Abstract
Diabulimia is the intentional omission or reduction of insulin administration in a patient with insulin-dependent diabetes mellitus (IDDM) and a coexisting eating disorder in the attempt to reduce or avoid weight gain. Although the true incidence of diabulimia is unknown, it is estimated that between 20-30% of girls and up to 40% young women with IDDM have experienced diabulimia since their diagnosis of IDDM was made. Patients with diabulimia frequently present to the emergency department, therefore early recognition of the eating disorder and prompt psychiatric consultation are essential. The aim of this review article is to summarize the existing literature about diabulimia and to raise awareness amongst emergency physicians about how to identify and treat these patients.
Citation
Atriham A R, Kleszczyński J, Sierakowska A, Springer J. Diabulimia – a diagnostic and therapeutic challenge in the Emergency Department. Eur J Transl Clin Med. 2024;7(1):57-62Introduction
Diabulimia is not a new disorder. The coexistence of eating disorders with insulin-dependent diabetes mellitus (IDDM) was first described in the 1980s [1] and the term “diabulimia” first appeared in the literature in 2007 [2]. Nevertheless, the clinicians’ awareness of diabulimia is still lagging in 2024. The current edition of the Statistical Manual of Mental Disorders (DSM V published in 2013) does include the intentional omission or reduction of insulin with the intention to reduce or prevent weight gain, although this is not described as diabulimia [3]. Whereas the International Classification of Diseases 11th edition (ICD-11) released in 2019, does not mention diabulimia or any equivalent [4].
Although the term “bulimia” is part of the name, patients with diabulimia may also meet criteria for anorexia nervosa (AN). Bulimia nervosa (BN) is the psychotic overeating, characterized by lack of control during the eating binge, followed by feelings of guilt, shame and compensation with self-induced vomiting, use of laxatives, diuretics, food deprivation and vigorous exercise [5]. AN overlaps many of the symptoms of BN, with the difference that these patients with AN typically do not binge-eat [6]. In both eating disorders, the psychological long-term effects can lead to low self-esteem, feelings of incompetence, anxiety, depression and even suicidality (defined as the risk of suicide, indicated by suicidal ideation or intent) [7]. The main objective of patients with diabulimia is to avoid the anabolic effects of insulin with regards to weight gain. Their body image is so distorted, they are willing to suffer the consequences and present to the ED with all the clinical features of poorly controlled diabetes plus the complications of the underlying eating disorder. The aim of this article is to review the unique challenges that exist in the identification and treatment of patients with diabulimia at the Emergency Department (ED) and to raise awareness amongst emergency physicians (EPs).
Material and methods
We used PubMed and Google Scholar to search for literature using keywords such as “diabulimia” and “eating disorders in diabetes.” The criteria of inclusion were: article type (clinical trial, randomized control trial or systematic review), language (English or Polish) and description of patient management. This is a narrative review, therefore meta-analysis was not performed.
Results
The initial literature search retrieved 966 records (44 about diabulimia and 922 about eating disorders in diabetes). After applying the exclusion criteria, 866 abstracts were excluded. Full texts of the remaining 144 records were read and 111 of them were excluded due to lack of description of patient management at the ED. Finally, 29 full text articles (including 3 guidelines) were included in the analysis. Full text articles were searched for relevant references regarding the epidemiology and pathophysiology of diabulimia.
Discussion
Currently, there is little data on the etiopathogenesis of diabulimia. However, based on the literature review, two relationships can be distinguished:
– due to the need to strictly follow the diet and numerous dietary restrictions that require the elimination of particular types of food, as well as focusing on the caloric value of food, diabetes may predispose to the development of eating disorders;
– eating disorders and irregular food intake, frequent binge eating resulting in excessive load on the endocrine system may contribute to the development of diabetes [5, 8].
The above hypotheses are reflected in the research. An experiment conducted on a group of adults suffering from insulin-dependent diabetes, with a median age of 51 years, determined the frequency of probable eating disorders among the research group at 21.7% (20.6% in men and 24.2% in women). However, incorrect use of insulin occurred in 39% of respondents [9]. Other studies conducted on a group of adolescents suggest that 23.9% of patients with type I diabetes present symptoms characteristic of diabetes-related eating disorders, while 32.6% of the respondents had symptoms of at least one mental disorder [10].
The true incidence of diabulimia is unknown and currently it is estimated that between 20-30% of girls and up to 40% young women with IDDM have experienced diabulimia since the diagnosis of IDDM was made [11]. Although the most common eating disorders in the population are AN and BN, data from the Polish literature suggest that diabulimia may occur in 20-30% of girls and young women diagnosed with type I diabetes [7], that men are less likely to present symptoms of this disorder and it often coexists with other mental disorders (mainly anxiety and depression). Interestingly, a population study from Germany revealed that although eating disorders among adolescents with IDDM are more common in females than males (31.2% versus 11.7%), there was little difference in their use of insulin restriction (20.5% of the females versus 18.5% of the males with IDDM) [12].
The mortality rate of IDDM for young girls is estimated at 2.2 per 1000-person years, whereas for girls with an eating disorder the mortality rate is 7.3 (the highest of all psychiatric disorders) and when combining both IDDM and eating disorders the mortality is as high as 34.6 per 1000-person years [13]. It should not be surprising that in psychiatry and endocrinology community, diabulimia is considered the most dangerous eating disorder.
The majority of patients with diabulimia are young women with a low body mass index (BMI), often educated, highly functional and very rational in other aspects of their lives, who have been admitted several times to the hospital due to an IDDM-related complication [14]. These patients are wellaware of the consequences of lowering insulin doses, but their fear of gaining weight is so strong and stressful, that it leads them ignore all that rational thinking.
Management in the Emergency Department
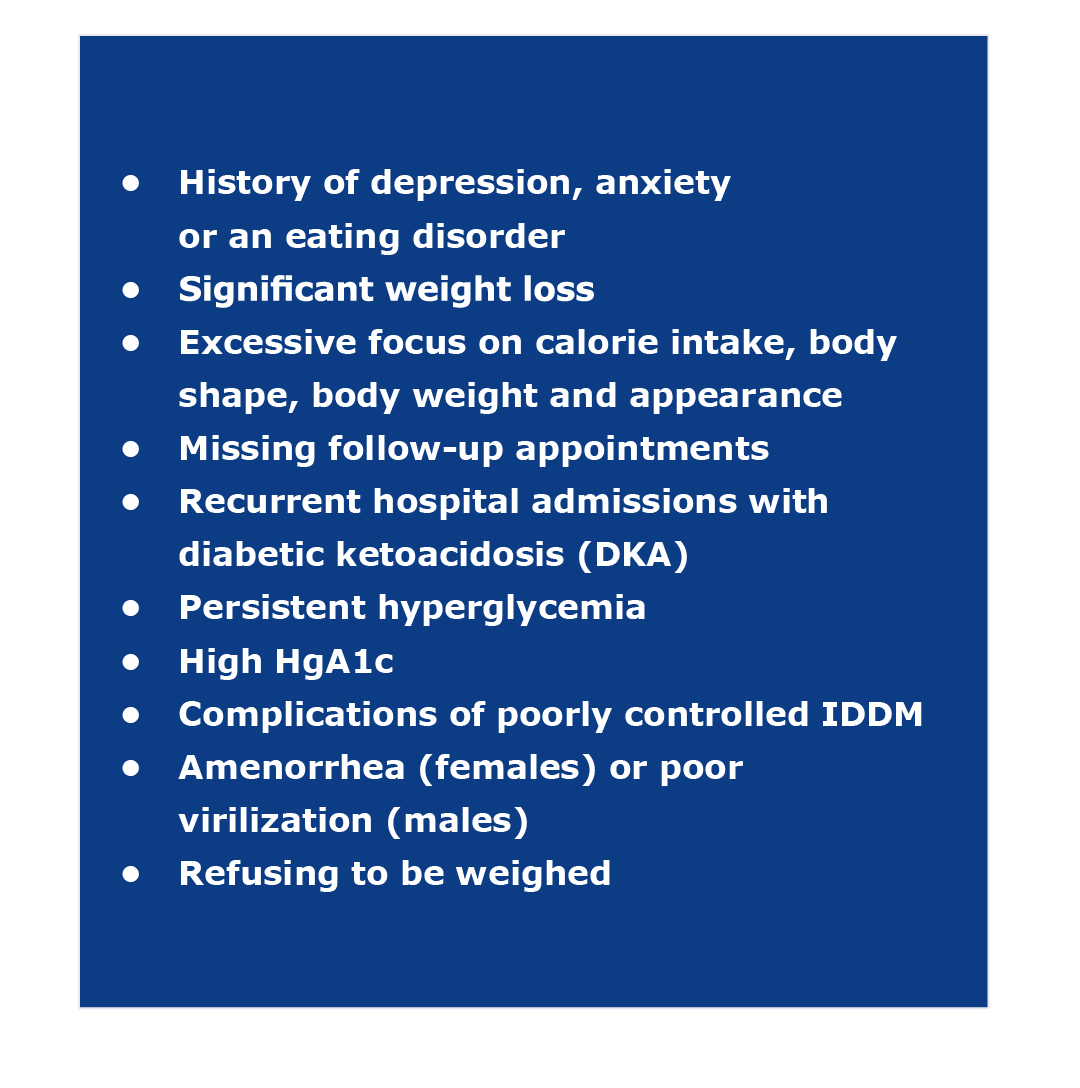
EPs are trained and experienced in the management the metabolic complications of poorly controlled IDDM, e.g. hyperglycemia, DKA, dehydration and electrolyte abnormalities. However, identifying an eating disorder in an ED patient still remains a challenge [15]. The role of the EP is particularly important in the diagnosis of this disorder because the ED is often where these patients have contact with the healthcare system. The frequent episodes of diabetes-associated complaints are an important feature of diabulimia. These presentations should raise the suspicion and prompt the clinician to ask more questions to unveil the possibility of eating disorder. It is worth mentioning that the diagnosis of diabulimia does not need to be made in the ED, however it is the responsibility of EPs to identify the patients with risk factors for an eating disorder and refer them to mental health professionals for evaluation and treatment.
If the EP suspects that a patient with IDDM has an eating disorder, it is important to collect a more detailed history and to dive deeper into the patient’s medical record. Eating disorders are often either well-hidden or denied. In a non-judgmental approach, asking questions to uncover insulin availability, food insecurity and body image dissatisfaction can be extremely helpful. We suggest asking the following 5 questions:
- Do you have access to insulin and the supplies needed to administer your insulin doses?
- Do you have enough food at home for you and your family?
- Have you ever been overweight?
- How often do you reduce or omit your insulin doses?
- Have you ever made yourself vomit or taken laxatives, diuretics or weight loss supplements?
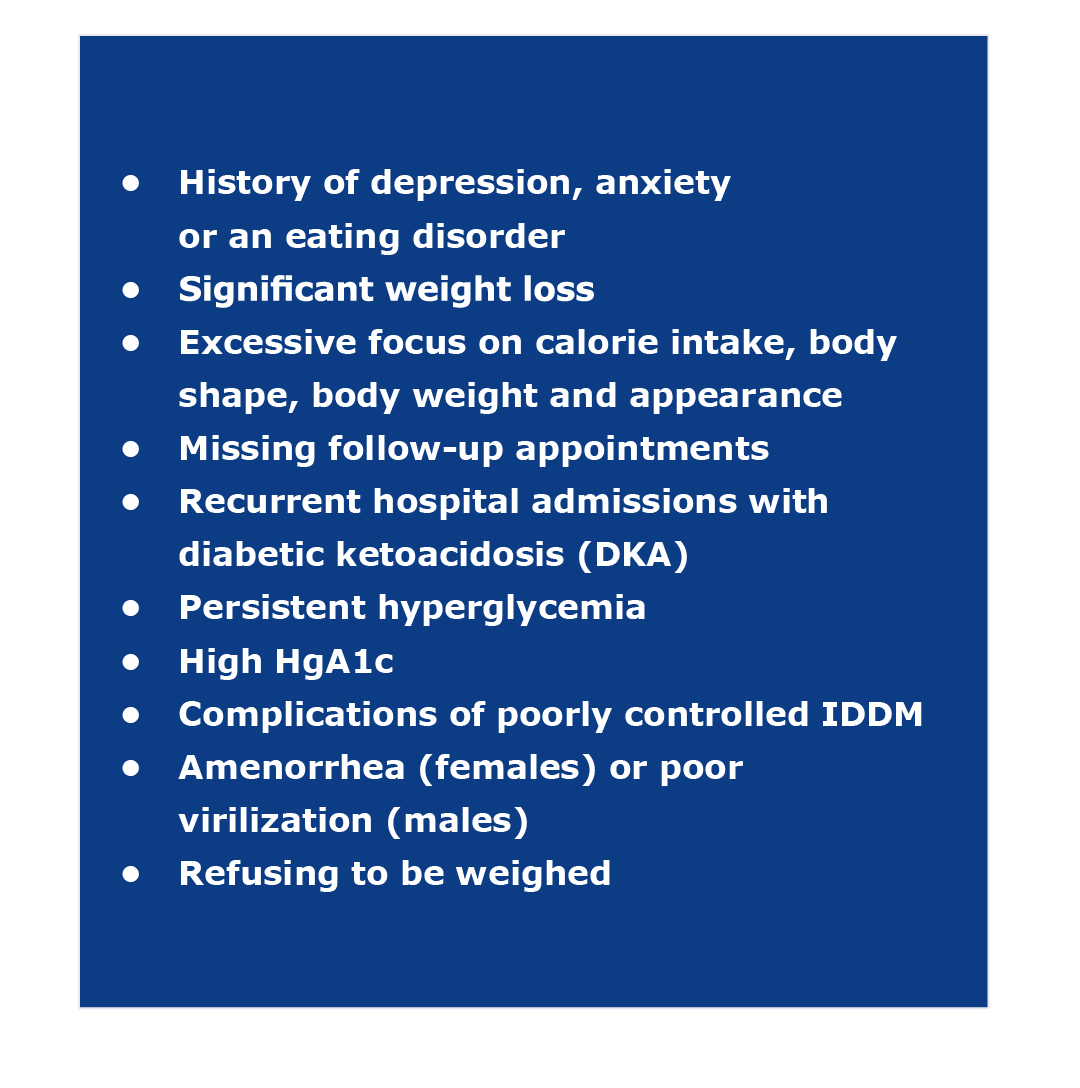
Fig 1. Details in the history and physical exam of a patient with IDDM that should raise the clinician’s suspicion of diabulimia
The first 2 questions are to screen for access to insulin and food insecurity, and the following 3 questions are more specific to having an eating disorder. If the patient has no problems with access to medications and is not food insecure; but screens positive for body image, reducing insulin dosage or using alternative weight loss medications, then it is likely this patient suffers a concomitant eating disorder, and a psychiatric referral is warranted.
This assessment can be done while in the ED (as long as it doesn’t interfere with the ongoing treatment) or at the ward the patient is admitted. A problem may arise if the patient refuses mental health assessment. In such case, it is important to proceed in accordance with the mental health law/s applicable in your country of practice. For example, in Poland psychiatric examination can be conducted without the patient’s consent in accordance with Article 21 of the amended Mental Health Protection Act of August 19, 1994:
“1. A person whose behavior indicates that, due to mental disorders, he or she may directly threaten his or her own life or the life or health of other people, or is unable to meet basic life needs, may also be subjected to a psychiatric examination without his or her consent, and a minor or incapacitated person completely – also without the consent of its legal representative” [16]. Having said that, it is important to acknowledge that different laws may apply in different jurisdictions. In case of doubt, seek advice from the legal department of your hospital or the institution that issued your license to practice medicine.
Special considerations
Patients with diabulimia arrive at the ED with the same complications as any patient with poorly-controlled IDDM: microangiopathy, retinopathy, diabetic nephropathy, peripheral neuropathy, electrolyte abnormalities, diabetic ketoacidosis (DKA) and potentially fatal coma [7]. When adding the eating disorder, the complication rate increases exponentially, adding negative energy balance, low BMI, increased catabolism, hypokalemia, hypomagnesemia, hypophosphatemia, prolonged QT interval, orthostatic disorders, endocrine abnormalities and decreased bone density causing pathological bone fractures [17]. However, the underlying psychiatric disorder (diabulimia) adds unique diagnostic and treatment challenges for clinicians in the ED. These include hypoglycemia, DKA and refeeding syndrome (RS).
Hypoglycemia
Hypoglycemia is the most common life-threatening acute complication of diabetes treatment [18]. Diabulimic patients are at risk for hypoglycemia for several reasons: decreased insulin clearance due to nephropathy (therefore even small doses of insulin can have prolonged effect) and reduced calorie intake which leads to low glycogen storage [19].
Diabetic ketoacidosis
The basic management of DKA in a patient with diabulimia is the same as in any patient with IDDM and has been described in detail in several guidelines [20-22]. However, in addition to the metabolic derangements of DKA, the nutritional deficiencies caused by the restrictive diet some of these patients follow can lead to severe electrolyte deficiencies, e.g. hypocalcemia, hypokalemia, hypomagnesemia and hypophosphatemia [23]. Patients with these abnormalities can present with severe muscle weakness (including the respiratory muscles), tetany, ataxia, paresthesias, nystagmus, diplopia, confusion, seizures, irritability, arrhythmias and even cardiac arrest. Therefore, the initial laboratory analysis should include these electrolytes and the correction of their abnormalities is of paramount importance.
Refeeding syndrome
As implied by its name, RS occurs when the malnourished body receives nutrients again [24]. Besides the serious electrolyte deficiencies (hypokalemia, hypomagnesemia and hypophosphatemia), patients with RS often have sodium and water shifts that can cause fluid overload with pulmonary edema and hypotension [20, 24]. Prolonged hypokalemia can lead to hypokalemic nephropathy and chronic kidney injury [23]. The other important deficiency that becomes evident during RS is thiamine. This B-vitamin is crucial in the glucose metabolism, thus when deficient, patients can develop severe neurological complications. Thiamine supplementation should be routine in these patients with diabulimia prior to alimentation [25]. RS is not a health problem we typically address in the ED. However, the lack of ICU beds is not an uncommon situation in many hospitals, thus we manage patients in the ED longer and longer [26-27]. Having a basic understanding of the possible complications during feeding of patients with diabulimia is important for the EP.
Further management
IDDM complicated with an eating disorder requires amultidisciplinary approach because of the complex social, medical, nutritional and psychological needs of the patients [25]. Cognitive behavioral therapy and SSRIs (mainly fluoxetine) seem to have some effect in reducing complications and promoting weight gain in patients with diabulimia [28-30]. Patient and family education play an important role in reducing maladaptive coping mechanisms and improving the self-image, nutrition and insulin therapy [31]. The use of diabetes-related software (e.g. mobile apps) can also help in patient education and provide ongoing support for decisions regarding insulin therapy and nutrition [32-33].
Conclusions
As the society continues to promote an unrealistic concept of beauty, the prevalence of eating disorders is only expected to rise. Together with an increasing incidence of IDDM, we can expect see more patients with diabulimia presenting to EDs. The role of the EP is therefore not only to diagnose and treat the acute complications of IDDM, but also to recognize those at risk of eating disorder and to ensure timely referrals for comprehensive mental health treatment.
Funding
None to report.
Conflicts of interest
None to report.
References
| 1. |
Hillard JR, Lobo MC, Keeling RP. Bulimia and diabetes: A potentially life-threatening combination. Psychosomatics [Internet]. 1983;24(3):292-5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033318283732329.
|
| 2. |
Yan L. ‘Diabulimia’ a growing problem among diabetic girls. Nephrol News Issues [Internet]. 2007;21(11):36, 38. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17970504.
|
| 3. |
Diagnostic and statistical manual of mental disorders. 5th ed. The American Psychiatric Association. Washington, DC; 2013.
|
| 4. |
ICD-11 Classification of Mental and Behavioral Disorders. Geneva: World Health Organization; 2018.
|
| 5. |
Colton P, Rodin G, Bergenstal R, Parkin C. Eating Disorders and Diabetes: Introduction and Overview. Diabetes Spectr [Internet]. 2009;22(3):138-42. Available from: https://diabetesjournals.org/spectrum/article/22/3/138/2391/Eating-Disorders-and-Diabetes-Introduction-and.
|
| 6. |
Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet [Internet]. 2020;395(10227):899–911. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673620300593.
|
| 7. |
Juruć A, Kubiak M, Wierusz-Wysocka B. Psychological and medical problems in prevention and treatment of eating disorders among people with type 1 diabetes. Clin Diabetol [Internet]. 2016;5(1):26-31. Available from: https://doi.org/10.5603/DK.2016.0005.
|
| 8. |
Colton PA, Olmsted MP, Daneman D, Farquhar JC, Wong H, Muskat S, et al. Eating Disorders in Girls and Women With Type 1 Diabetes: A Longitudinal Study of Prevalence, Onset, Remission, and Recurrence. Diabetes Care [Internet]. 2015;38(7):1212-7. Available from: https://diabetesjournals.org/care/article/38/7/1212/30754/Eating-Disorders-in-Girls-and-Women-With-Type-1.
|
| 9. |
Albaladejo L, Périnet-Marquet P, Buis C, Lablanche S, Iceta S, Arnol N, et al. High prevalence with no gender difference of likely eating disorders in type 1 mellitus diabetes on insulin pump. Diabetes Res Clin Pract [Internet]. 2023;199:110630. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0168822723001055.
|
| 10. |
Tarçın G, Akman H, Güneş Kaya D, Serdengeçti N, İncetahtacı S, Turan H, et al. Diabetes-specific eating disorder and possible associated psychopathologies in adolescents with type 1 diabetes mellitus. Eat Weight Disord - Stud Anorexia, Bulim Obes [Internet]. 2023;28(1):36. Available from: https://link.springer.com/10.1007/s40519-023-01559-y.
|
| 11. |
Pinhas-Hamiel O. Eating disorders in adolescents with type 1 diabetes: Challenges in diagnosis and treatment. World J Diabetes [Internet]. 2015;6(3):517. Available from: http://www.wjgnet.com/1948-9358/full/v6/i3/517.htm.
|
| 12. |
Baechle C, Castillo K, Straßburger K, Stahl‐Pehe A, Meissner T, Holl RW, et al. Is disordered eating behavior more prevalent in adolescents with early‐onset type 1 diabetes than in their representative peers? Int J Eat Disord [Internet]. 2014;47(4):342-52. Available from: https://onlinelibrary.wiley.com/doi/10.1002/eat.22238.
|
| 13. |
Nielsen S, Emborg C, Mølbak A-G. Mortality in Concurrent Type 1 Diabetes and Anorexia Nervosa. Diabetes Care [Internet]. 2002;25(2):309-12. Available from: https://diabetesjournals.org/care/article/25/2/309/23330/Mortality-in-Concurrent-Type-1-Diabetes-and.
|
| 14. |
Kinik MF, Volkan Gonullu F, Vatansever Z, Karakaya I. Diabulimia, a Type I diabetes mellitus-specific eating disorder. Türk Pediatr Arşivi [Internet]. 2017;52(1):46-9. Available from: https://turkarchpediatr.org/en/diabulimia-a-type-i-diabetes-mellitus-specific-eating-disorder-13234.
|
| 15. |
Ma C, Gonzales-Pacheco D, Cerami J, Coakley KE. Emergency medicine physicians’ knowledge and perceptions of training, education, and resources in eating disorders. J Eat Disord [Internet]. 2021;9(1):4. Available from: https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-020-00355-8.
|
| 16. |
Obwieszczenie Marszałka Sejmu Rzeczypospolitej Polskiej z dnia 26 marca 2020 r. w sprawie ogłoszenia jednolitego tekstu ustawy o ochronie zdrowia psychicznego [in Polish]. Dz Ustaw RP [Internet]. 2020; poz. 685. Available from: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20200000685/O/D20200685.pdf.
|
| 17. |
Chidiac CW. An update on the medical consequences of anorexia nervosa. Curr Opin Pediatr [Internet]. 2019;31(4):448-53. Available from: https://journals.lww.com/00008480-201908000-00005.
|
| 18. |
Cryer PE. Hypoglycemia in diabetes: pathophysiological mechanisms and diurnal variation. Prog Brain Res [Internet]. 2006;153:361-5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0079612306530213.
|
| 19. |
Williams ME, Garg R. Glycemic Management in ESRD and Earlier Stages of CKD. Am J Kidney Dis [Internet]. 2014;63(2):S22-38. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0272638613014327.
|
| 20. |
Araszkiewicz A, Bandurska-Stankiewicz E, Borys S, Budzyński A, Cyganek K, Cypryk K, et al. 2023 Guidelines on the management of patients with diabetes-a position of Diabetes Poland. Curr Top Diabetes [Internet]. 2023;3(1). Available from: https://ruj.uj.edu.pl/xmlui/handle/item/311730.
|
| 21. |
Goguen J, Gilbert J. Hyperglycemic Emergencies in Adults. Can J Diabetes [Internet]. 2018;42:S109-14. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1499267117308237.
|
| 22. |
Poole R. Diagnosis and management of type 1 diabetes in adults [Internet]. Vol. 266, National Institute for Health and Care Excellence. p. 23-6. Available from: https://www.nice.org.uk/guidance/ng17.
|
| 23. |
Puckett L. Renal and electrolyte complications in eating disorders: a comprehensive review. J Eat Disord [Internet]. 2023;11(1):26. Available from: http://www.ncbi.nlm.nih.gov/pubmed/36803805.
|
| 24. |
Skowrońska A, Sójta K, Strzelecki D. Refeeding syndrome as treatment complication of anorexia nervosa. Psychiatr Pol [Internet]. 2019;53(5):1113-23. Available from: https://www.psychiatriapolska.pl/Refeeding-syndrome-as-treatment-complication-of-anorexia-nervosa,90275,0,2.html.
|
| 25. |
Chakraborty K, Basu D. Management of anorexia and bulimia nervosa: An evidence-based review. Indian J Psychiatry [Internet]. 2010;52(2):174. Available from: https://journals.lww.com/10.4103/0019-5545.64596.
|
| 26. |
Kappy B, Berkowitz D, Isbey S, Breslin K, McKinley K. Characteristics and patient impact of boarding in the pediatric emergency department, 2018–2022. Am J Emerg Med [Internet]. 2024;77:139-46. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0735675723007015.
|
| 27. |
Mohr NM, Wessman BT, Bassin B, Elie-Turenne M-C, Ellender T, Emlet LL, et al. Boarding of Critically Ill Patients in the Emergency Department. Crit Care Med [Internet]. 2020;48(8):1180-7. Available from: https://journals.lww.com/10.1097/CCM.0000000000004385.
|
| 28. |
Candler T, Murphy R, Pigott A, Gregory JW. Fifteen-minute consultation: Diabulimia and disordered eating in childhood diabetes. Arch Dis Child – Educ Pract Ed [Internet]. 2018;103(3):118-23. Available from: https://ep.bmj.com/lookup/doi/10.1136/archdischild-2017-312689.
|
| 29. |
Crow SJ. Pharmacologic Treatment of Eating Disorders. Psychiatr Clin North Am [Internet]. 2019;42(2):253-62. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0193953X19300127.
|
| 30. |
Hay PP, Claudino AM, Kaio MH. Antidepressants versus psychological treatments and their combination for bulimia nervosa. Cochrane Database Syst Rev [Internet]. 2001; Available from: https://doi.wiley.com/10.1002/14651858.CD003385.
|
| 31. |
Larrañaga A, Docet MF, García-Mayor R V. Disordered eating behaviors in type 1 diabetic patients. World J Diabetes [Internet]. 2011;2(11):189. Available from: http://www.wjgnet.com/1948-9358/full/v2/i11/189.htm.
|
| 32. |
Pi L, Shi X, Wang Z, Zhou Z. Effect of smartphone apps on glycemic control in young patients with type 1 diabetes: A meta-analysis. Front Public Heal [Internet]. 2023;11. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1074946/full.
|
| 33. |
Sun C, Malcolm JC, Wong B, Shorr R, Doyle M-A. Improving Glycemic Control in Adults and Children With Type 1 Diabetes With the Use of Smartphone-Based Mobile Applications: A Systematic Review. Can J Diabetes [Internet]. 2019;43(1):51-58.e3. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1499267117310547.
|