Abstract
Introduction: Cases of myocarditis in people were vaccinated against COVID-19 have been reported in the recent years. Nevertheless, the histopathological features and the pathomechanisms in these cases are still unclear. Hence, a scoping review of existing literature was performed to discover the histopathological features of myocarditis induced by the above-mentioned vaccine.
Methods: A search was performed in the PubMed, Scopus and EMBASE databases to retrieve the relevant records, involving analyses of biopsy and autopsy specimens. Baseline characteristics of the patients and the histopathological characteristics of the respective specimens were extracted and recorded.
Results: Overall, 24 case reports and case series (involving a total of 54 patients) were included in this scoping review. The following signs of inflammation were present in the specimens: lymphocyte infiltration (64.8%), eosinophilic infiltration (29.6%), neutrophil infiltration (3.7%) and giant-cell formation (1.9%). Other features included myocardial tissue necrosis (20.4%), the presence of the SARS-CoV-2 spike protein (16.7%) and microthrombosis (3.7%).
Conclusions: The histopathological characteristics of SARS-CoV-2 vaccine-induced myocarditis were heterogenous, the only common characteristic was the presence of lymphocyte infiltration in more than half of the cases. Studies of unreported past cases may provide further insights into the topic.
Citation
Kalali D, Anestakis D. Histopathological characteristics of myocarditis following COVID-19 vaccination: a scoping review. Eur J Transl Clin Med. 2023;6(2):85-90Introduction
Myocarditis is a rare but serious condition where the heart muscle (myocardium) becomes inflamed [1]. According to the histopathological standard for diagnosing myocarditis (the Dallas criteria), myocarditis is defined as an inflammatory infiltration of the myocardium with or without fibrosis of the tissue [2]. Although the latter disease is not generally life-threatening and doesn’t cause permanent damage to the myocardium, it can lead to hospitalization and increased risk of developing arrythmias [3].
Since early 2021, several cases of myocarditis have been reported in people following vaccination against the severe acute respiratory syndrome coronavirus-2 (SARSCoV-2) virus, particularly in those vaccinated with mRNA vaccines [4-5]. Interestingly, most patients who developed myocarditis presented some common patterns, including the onset of the disease in an average of 2-3 days after receiving the second dose of the SARS-CoV-2 vaccine [6]. Nonetheless, most cases of post-vaccination myocarditis were diagnosed based on medical imaging techniques or laboratory examinations, therefore not enough data and systemic descriptions were available to comprehend the pathophysiology of this condition [7-8]. Hence, there is a significant need for the analysis of biopsy or necropsy specimens of the myocardia of patients with inflammatory cardiomyopathy after receiving the SARS-CoV-2 vaccine. Moreover, according to the proposals of the World Health Organization, it is necessary to systematically evaluate the adverse effects of vaccines [9]. The aim of this study was to conduct a scoping review of the available literature in order to investigate the histopathological features of the myocarditis following SARS-CoV-2 vaccination.
The inclusion criteria were: case report, case series or observational study reporting the biopsy or necropsy results of patients with myocarditis occurring after the SARSCoV-2 vaccination. We used the citation manager EndNote (Clarivate, Philadelphia USA and London UK) to remove duplicate records. All remaining records were screened for eligibility based on their titles and abstracts. Finally, we obtained the full-text versions of the remaining records and assessed them in detail.
Data extraction and statistical analyses
Data was extracted from all included studies regarding the number of patients, their gender, the number of vaccine doses they received prior to the onset of myocarditis, the type of vaccine they received, their medical history, the type of specimen taken (biopsy sample or necrotomy specimen) and the histopathological features found within the myocardial specimens. The extracted data was processed and presented using descriptive statistics. All statistical processes were performed using the STATA software package version 17.0 (StataCorp LLC, College Station USA).
Results
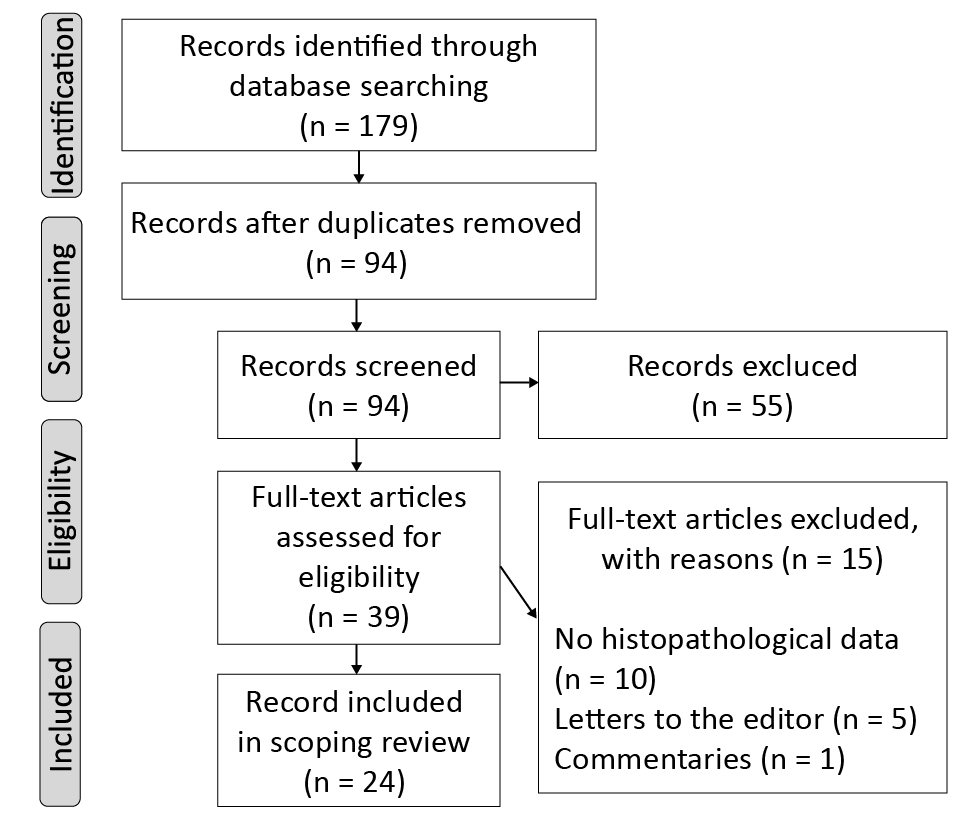
The database search retrieved a total of 179 records, of which 94 remained after the duplicates were removed. During the title and abstract screening, a total of 55 citations were deemed ineligible due to irrelevance to the research question. Once the full-text versions of the remaining articles were assessed, 15 were excluded (see Figure 1 for details). Hence, a total of 24 studies were finally included in the review, all of which were case reports and case series [11-34].
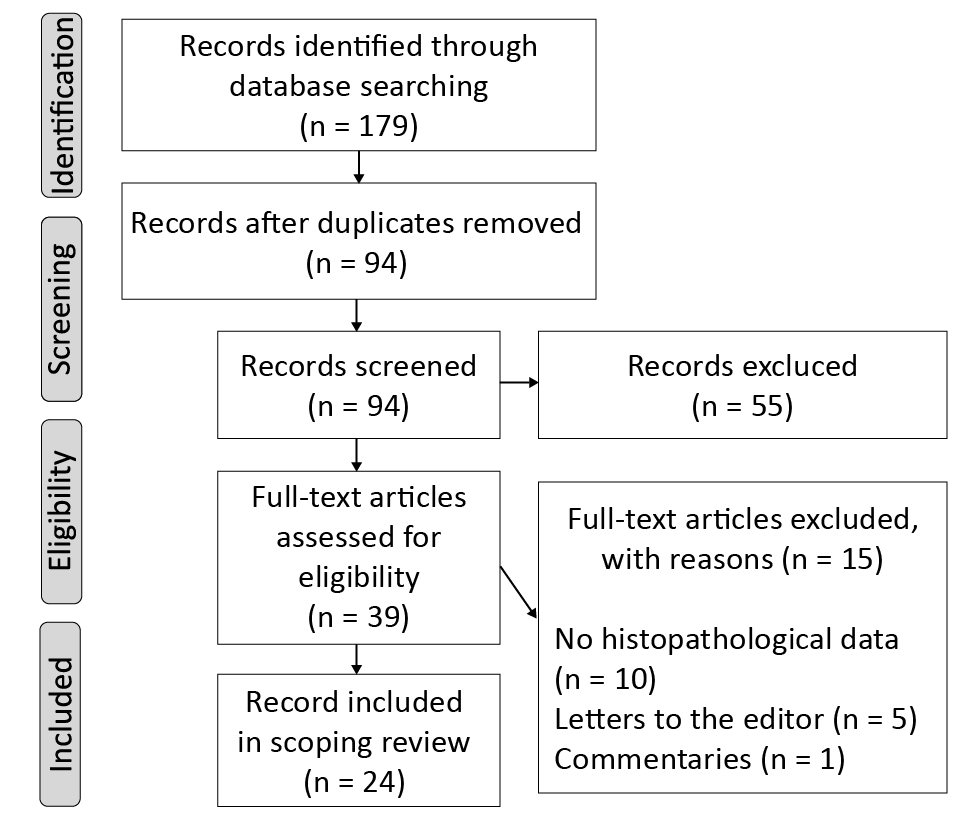
Figure 1. PRISMA diagram of our systematic review
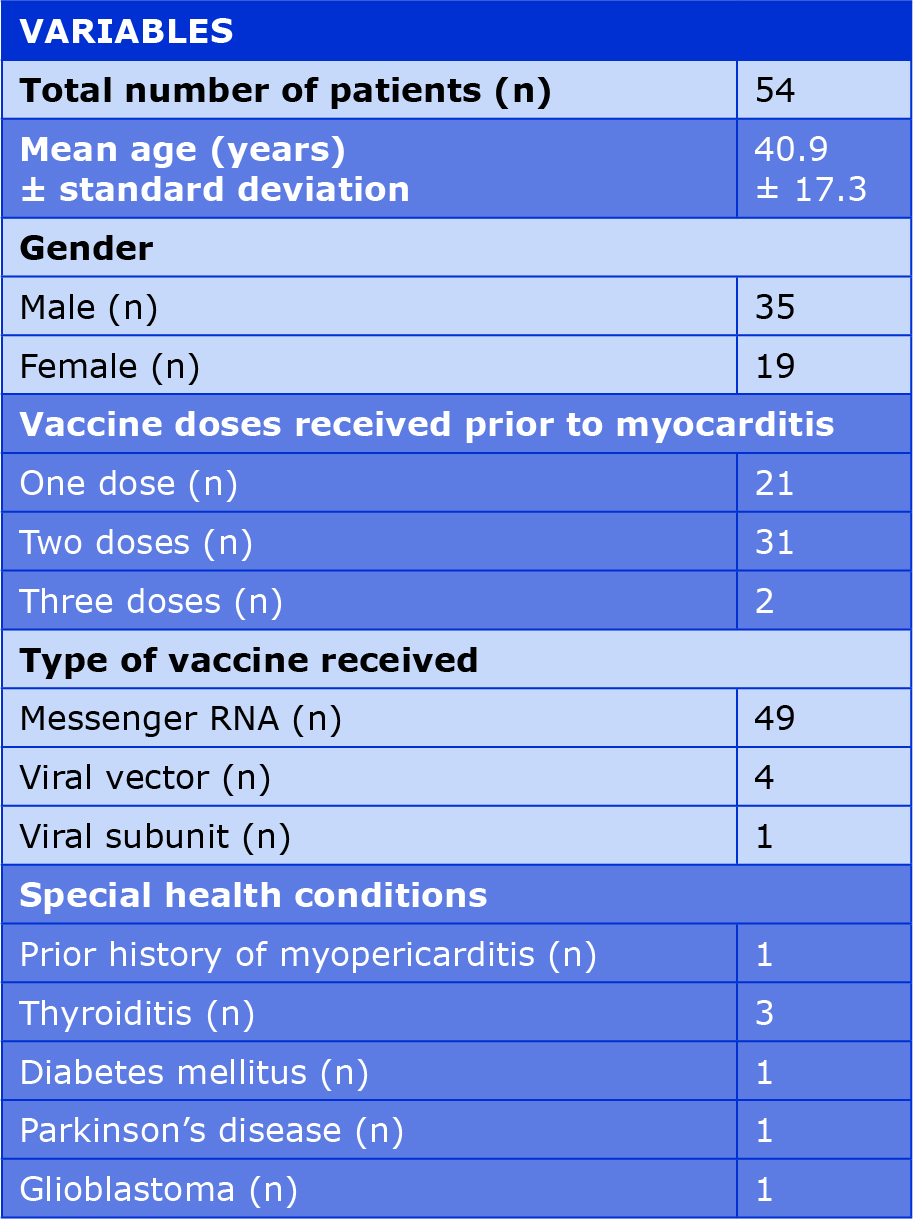
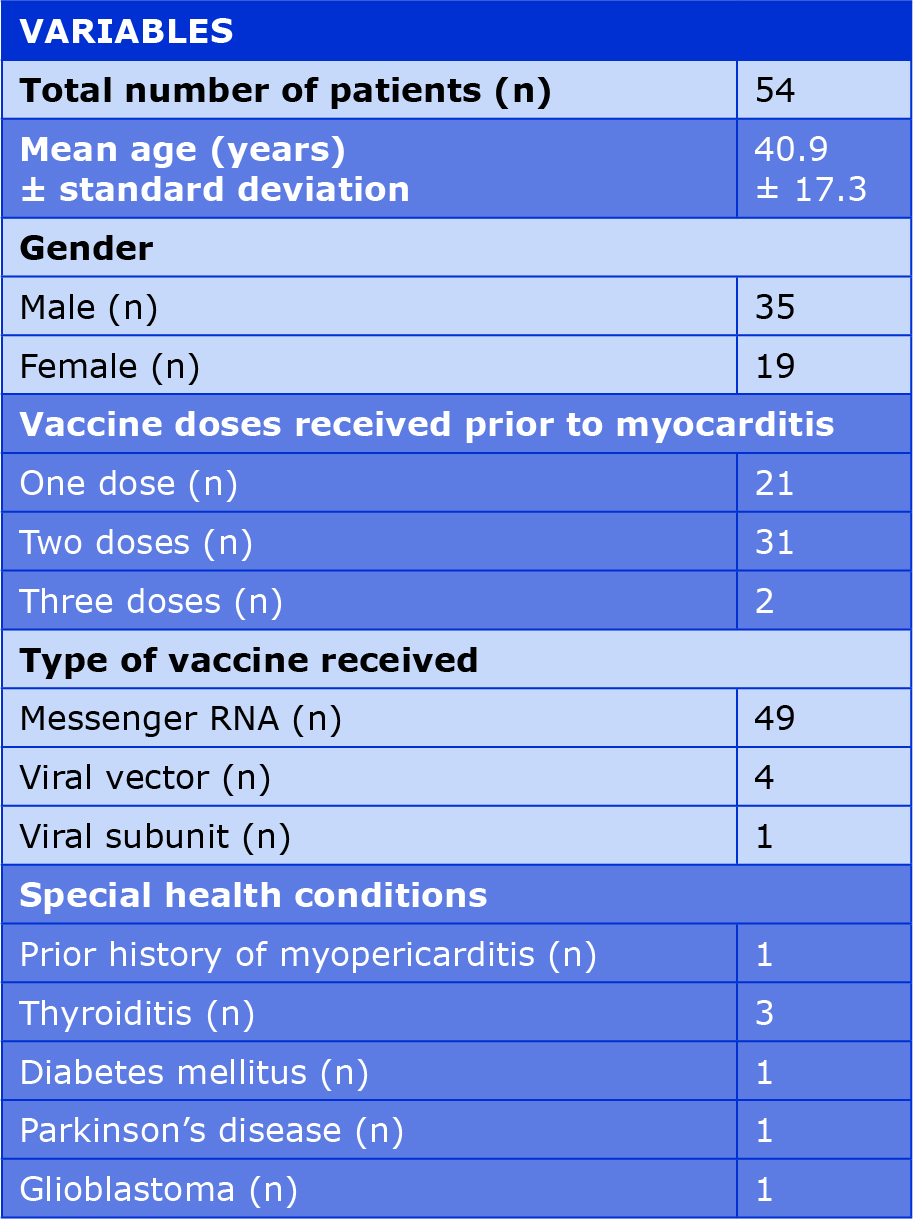
Overall, the included studies described a total of 54 patients who presented with myocarditis after obtaining a dose of the SARS-CoV-2 vaccine. The baseline characteristics and vaccination information of the patients have been recorded in Table 1. Most of the included patients were healthy with no prior history of serious disease and 7 had prior history of myopericarditis, thyroiditis, diabetes mellitus, Parkinson’s disease and glioblastoma [22, 24, 26-28, 31-32]. Moreover, all patients expect 2, developed myocarditis after receiving ether the first or the second dose of the vaccine [23-24]. It is also worth mentioning that majority of the patients who developed myocarditis received an mRNA vaccine.
Table 1. Baseline characteristics of patients in the included studies
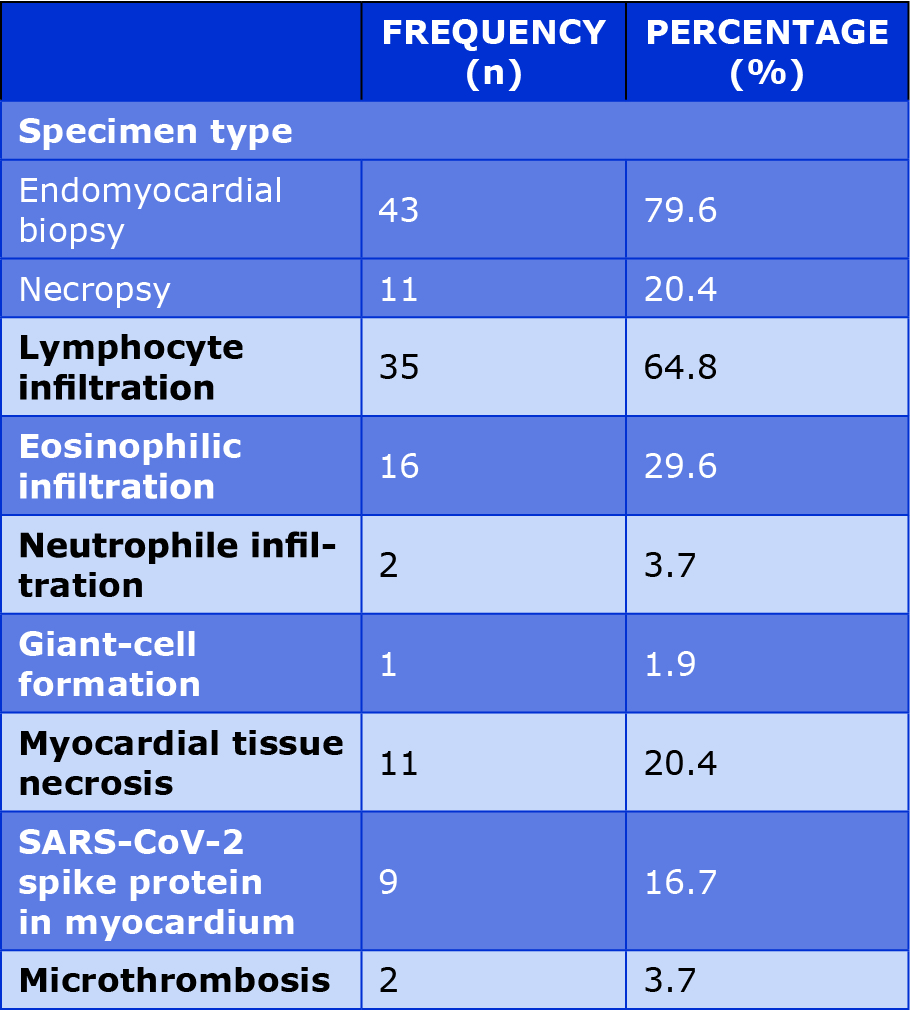
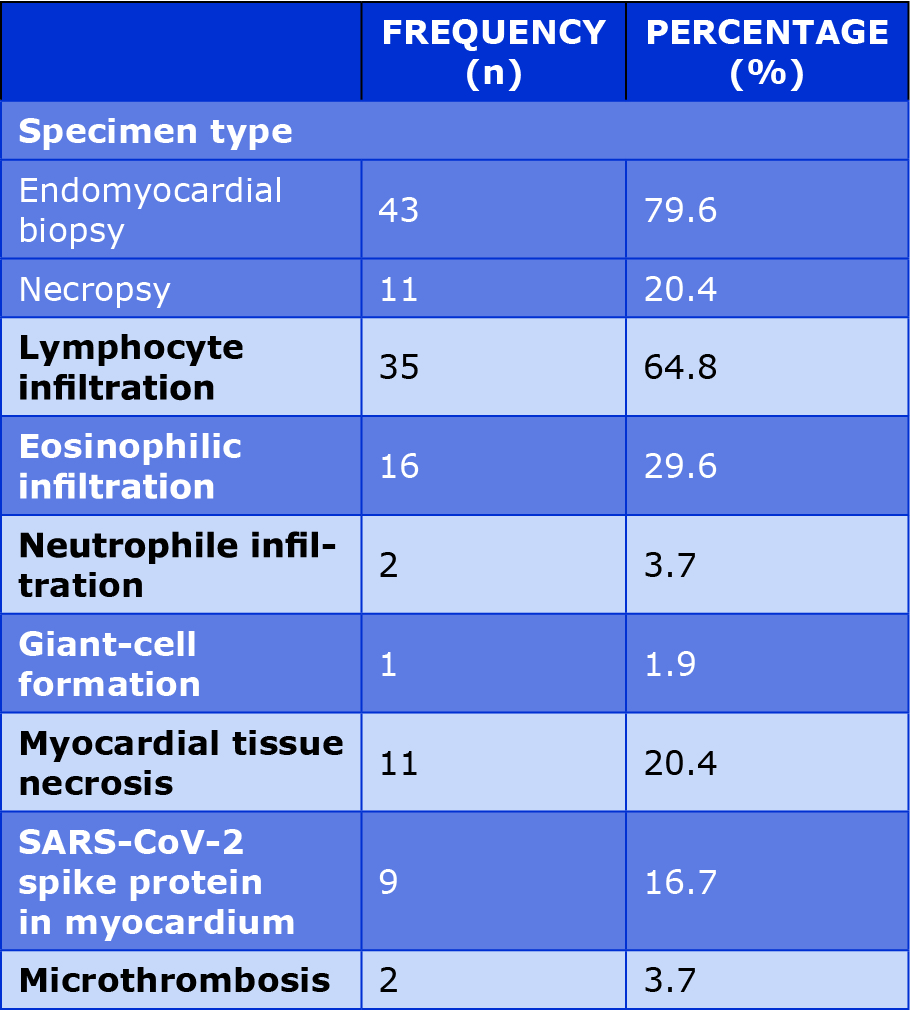
All of the specimens (43 from endomyocardial biopsy and 11 from necropsy) in the included studies had undergone anatomopathological analysis. In all the specimens, myocarditis was characterized by inflammatory infiltration, namely lymphocyte infiltration (64.8%), eosinophilic infiltration (29.6%), neutrophile infiltration (3.7%) and giant-cell formation (1.9%). In some specimens, myocardial tissue necrosis was also observed, which was previously reported, particularly in patients with viral myocarditis [35]. Histochemical analyses also revealed that in 16.7% of the specimens, the SARS-CoV-2 spike protein was present. It is also necessary to mention that in 2 specimens, microthrombi were also present and it is known that microthrombosis is associated with SARS-CoV-2 [12, 25, 36]. Table 2 summarizes the histopathological features of the myocardial specimens in the included studies.
Table 2. Histopathological features of myocardial specimens in the included studies
Discussion
As seen in this scoping review, the histopathological features of the inflamed myocardia after COVID-19 vaccination vary from case to case. The only prevalent feature amongst the cases was the lymphocytic nature of the myocardial inflammation. Interestingly, the most common type of viral myocarditis is lymphocytic myocarditis as well [37]. Therefore, this histopathological finding may possibly indicate the involvement of the virus in the formation of post-vaccine myocarditis. Indeed, one of the proposed mechanisms is the leakage of vaccine nanoparticles into the bloodstream, which subsequently reach the myocardial cells and cause viral protein expression [38]. The presence of the SARS-CoV-2 spike protein in some of the specimens included in this review may also further support this theory.
Although the present scoping review was performed according to the PRISMA-ScR guidelines it has several significant limitations. First, most included records were case reports, yielding only a small number of included patients and thus decreasing the reliability of the results. Moreover, many of the articles did not provide details of the histopathological characteristics and therefore, possible additional characteristics may not have been recorded in this review. Lastly, since the search was limited to articles written in the English language, valuable reports written in other languages might have been excluded.
Conclusions
Our review demonstrated that myocarditis accompanied with inflammatory infiltration and sometimes myocardial necrosis rarely occurs in patients who were vaccinated against COVID-19, particularly with the novel mRNA vaccines. Further studies are required to validate our results. In particular, retrospective cohort studies of unreported past cases may shed some more light on the histopathological features of myocarditis induced by vaccination against SARS-CoV-2.
Conflicts of interest
None to report.
Funding
Not applicable.
References
| 1. |
Cooper LT. Myocarditis. N Engl J Med [Internet]. 2009 Apr 9;360(15):1526–38. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMra0800028.
|
| 2. |
Trachtenberg BH, Hare JM. Inflammatory Cardiomyopathic Syndromes. Circ Res [Internet]. 2017 Sep 15;121(7):803–18. Available from: https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.117.310221.
|
| 3. |
Lampejo T, Durkin SM, Bhatt N, Guttmann O. Acute myocarditis: aetiology, diagnosis and management. Clin Med (Northfield Il) [Internet]. 2021 Sep;21(5):e505–10. Available from: https://www.rcpjournals.org/lookup/doi/10.7861/clinmed.2021-0121.
|
| 4. |
Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson I V., Robicsek A. Myocarditis and Pericarditis After Vaccination for COVID-19. JAMA [Internet]. 2021 Sep 28;326(12):1210. Available from: https://jamanetwork.com/journals/jama/fullarticle/2782900.
|
| 5. |
Salah HM, Mehta JL. COVID-19 Vaccine and Myocarditis. Am J Cardiol [Internet]. 2021 Oct;157:146–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0002914921006391.
|
| 6. |
Ali M, Shiwani HA, Elfaki MY, Hamid M, Pharithi R, Kamgang R, et al. COVID-19 and myocarditis: a review of literature. Egypt Hear J [Internet]. 2022 Dec 5;74(1):23. Available from: https://tehj.springeropen.com/articles/10.1186/s43044-022-00260-2.
|
| 7. |
Ling RR, Ramanathan K, Tan FL, Tai BC, Somani J, Fisher D, et al. Myopericarditis following COVID-19 vaccination and non-COVID-19 vaccination: a systematic review and meta-analysis. Lancet Respir Med [Internet]. 2022 Jul;10(7):679–88. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2213260022000595.
|
| 8. |
Viskin D, Topilsky Y, Aviram G, Mann T, Sadon S, Hadad Y, et al. Myocarditis Associated With COVID-19 Vaccination. Circ Cardiovasc Imaging [Internet]. 2021 Sep;14(9):e013236. Available from: https://www.ahajournals.org/doi/10.1161/CIRCIMAGING.121.013236.
|
| 9. |
Organization WH. Causality assessment of an adverse event following immunization (AEFI): user manual for the revised who classification. 2019; Available from: https://iris.who.int/bitstream/handle/10665/340802/9789241516990-eng.pdf.
|
| 10. |
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med [Internet]. 2018 Oct 2;169(7):467–73. Available from: https://www.acpjournals.org/doi/10.7326/M18-0850.
|
| 11. |
Abete R, Valastro P, Iacovoni A, Vittori C, Arbustini E, Pellicioli F, et al. Acute necrotizing eosinophilic myocarditis presenting with cardiogenic shock after mRNA booster dose for COVID-19: Case report and review of literature. J Cardiol Cases [Internet]. 2023 Feb;27(2):52–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1878540922001712.
|
| 12. |
Aikawa T, Ogino J, Kita Y, Funayama N. Myocardial microthrombi after COVID-19 mRNA vaccination. Eur Heart J [Internet]. 2021 Nov 14;42(43):4501–4501. Available from: https://academic.oup.com/eurheartj/article/42/43/4501/6384671.
|
| 13. |
Ameratunga R, Woon S-T, Sheppard MN, Garland J, Ondruschka B, Wong CX, et al. First Identified Case of Fatal Fulminant Necrotizing Eosinophilic Myocarditis Following the Initial Dose of the Pfizer-BioNTech mRNA COVID-19 Vaccine (BNT162b2, Comirnaty): an Extremely Rare Idiosyncratic Hypersensitivity Reaction. J Clin Immunol [Internet]. 2022 Apr 3;42(3):441–7. Available from: https://link.springer.com/10.1007/s10875-021-01187-0.
|
| 14. |
Baumeier C, Aleshcheva G, Harms D, Gross U, Hamm C, Assmus B, et al. Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series. Int J Mol Sci [Internet]. 2022 Jun 22;23(13):6940. Available from: https://www.mdpi.com/1422-0067/23/13/6940.
|
| 15. |
Bricoli S, Cacciola G, Barocelli F, Guerra C, Zardini M. 553 Myocarditis after COVID-19 vaccination – a case series. Eur Hear J Suppl [Internet]. 2021 Dec 8;23(Supplement_G). Available from: https://academic.oup.com/eurheartjsupp/article/doi/10.1093/eurheartj/suab135.008/6456956.
|
| 16. |
Choi S, Lee S, Seo J-W, Kim M, Jeon YH, Park JH, et al. Myocarditis-induced Sudden Death after BNT162b2 mRNA COVID-19 Vaccination in Korea: Case Report Focusing on Histopathological Findings. J Korean Med Sci [Internet]. 2021;36(40). Available from: https://jkms.org/DOIx.php?id=10.3346/jkms.2021.36.e286.
|
| 17. |
Chow BT, Lai CK. Lymphohistiocytic Myocarditis Possibly Due to Moderna mRNA-1273 Vaccine. Am J Clin Pathol [Internet]. 2022 Aug 4;158(2):167–72. Available from: https://academic.oup.com/ajcp/article/158/2/167/6548250.
|
| 18. |
Dong Y, Liu X, Yang C, Qi Q, Shi W, Li Y, et al. Case report: Myocarditis following COVID-19 protein subunit vaccination. Front Cardiovasc Med [Internet]. 2022 Sep 7;9. Available from: https://www.frontiersin.org/articles/10.3389/fcvm.2022.970045/full.
|
| 19. |
Ehrlich P, Klingel K, Ohlmann-Knafo S, Hüttinger S, Sood N, Pickuth D, et al. Biopsy-proven lymphocytic myocarditis following first mRNA COVID-19 vaccination in a 40-year-old male: case report. Clin Res Cardiol [Internet]. 2021 Nov 6;110(11):1855–9. Available from: https://link.springer.com/10.1007/s00392-021-01936-6.
|
| 20. |
Frustaci A, Verardo R, Galea N, Lavalle C, Bagnato G, Scialla R, et al. Hypersensitivity Myocarditis after COVID-19 mRNA Vaccination. J Clin Med [Internet]. 2022 Mar 16;11(6):1660. Available from: https://www.mdpi.com/2077-0383/11/6/1660.
|
| 21. |
Gill JR, Tashjian R, Duncanson E. Autopsy Histopathologic Cardiac Findings in 2 Adolescents Following the Second COVID-19 Vaccine Dose. Arch Pathol Lab Med [Internet]. 2022 Aug 1;146(8):925–9. Available from: https://meridian.allenpress.com/aplm/article/146/8/925/477788/Autopsy-Histopathologic-Cardiac-Findings-in-2.
|
| 22. |
Kadwalwala M, Chadha B, Ortoleva J, Joyce M. Multimodality imaging and histopathology in a young man presenting with fulminant lymphocytic myocarditis and cardiogenic shock after mRNA-1273 vaccination. BMJ Case Rep [Internet]. 2021 Nov 30;14(11):e246059. Available from: https://casereports.bmj.com/lookup/doi/10.1136/bcr-2021-246059.
|
| 23. |
Mengesha B, Asenov AG, Hirsh-Raccah B, Amir O, Pappo O, Asleh R. Severe Acute Myocarditis after the Third (Booster) Dose of mRNA COVID-19 Vaccination. Vaccines [Internet]. 2022 Apr 8;10(4):575. Available from: https://www.mdpi.com/2076-393X/10/4/575.
|
| 24. |
Mörz M. A case report: Multifocal necrotizing encephalitis and myocarditis after BNT162b2 mRNA vaccination against COVID-19. Vaccines [Internet]. 2022 Oct 1;10(10):1651. Available from: https://www.mdpi.com/2076-393X/10/10/1651.
|
| 25. |
Nakatani S, Ohta-Ogo K, Nishio M, Amemiya K, Sato S, Sawano H, et al. Microthrombosis as a cause of fulminant myocarditis-like presentation with COVID-19 proven by endomyocardial biopsy. Cardiovasc Pathol [Internet]. 2022 Sep;60:107435. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1054880722000291.
|
| 26. |
Nunn S, Kersten J, Tadic M, Wolf A, Gonska B, Hüll E, et al. Case Report: Myocarditis After COVID-19 Vaccination – Case Series and Literature Review. Front Med [Internet]. 2022 Feb 14;9. Available from: https://www.frontiersin.org/articles/10.3389/fmed.2022.836620/full.
|
| 27. |
Olmos CV, Trahan S, Rochon A, Ducharme A. Severe myocarditis after SARS-CoV-2 vaccination in a 49-year-old woman. Can Med Assoc J [Internet]. 2022 Apr 25;194(16):E581–4. Available from: http://www.cmaj.ca/lookup/doi/10.1503/cmaj.211687.
|
| 28. |
Onishi N, Konishi Y, Kaneko T, Maekawa N, Suenaga A, Nomura S, et al. Fulminant myocarditis with complete atrioventricular block after mRNA COVID-19 vaccination: A case report. J Cardiol Cases [Internet]. 2023 May;27(5):229–32. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1878540923000051.
|
| 29. |
Otsuka K, Matsuo T, Ishimatsu T, Fukae A, Hamamoto T, Oku K, et al. A case of BNT162b2 COVID‐19 vaccine‐associated fulminant myocarditis in a very elderly woman. Clin Case Reports [Internet]. 2022 Sep 5;10(9):e6161. Available from: https://onlinelibrary.wiley.com/doi/10.1002/ccr3.6161.
|
| 30. |
Satomi H, Katano H, Kanno H, Kobayashi M, Ohkuma Y, Hashidume N, et al. An autopsy case of fulminant myocarditis after severe acute respiratory syndrome coronavirus 2 vaccine inoculation. Pathol Int [Internet]. 2022 Oct 30;72(10):519–24. Available from: https://onlinelibrary.wiley.com/doi/10.1111/pin.13267.
|
| 31. |
Schwab C, Domke LM, Hartmann L, Stenzinger A, Longerich T, Schirmacher P. Autopsy-based histopathological characterization of myocarditis after anti-SARS-CoV-2-vaccination. Clin Res Cardiol [Internet]. 2023 Mar 27;112(3):431–40. Available from: https://link.springer.com/10.1007/s00392-022-02129-5.
|
| 32. |
Arushi S, Shanil S, Alampoondi VSV, Qiying D, L. HM. Lymphohistiocytic myocarditis following SARS-COV-2 vaccine. J Am Coll Cardiol [Internet]. 2022 Mar 8;79(9_Supplement):3384. Available from: https://doi.org/10.1016/S0735-1097(22)04375-3.
|
| 33. |
Stervbo U, Van Bracht M, Philippou S, Babel N, Westhoff TH. Case report: SARS-CoV-2 specific T-cells are associated with myocarditis after COVID-19 vaccination with mRNA-1273. Front Med [Internet]. 2023 Mar 3;10. Available from: https://www.frontiersin.org/articles/10.3389/fmed.2023.1088764/full.
|
| 34. |
Yamamoto M, Tajiri K, Ayuzawa S, Ieda M. Pathological findings of clinically suspected myocarditis temporally associated with COVID‐19 vaccination. Eur J Heart Fail [Internet]. 2022 Jun 15;24(6):1132–8. Available from: https://onlinelibrary.wiley.com/doi/10.1002/ejhf.2523.
|
| 35. |
Kühl U, Schultheiss H. Viral myocarditis. Swiss Med Wkly [Internet]. 2014 Oct 2; Available from: https://smw.ch/index.php/smw/article/view/1906.
|
| 36. |
Chen W, Pan JY. Anatomical and Pathological Observation and Analysis of SARS and COVID-19: Microthrombosis Is the Main Cause of Death. Biol Proced Online [Internet]. 2021;23(1):4. Available from: https://doi.org/10.1186/s12575-021-00142-y.
|
| 37. |
Huber S. Viral myocarditis and dilated cardiomyopathy: etiology and pathogenesis. Curr Pharm Des [Internet]. 2016;22(4):408–26. Available from: https://www.ingentaconnect.com/content/ben/cpd/2016/00000022/00000004/art00002.
|
| 38. |
Kadkhoda K. Post RNA-based COVID vaccines myocarditis: Proposed mechanisms. Vaccine [Internet]. 2022 Jan;40(3):406–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X21015942.
|