Abstract
Low back-pain is the most common pain syndrome. Radiofrequency facet denervation (RFD) is a minimally invasive method of treatment of chronic low back pain caused by facet joint syndrome. In this procedure electric current with frequency of radio waves are used to cause thermal injury to a small branch nerve that innervates painful facets. There are numerous studies confirming the effectiveness of this therapy. A good outcome of RFD can be sustained by appropriate and regular exercise. The aim of this article is to recommend such a program of exercises focused on strengthening the muscles and improving stabilization of the lumbar spine.
Citation
Broda M, Miler J, Jankowski K, Rogowski B, Krakowiak M, Sokal P. Interdisciplinary interventional and physiotherapy management of facet joint syndrome. Eur J Transl Clin Med. 2023;6(2):78-84Abbreviations
- LBP – low-back pain
- IJ – intervertebral joints
- FJS – facet joint syndrome
- RFD – lumbar radiofrequency denervation
Introduction
Low back pain (LBP) is the most common pain syndrome. Diagnosing the cause of LBP is challenging due to its numerous etiologies. Maas et al. reported that lower back pain was classified as “non-specific” in 85-90% of cases [1]. LBP is the second most common reason for years lived with disability [2]. Rubin described that 50-80% of adults experience back pain at least once in their lifetime and 15-20% of adults struggle with back pain at least once a year [3]. Frosch et al. indicated that the prevalence of non-specific back pain was increasing among children and adolescents [4]. Yang et al. reported that that 80% of adolescents with LBP could not be clearly diagnosed within a year and the most common final diagnoses were muscle cramps, scoliosis, lumbar degenerative disc disease or disc herniation [5]. Andersson reported that > 50% cases of LBP resolved spontaneously within 2-4 weeks and 90% by 12 weeks. In another study, he reported that 60‑70% recovered within 6 weeks and 80-90% in 12 weeks [6]. In another study, spontaneous resolution of LBP of disc origin occurred after 2.33 ± 1.23 months [7]. In their review Chiu et al. reported that the rate of spontaneous resolution of lower back pain was to be 96% for disc sequestration, 70% for disc extrusion, 41% for disc protrusion, and 13% for disc bulging and the rate of complete resolution of disc herniation was 43% for sequestrated discs and 15% for extruded discs [8].
A significant number of employees complain of back pain and it is one of the main reasons for absence or resignation from work. Based on data from ZUS (Zakład Ubezpieczeń Społecznych, the institution responsible for social insurance in Poland), cervical pain was the main reason for work absence (51% of employees in Poland), 34% cited LBP and 18% cited thoracic spine pain [9]. The statistical age of patients who seek medical consult due to back pain is systematically decreasing in Poland. The average Polish patient with medically confirmed back pain is currently on average 46 years of age (age ranged from 7 to 95 years of age [9]. Statistics from other European countries show that 10-15% of sick leave from work is due to back pain [6]. Stewart et al. indicate that in the United States LBP is the second most common cause of absenteeism/lost productive time (right after headache) due to pain [10]. Savari et al. showed that the most common reasons for work absence (after respiratory system diseases) were skeletal system diseases (neck and back pains accounted for 12.3% of absences at work) and the most predisposed group was age 20-39 years [11]. The above data clearly shows the scale of the problem that affects our society.
Facet joint syndrome versus radicular pain
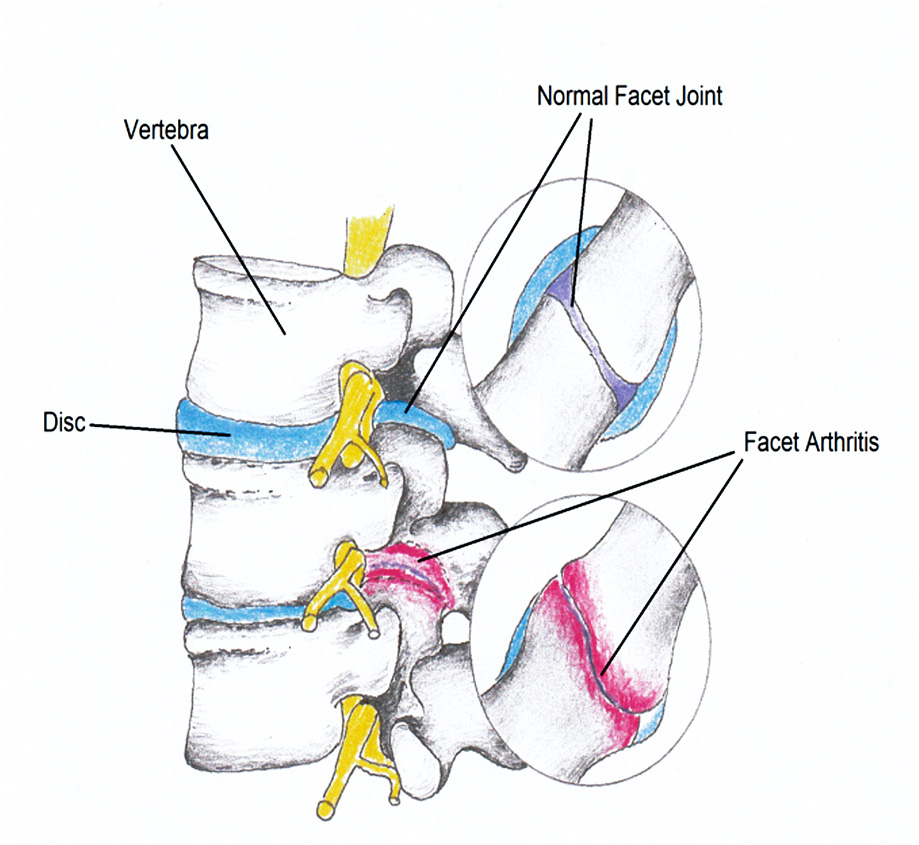
When diagnosing a patient, the source of the LBP must be correctly located, which increases the chances of success treatment results. The intervertebral joints (IJ) of the lumbar spine are a common source of pain, accounting for 15-45% of cases apart from other structures like intervertebral discs, sacroiliac joints, and nerve roots [12]. Osteoarthritis of the lumbar spine is the most common cause of intervertebral joint pain (Figure 1). Facet joint syndrome (FJS), also known as facet joint disease, is associated with local pain in the lower back, rarely radiating to the leg. The causes of FJS are: heavy physical work, scoliosis, spondylolisthesis and obesity [13]. It is noteworthy that not every case of chronic LBP originates in the IJ. FJS is related to age and occurs most commonly between the ages of 51 and 60 [12].
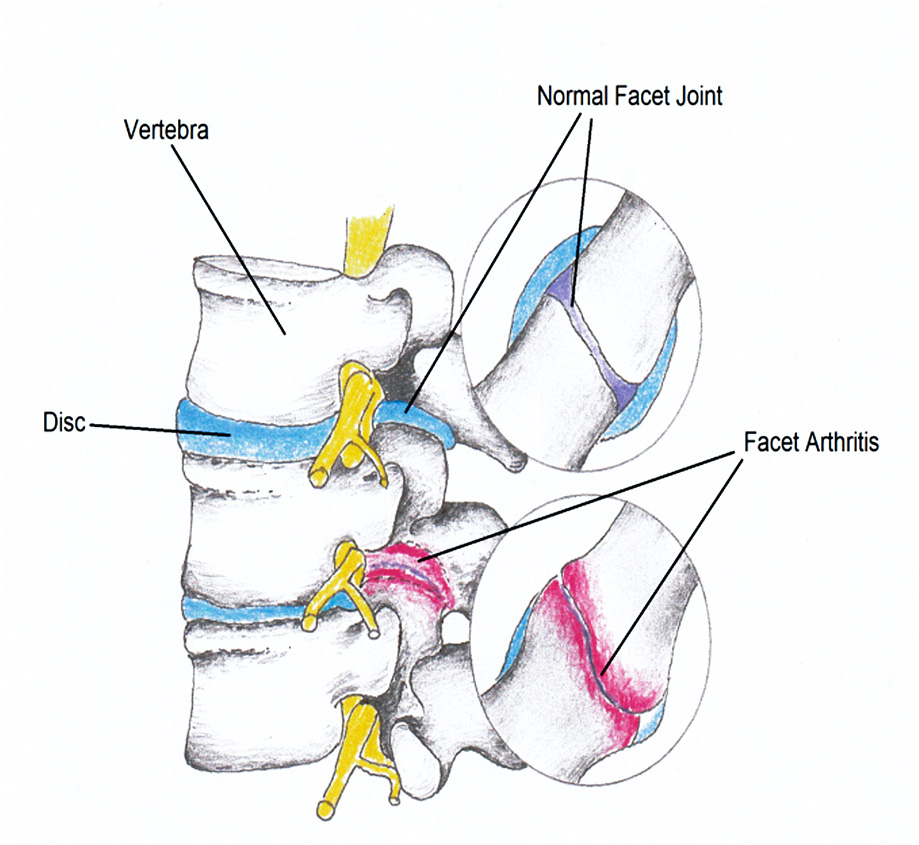
Figure 1. Facet joint syndrome is caused by osteoarthitis of an intervertebral joint which is the source of pain
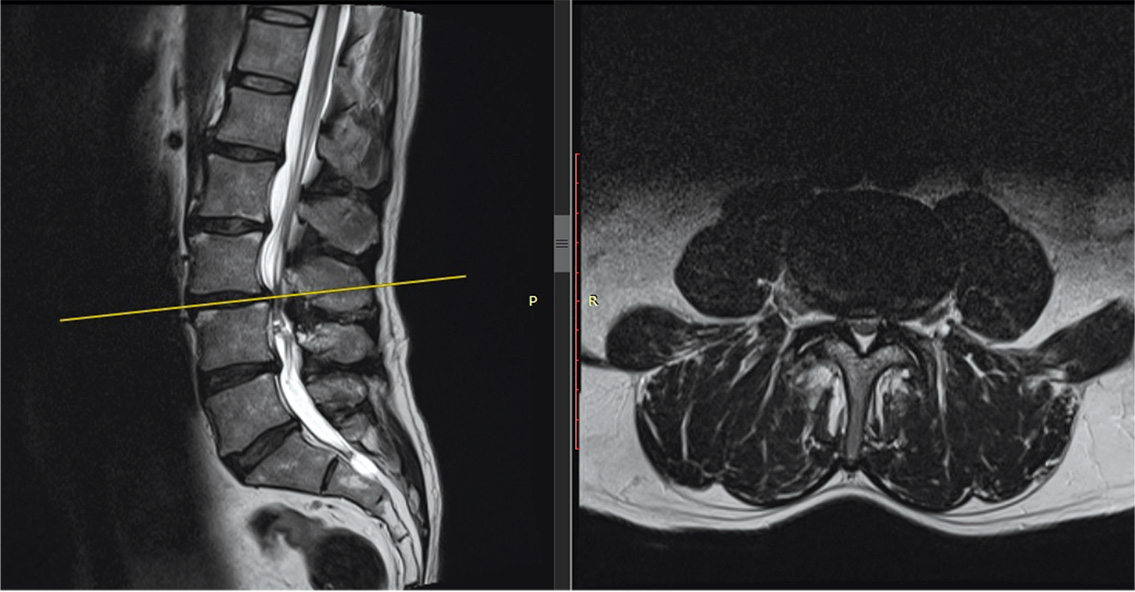
Radicular pain is characterized by severe, shooting pain radiating to the extremities. This is accompanied by neurological symptoms such as sensory disturbances, paraesthesia and muscle weakness. Clinical symptoms of lumbosacral radicular syndrome usually result from irritation of L4, L5, S1 roots. Radicular syndromes are most often caused by compression of the spinal roots near the entrance to the intervertebral foramen, the narrowest part of this opening, which is most easily narrowed in the course of degenerative changes of the spine (Figure 2). The second most common cause of spinal root compression is disc displacement [14].
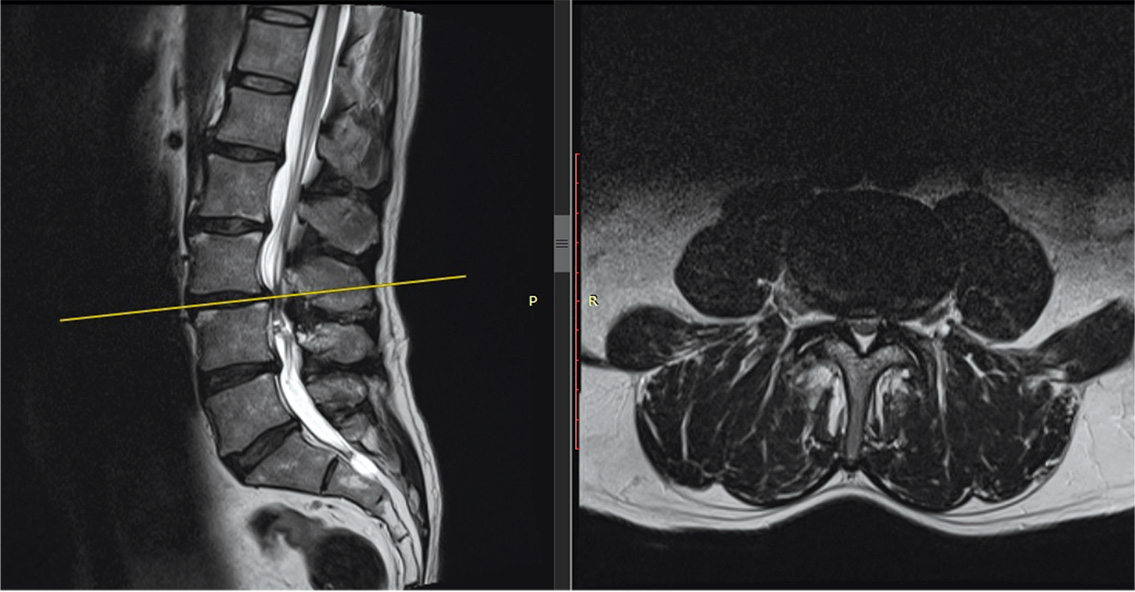
Figure 2. Narrowed spinal canal recess or intervertebral foramen are the causes of compression of the nerve root which is the source of radicular pain
Lumbar denervation procedure
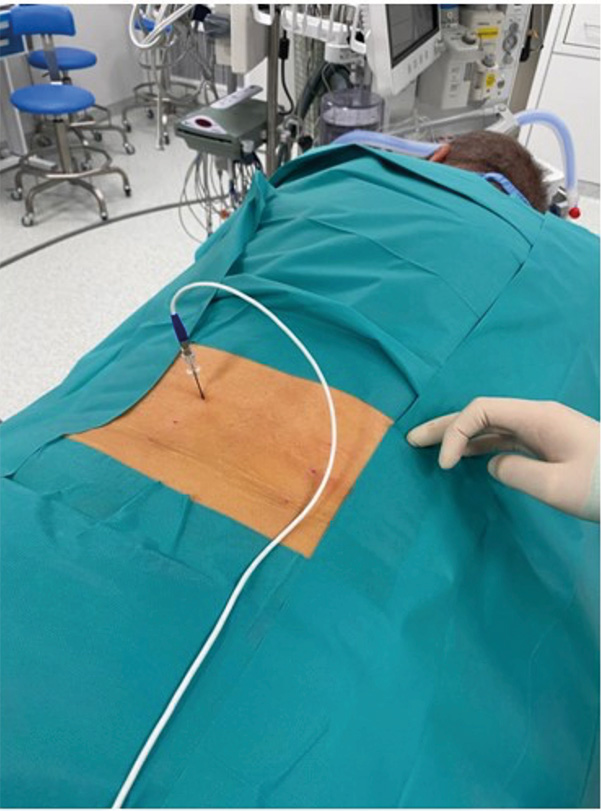
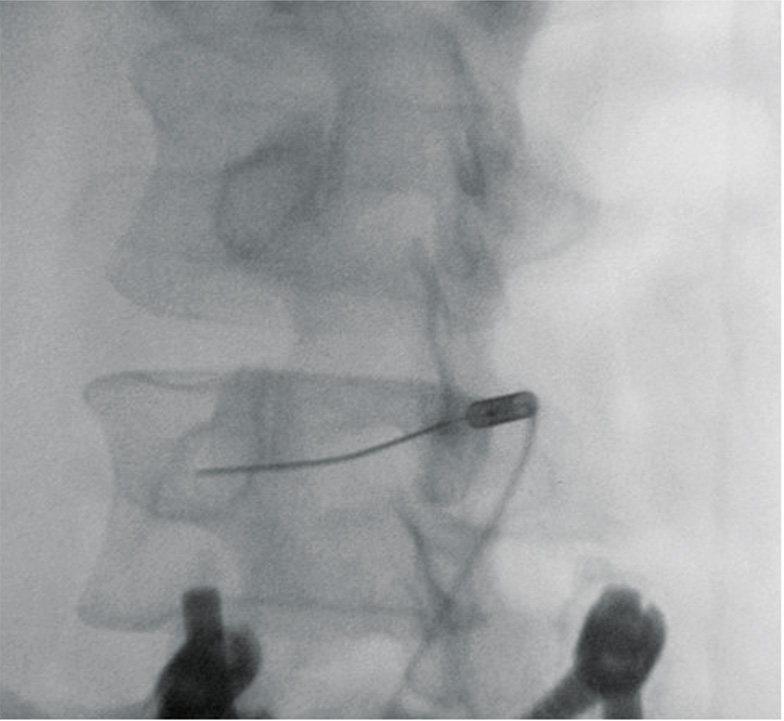
Lumbar radiofrequency denervation (RFD) is a minimally invasive treatment for chronic LBP that involves targeted percutaneous nerve injury using 300-500 kHz heat-generation for precise and long-lasting pain relief. The indication for this procedure is chronic LBP lasting at least 6 months that cannot be relieved by conventional treatment e.g. analgesics and physiotherapy. The advantage of RFD is its precision, reproducibility regardless of the patient’s age and relatively few contraindications (e.g. heart failure, pregnancy, inflammatory skin changes and certain mental diseases, particularly depression secondary to chronic pain) [15]. The RFD procedure can be performed safely approximately 3 months after stroke and myocardial infarction [16]. See Figure 3-5 for an RDF procedure for faucet joint syndrome.
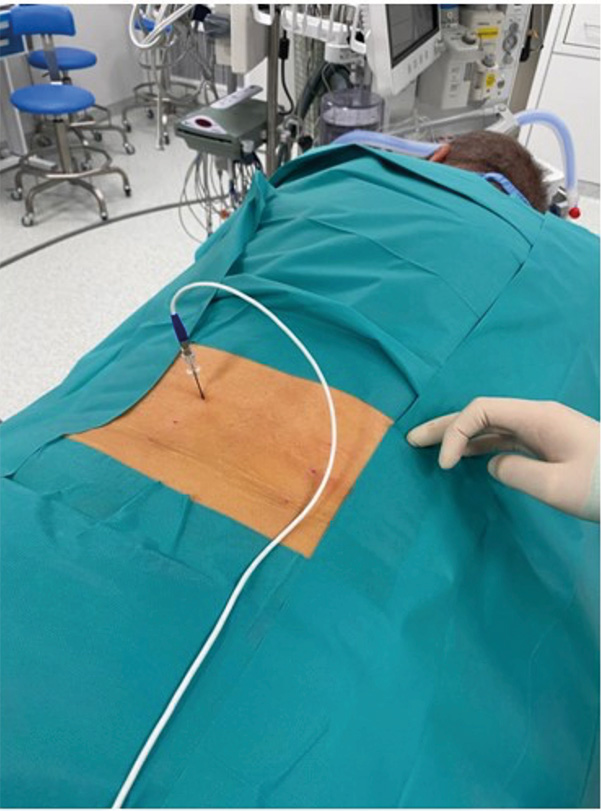
Figure 3. RFD the in operating room under fluoroscopy
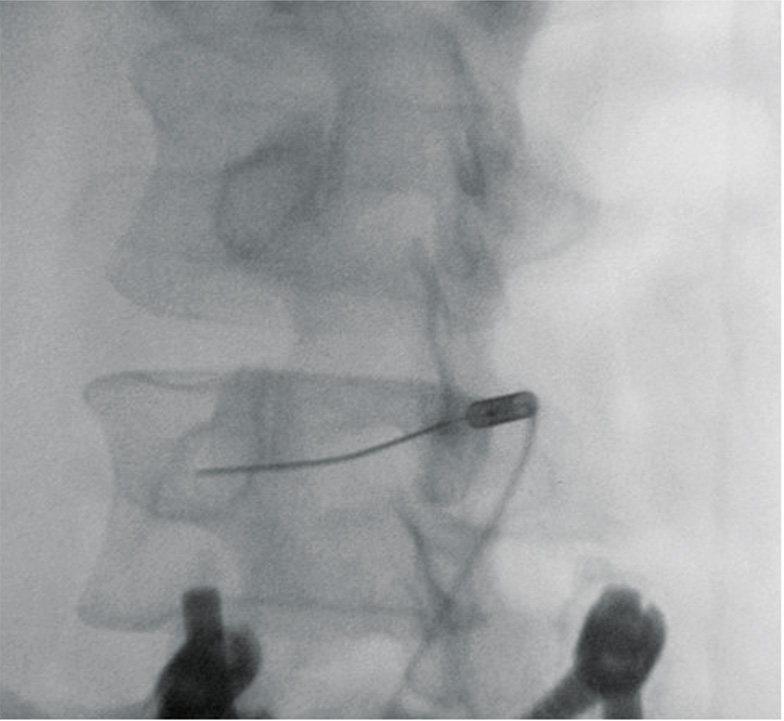
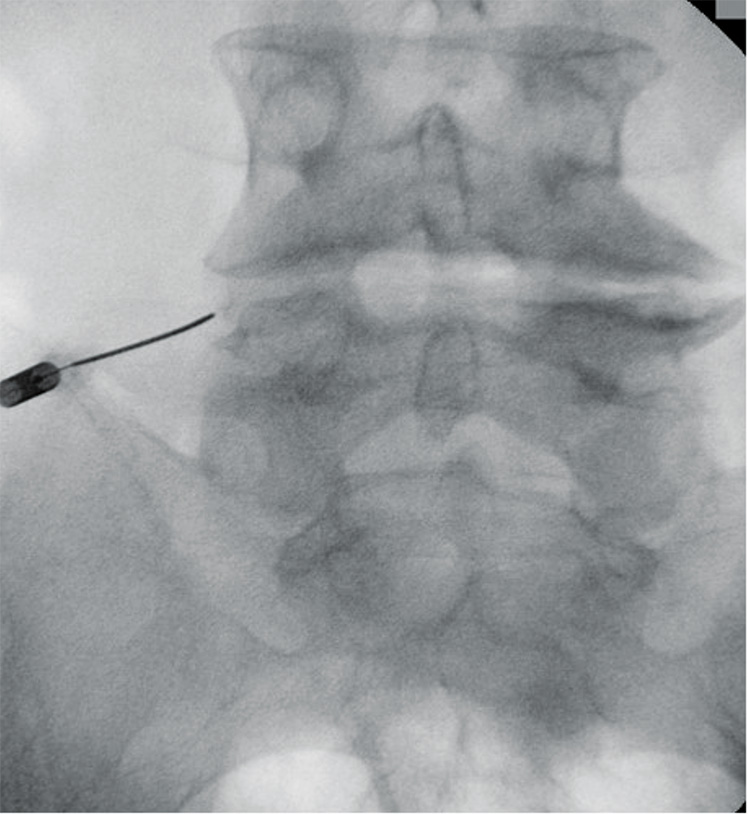
Figure 4. Oblique X-ray of lumbar spine with the needle and electrode lead inserted in the so-called “eye of the scottie dog”
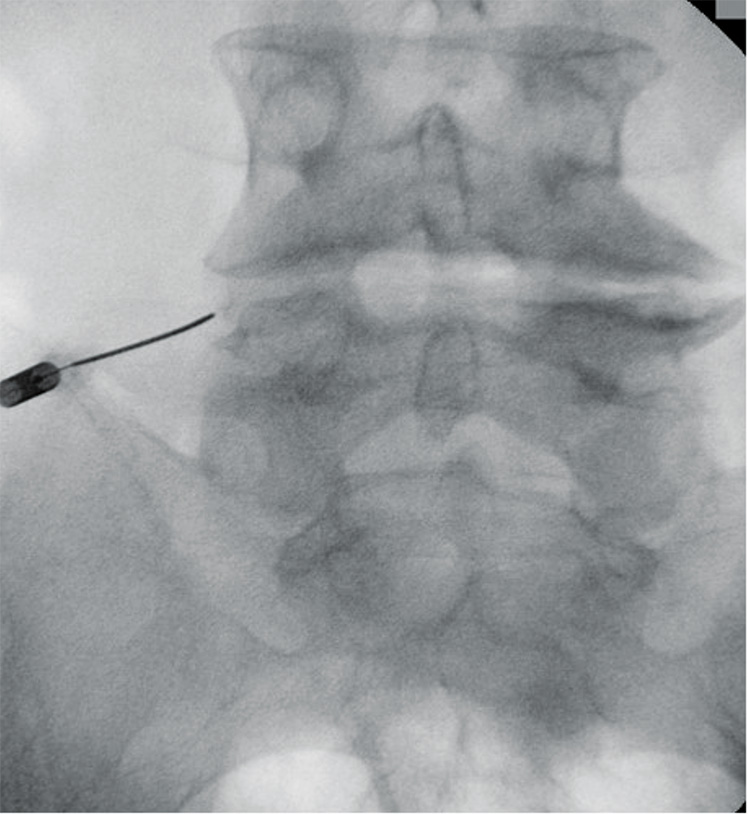
Figure 5. A-P X-ray of the electrode placed on left transverse process of L5
Efficacy of lumbar facet RFD
In a study on 1309 patients with chronic LBP, RFD was shown to provide only short-term pain relief for patients with pain of disc origin, while it was more effective for FJS [1]. Adakli et al demonstrated, comparing RFD with Target Disc Decompression, that RFD was an attractive alternative to conventional surgery for the treatment of radicular symptoms [17]. Pain relief was reported by 41.7% of patients undergoing RFD. In a study on the efficacy of RFD for discogenic lumbar spine pain, Zhang et al noted pain relief in 65% of patients in the first week after treatment, 17 (74%) at 1 month, 18 (78%) at 3 months, 19 (82%) at 6 months, and up to 87% of patients at 12 weeks after treatment [18]. Arici et al. included in their study 164 patients with LBP due to lumbar arthropathy, who underwent RFD and at least 50% of noted pain relief and 68% had good to excellent results. The median time of relief after the procedure was 7.3 months, with 10.2 months for patients with good/excellent results [19]. In a Korean study on 30 patients with discopathy or spinal stenosis underwent RFD, of whom 17 patients scored ‘excellent’ according to the MacNab criteria, 11 scored ‘good’ and the remaining 2 patients scored ‘fair.’ The patients were also assessed with VAS and Oswestry scales in which they showed significant improvement [20]. In their double-blind study, Ertival et al. subjected 96 patients in 3 randomized groups to RFD with different parameters in terms of temperature and time. The results, regardless of the parameters used, were good (pain relief > 50% in 57% of patients), but were worse in patients who had previously undergone spinal procedures [21]. Masala et al. found significant lumbar pain relief in 70%-81% of patients with FJS [22]. Similar results were also found by Hee Son et al. (85% of patients experienced pain relief) [23] and MacVicar et al. (58% and 53% of patients had a positive treatment outcome) [24].
Physiotherapy approach after RFD treatment on FJS
RFD has been demonstrated to relieve LBP, allowing patients to resume independent daily activities and work. This minimally invasive technique allows patients to start physiotherapy after a week in the form of physical exercises. Patients with LBP tend to have abnormally reduced paraspinal muscle tone caused by long-term chronic overload pain resulting from poor spinal alignment. Therefore, correct body posture and proper shaping of the lumbar lordosis are important [25]. It is important to educate the patient, to implement the correct body posture in everyday activities and the correct sitting position while working in a sitting position, e.g. at the desk. Regular exercises strengthen the lumbar muscles and improve the stabilization of the lumbar spine by correcting its position (from deepened to normal), all of which reduce LBP [26]. The lumbar spine is exposed to heavy loads, and thanks to proper physical activity, we can avoid overload. The greatest pressure is exerted on them during forward tilting of the lumbar spine (lordosis) and rotation of the trunk and pelvis. Active exercises performed regularly, activating the deep muscles of the trunk and aimed at restoring the proper tension and coordination of paraspinal muscles in the lumbar spine [27].
Proper exercise by the patient is based on the principle of performing exercises without increasing pain, gradually increasing the range of motion in the joints of the spine, only to the limit of pain. Regular, daily exercise should be done in isolated, safe positions. Change of exercise position should take place with a stiffened spine. During exercises, the patient should maintain deep breaths by inhaling through the nose and exhaling through the mouth. The effectiveness of individual exercises in terms of reducing pain and improving the patient’s functionality has also been demonstrated in other studies [28-29]. Performing RDF treatment in a patient with LBP and performing regular physical exercises under the supervision of a physiotherapist an extend the therapeutic effect of RDF treatment in the form of life without LBP symptoms. See Figure 6-10 for a sample set of exercises for patients after RFD.

Figure 6. Exercise 1*. While in the supine position, with arms along the torso, knees flexed, raise the pelvis, hold position for 7 seconds, lower the pelvis.

Figure 7. Exercise 2*. While lying down, use the right heel to touch the left knee and repeat with opposite heel and knee.

Figure 8. Exercise 3*. Cat (back) stretch. Inhale while pushing the spine towards the ceiling, exhale while lowering the spine to the starting position.

Figure 9. Exercise 4*. Arch supports while in the prone position. Hold this position for a few seconds, preferably while inhaling.

Figure 10. Exercise 5*. While in the prone position, put your hands on your hips and try to “stick your head” as far as possible in front of you lifting it slightly from the floor.
_____
* The person shown in figures 6-10 is one of the co-authors of this article, and gave his informed consent to publish this photographs.
Conclulsions
A good outcome of facet joint denervation can be maintained with an appropriate, regular program of exercises to strengthen the muscles and improve the stabilization of the lumbar spine. The exercises described in this article are exemplary. Patients must stay in contact with their doctor or physiotherapist, who work closely together. Combining the RFD treatment with physiotherapy will probably prolong the therapeutic effect and get rid of chronic low back pain. Therefore, it should be remembered that the form of exercise should always be individual and adapted to the current physical condition of the patient.
References
| 1. |
Maas ET, Ostelo RWJG, Niemisto L, Jousimaa J, Hurri H, Malmivaara A, et al. Radiofrequency denervation for chronić low back pain. Cochrane database Syst Rev [Internet]. 2015;2015(10):CD008572. Available from: http://doi.wiley.com/10.1002/14651858.CD008572.pub2.
|
| 2. |
The Lancet. GBD 2017: a fragile world. Lancet [Internet]. 2018;392(10159):1683. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673618328587.
|
| 3. |
Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin [Internet]. 2007;25(2):353–71. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0733861907000059.
|
| 4. |
Frosch M, Mauritz MD, Bielack S, Blödt S, Dirksen U, Dobe M, et al. Etiology, risk factors, and diagnosis of back pain in children and adolescents: evidence- and consensus-based interdisciplinary recommendations. Children [Internet]. 2022;9(2):192. Available from: https://www.mdpi.com/2227-9067/9/2/192.
|
| 5. |
Yang S, Werner BC, Singla A, Abel MF. Low back pain in adolescents: a 1-year analysis of eventual diagnoses. J Pediatr Orthop [Internet]. 2017;37(5):344–7. Available from: https://journals.lww.com/01241398-201707000-00016.
|
| 6. |
Andersson GB. Epidemiological features of chronic low-back pain. Lancet [Internet]. 1999;354(9178):581–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673699013124.
|
| 7. |
Akpinar A, Akintürk N, Kilinç BM, Kasap M. Spontaneous regression of lumbar disc herniations. J Turkish Spinal Surg [Internet]. 2020;31(3):141–7. Available from: http://cms.galenos.com.tr/Uploads/Article_39992/jtss-31-141-En.pdf.
|
| 8. |
Chiu C-C, Chuang T-Y, Chang K-H, Wu C-H, Lin P-W, Hsu W-Y. The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clin Rehabil [Internet]. 2015;29(2):184–95. Available from: http://journals.sagepub.com/doi/10.1177/0269215514540919.
|
| 9. |
Zheltoukhova K, Bevan S, Reich A. Fit for work? Musculoskeletal disorders and the Polish labour market [Internet]. London; 2012. Available from: https://www.ceestahc.org/pliki/projekty/f4w/poland_English_060911.pdf.
|
| 10. |
Stewart WF. Lost productive time and cost due to common pain conditions in the US workforce. JAMA [Internet]. 2003;290(18):2443. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.290.18.2443.
|
| 11. |
Saravi B, Kabirzadeh A, Rezazadeh E, Khariki M, Zolaykha Z, Asgari A, et al. Prevalence and causes of medical absenteeism among staff (case study at Mazandaran University of Medical Sciences: 2009-2010). Mater Socio Medica [Internet]. 2013;25(4):233. Available from: http://www.scopemed.org/fulltextpdf.php?mno=47883.
|
| 12. |
Manchikanti L, Manchikanti KN, Cash KA, Singh V, Giordano J. Age-related prevalence of facet-joint involvement in chronić neck and low back pain. Pain Physician [Internet]. 2008;11(1):67. Available from: https://www.painphysicianjournal.com/current/pdf?article=OTQ1&journal=39.
|
| 13. |
Perolat R, Kastler A, Nicot B, Pellat J-M, Tahon F, Attye A, et al. Facet joint syndrome: from diagnosis to interventional management. Insights Imaging [Internet]. 2018;9(5):773–89. Available from: https://insightsimaging.springeropen.com/articles/10.1007/s13244-018-0638-x.
|
| 14. |
Koszewicz M, Budrewicz S. Elektrofizjologiczna diagnostyka zespołów korzeniowych [in Polish]. Pol Przegląd Neurol [Internet]. 2010;6(2):86–91. Available from: https://journals.viamedica.pl/polski_przeglad_neurologiczny/article/view/19938.
|
| 15. |
Drobnik L, Kowalski G. Analgezja regionalna. Skrypt [in Polish]. Poznań: Szkoła Analgezji Regionalnej; 2012.
|
| 16. |
Raszka A, Waliszewska R, Sokal P, Zieliński P, Harat M. Quality of life in patients after lumbar thermolesion. J Neurol Neurosurg Nurs [Internet]. 2016;5(2):76–80. Available from: https://apcz.umk.pl/PNIN/article/view/38583.
|
| 17. |
Adakli B, Cakar Turhan KS, Asik I. The comparison of the efficacy of radiofrequency nucleoplasty and targeted disc decompression in lumbar radiculopathy. Biomol Biomed [Internet]. 2015;15(2):57–61. Available from: https://www.bjbms.org/ojs/index.php/bjbms/article/view/427.
|
| 18. |
Zhang L, Ding X-L, Zhao X-L, Wang J-N, Li Y-P, Tian M. Fluoroscopy-guided bipolar radiofrequency thermocoagulation treatment for discogenic low back pain. Chin Med J (Engl) [Internet]. 2016;129(19):2313–8. Available from: https://journals.lww.com/00029330-201610050-00008.
|
| 19. |
Arici T. Distal approach for percutaneous radiofrequency thermocoagulation of lumbar medial branches in patients with lumbar facet arthropathy: a retrospective analysis. Ağrı – J Turkish Soc Algol [Internet]. 2019;32(1):31–7. Available from: http://www.agridergisi.com/jvi.aspx?pdir=agri&plng=eng&un=AGRI-15921.
|
| 20. |
Kim HS, Wu PH, Jang I-T. Lumbar degenerative disease part 1: anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: a prospective case series and review of lite. Int J Mol Sci [Internet]. 2020;21(4):1483. Available from: https://www.mdpi.com/1422-0067/21/4/1483.
|
| 21. |
Ertilav E, Aydin ON, Erel KV. Facet median branch radiofrequency thermocoagulation treatment at different temperatures and durations in patients with lumbar facet syndrome: a randomized controlled, double-blind study. Turk Neurosurg [Internet]. 2021;32(1):149–54. Available from: http://www.turkishneurosurgery.org.tr/summary_en_doi.php3?-doi=10.5137/1019-5149.JTN.34637-21.2.
|
| 22. |
Masala S, Nano G, Mammucari M, Marcia S, Simonetti G. Medial branch neurotomy in low back pain. Neuroradiology [Internet]. 2012;54(7):737–44. Available from: http://link.springer.com/10.1007/s00234-011-0968-6.
|
| 23. |
Son JH, Kim SD, Kim SH, Lim DJ, Park JY. The efficacy of repeated radiofrequency medial branch neurotomy for Lumbar Facet Syndrome. J Korean Neurosurg Soc [Internet]. 2010;48(3):240. Available from: http://jkns.or.kr/journal/view.php?-doi=10.3340/jkns.2010.48.3.240.
|
| 24. |
MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Lumbar medial branch radiofrequency neurotomy in New Zealand. Pain Med [Internet]. 2013;14(5):639–45. Available from: https://academic.oup.com/painmedicine/article-lookup/doi/10.1111/pme.12000.
|
| 25. |
Maeo S, Takahashi T, Takai Y, Kanehisa H. Trunk muscle activities during abdominal bracing: comparison among muscles and exercises. J Sports Sci Med [Internet]. 2013;12(3):467–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24149153.
|
| 26. |
Aleksiev AR. Ten-year follow-up of strengthening versus flexibility exercises with or without abdominal bracing in recurrent low back pain. Spine (Phila Pa 1976) [Internet]. 2014;39(13):997–1003. Available from: http://journals.lww.com/00007632-201406010-00002.
|
| 27. |
Saragiotto BT, Maher CG, Yamato TP, Costa LO, Menezes Costa LC, Ostelo RW, et al. Motor control exercise for chronić non-specific low-back pain. Cochrane Database Syst Rev [Internet]. 2016;2016(11). Available from: http://doi.wiley.com/10.1002/14651858.CD012004.
|
| 28. |
Chambon X, Paysant J, Maureira J., André J. Étude comparative et préliminaire d’un réentraînement à l’effort au sein de deux populations de sujets déconditionnés douloureux ou non [in French]. Ann Réadaptation Médecine Phys [Internet]. 2003;46(4):198–204. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0168605403000552.
|
| 29. |
Chatzitheodorou D, Kabitsis C, Malliou P, Mougios V. A pilot study of the effects of high-intensity aerobic exercise versus passive interventions on pain, disability, psychological strain, and serum cortisol concentrations in people with chronic low back pain. Phys Ther [Internet]. 2007;87(3):304–12. Available from: https://academic.oup.com/ptj/article/87/3/304/2742120.
|