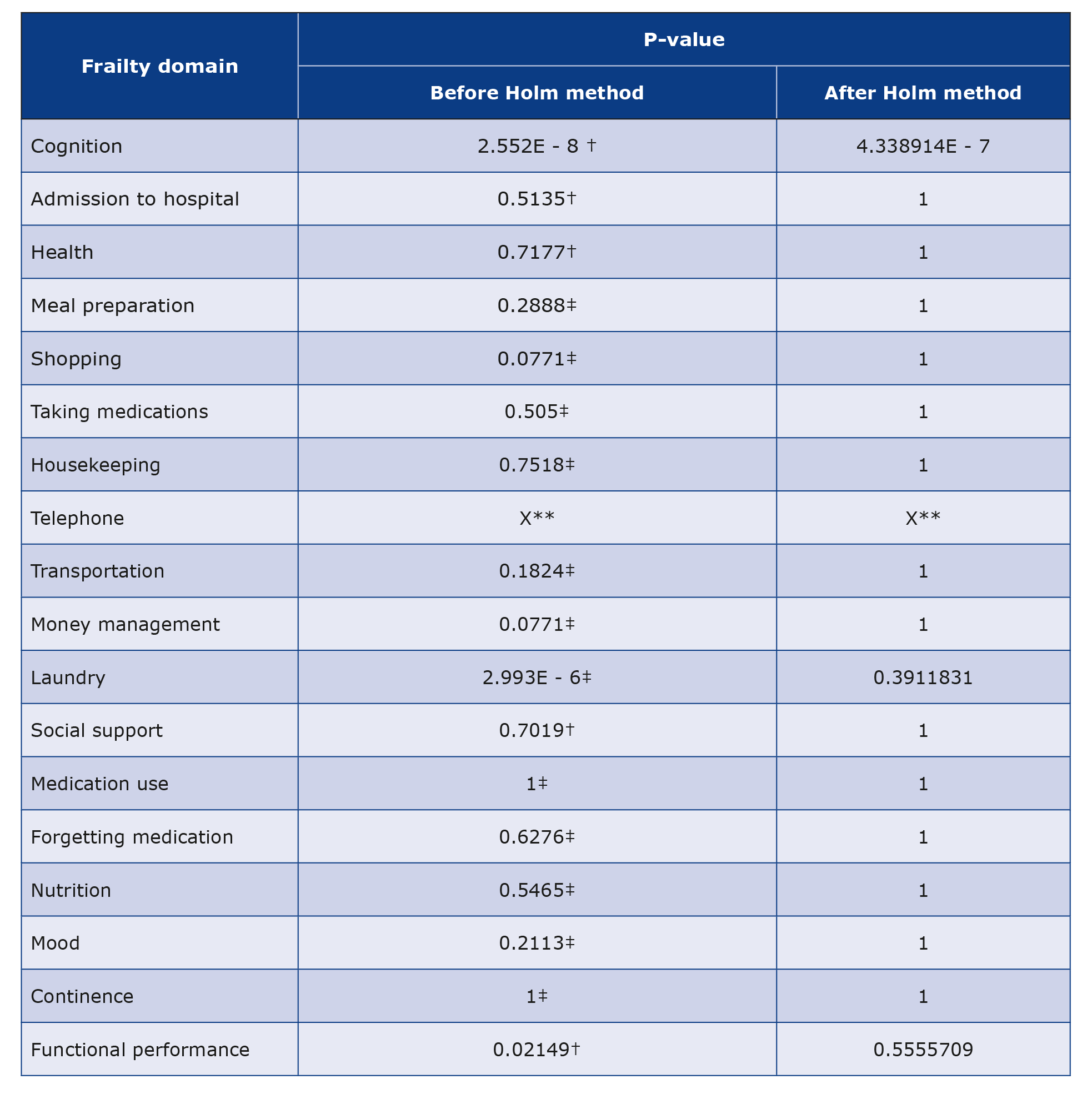
To compare the answers of patients and their caregivers, the Bowker-McNemar test was used for questions in which the answers were on a nominal scale. For variables in which there was an ordinal scale, the Wilcoxon signed-rank test was used. The answers of the senior and his caregiver turned out to be statistically different in the question addressing the ability to do laundry on their own and in two domains outside the questionnaire part – cognitive abilities, and functional performance. However, after applying the Holm method for multiple testing, only the results of the cognitive assessment were statistically different. The answers regarding other domains did not show statistically significant differences. Comparison of the cognitive ability assessment measured by objective test and opinion of a carer turned out to be the least convergent.
Some caregivers declared insufficient knowledge to answer several questions, specifically about taking medications (question 1 n = 4; question 2 (n = 4), preparing meals (n = 1), mood (n = 4), incontinence (n = 2). The results of statistical tests are presented in Table 2.
Table 2. Comparison of patient and caregiver responses
Discussion
Despite the well-established importance of taking a collateral history in geriatrics [7], literature exploring this field is scarce, usually focusing on assessing the presence of cognitive disorders [8]. Nevertheless, even in the presence of dementia symptoms, physicians rarely take collateral history or the obtained history is incomplete [9]. Physicians also report a lack of training and tools facilitating the collection of anamnesis from the patient’s family [10].
Statistical analysis of the obtained data showed that there were no significant differences between the responses of patients and caregivers to questions included in the questionnaire part of EFS. While there was no statistical difference in the results regarding functional performance, there was a difference between the cognitive performance of seniors and the assessment of seniors’ cognitive abilities by their caregivers.
Our study has several limitations. First of them is the small study group (n = 45), limited to a single center. Secondly, many patients who met the clinical and organizational inclusion criteria declined to participate in the study (n = 17). We hypothesize that patients who agreed to participate in the study had better relationships with their caregivers, and therefore the results may be biased.
In the EFS the cognitive domain is assessed using the clock-drawing test. It is worth mentioning that despite its recognized value, the clock-drawing test is a screening test and should not be applied as the sole diagnostic tool for dementia [11]. Moreover, the clock-drawing test allows objective assessment of the patients’ cognition, not subjectively. Hence, the obtained results are difficult to compare to the caregivers’ responses.
We would also like to point out that for organizational reasons our study included a group of patients that did not have severe cognitive impairment, which was excluded using the AMTS. Therefore our results may not be applicable to seniors with advanced cognitive deficits.
Conclusions
The results of our study suggest that the caregiver is a reliable source of information about the patient’s functional status. This is valuable when patients for various reasons (e.g. acute illness or dementia) are unable to answer questions about their previous functioning [9, 12]. Due to the limitations mentioned above, larger studies are needed to confirm our results.
Acknowledgements
The authors used the Edmonton Frail Scale (bedside version), copyright 2000. All rights reserved. Created by Dr. Darryl Rolfson et al. and used under license from the University of Alberta: https://edmontonfrailscale.org.
Funding
None to report.
Conflicts of interest
None to report.
References
| 1. |
Główny Urząd Statystyczny. Sytuacja demograficzna osób starszych i konsekwencje starzenia się ludności Polski w świetle prognozy na lata 2014–2050 [Internet]. GUS, Warszawa. 2014 [cited 2022 Oct 25]. Available from: https://przemocymowimystop.mrips.gov.pl/wp-content/uploads/2021/11/Sytuacja-demograficzna-osob-starszych-i-konsekwencje-starzenia-sie-ludnosci-Polski-w-swietle-prognozy-na-lata-2014-2050..pdf.
|
| 2. |
Sacha M, Sacha J. Frailty syndrome – Uni- and multidimensional approach / Zespół kruchości – podejście jedno- i wielowymiarowe Frailty syndrome – uni- and multidimensional approach [in Polish]. Geriatrics [Internet]. 2017;11:290-3. Available from: https://www.akademiamedycyny.pl/wp-content/uploads/2018/04/Geriatria_4_8.pdf.
|
| 3. |
Papachristou E, Wannamethee SG, Lennon LT, Papacosta O, Whincup PH, Iliffe S, et al. Ability of Self-Reported Frailty Components to Predict Incident Disability, Falls, and All-Cause Mortality: Results From a Population-Based Study of Older British Men. J Am Med Dir Assoc [Internet]. 2017;18(2):152-7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1525861016303723.
|
| 4. |
Skalska A. Kompleksowa ocena geriatryczna [in Polish]. In: Grodzicki T, Kocemba J, Skalska A, editors. Geriatria z elementami gerontologii ogólnej Podręcznik dla lekarzy i studentów. 1st ed. Gdańsk: Via Medica; 2006. p. 68-75.
|
| 5. |
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton Frail Scale. Age Ageing [Internet]. 2006;35(5):526-9. Available from: https://doi.org/10.1093/ageing/afl041.
|
| 6. |
Jankowska-Polańska B, Uchmanowicz B, Kujawska-Danecka H, Nowicka-Sauer K, Chudiak A, Dudek K, et al. Assessment of frailty syndrome using Edmonton frailty scale in Polish elderly sample. Aging Male [Internet]. 2019;22(3):177-86. Available from: https://www.tandfonline.com/doi/full/10.1080/13685538.2018.1450376.
|
| 7. |
Religa D, Derejczyk J. Drogowskazy w geriatrii [in Polish]. 1st ed. Warszawa: PZWL; 2021. 506 p.
|
| 8. |
Briggs R, O’Neill D. The informant history: a neglected aspect of clinical education and practice. QJM An Int J Med [Internet]. 2016;109(5):301-2. Available from: https://doi.org/10.1093/qjmed/hcv145.
|
| 9. |
Fitzpatrick D, Doyle K, Finn G, Gallagher P. The collateral history: an overlooked core clinical skill. Eur Geriatr Med [Internet]. 2020;11(6):1003-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32705626.
|
| 10. |
Dyer AH, Foley T, O’Shea B, Kennelly SP. Cognitive assessment of older adults in general practice: the collateral history. Irish J Med Sci (1971 -) [Internet]. 2018;187(3):683-7. Available from: https://doi.org/10.1007/s11845-017-1723-8.
|
| 11. |
Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry [Internet]. 2000;15(6):548-61. Available from: https://doi.org/10.1002/1099-1166(200006)15:6%3C548::AID-GPS242%3E3.0.CO.
|
| 12. |
Ghosh D, Karunaratne P. The importance of good history taking: a case report. J Med Case Rep [Internet]. 2015;9(1):97. Available from: https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-015-0559-y.
|