Abstract
Background: In 2020, Polish experts recommended the use of the guidelines of the American Association of Clinical Endocrinologist and the American College of Endocrinology (AACE/ACE) in the diagnosis of obesity instead of the 1998 WHO criteria. Thus, obesity can be also diagnosed in patients with BMI 25.0-29.9 if there are complications related to the excess body weight including infertility and hypogonadism, asthma, sleep apnea, gastroesophageal reflux disease, stress urinary incontinence, osteoarthritis and depression.
Material and methods: The aim of the study was to assess the prevalence of obesity diagnosed according to the new criteria in the group of Polish social media users.
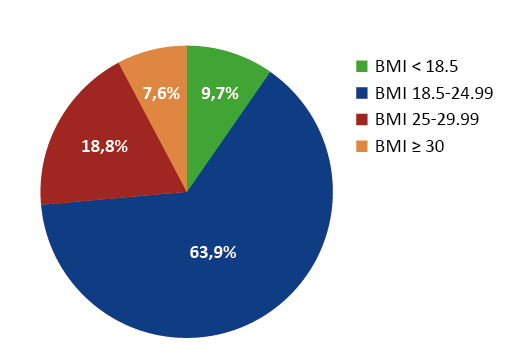
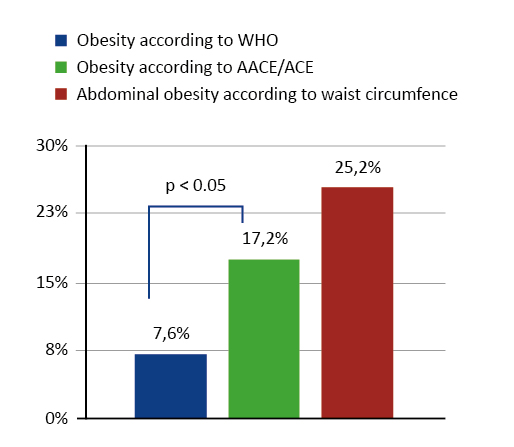
Results: Among the respondents, 9.7% had a BMI below 18.5 kg/m2, 63.9% declared normal BMI, and 18.8% had BMI 25.0-29.9 kg/m2. The value of BMI ≥ 30 kg/m2, equivalent to the diagnosis of obesity according to WHO, was found in 7.6% of the respondents. For comparison, the prevalence of obesity according to the AACE/ACE criteria was more than twice as high (17.2%, p < 0.05).
Conclusions: Concluding, according to the new criteria, more respondents were diagnosed with obesity compared to WHO criteria. The results of the study indicate that the application of the new diagnostic criteria may enable earlier diagnosis and thus earlier treatment of obesity.
Citation
Samek G, Szulc A, Dardzińska J A. The prevalence of obesity diagnosed by different diagnostic criteria in Polish social-media users. Eur J Transl Clin Med. 2023;6(1):25-30Introduction
In accordance with the World Health Organization (WHO), obesity is a chronic disease with a complex etiology and serious consequences [1]. This is undoubtedly demonstrated during the current SARS-CoV-2 pandemic as obese people have a more severe course and a longer duration of coronavirus infection due to immunodeficiency secondary to obesity. Other common complications of obesity, e.g. type 2 diabetes, left ventricular hypertrophy, hypertension and heart failure and prothrombotic state also contributed to a vastly increased risk of hospitalization or even death from COVID-19 in this group of patients [2-6]. Unfortunately, as if that were not enough, obesity is also associated with a psychological burden, such as lowered self-esteem, depressed mood, decreased quality of life and emotional stress, all of which can significantly interfere with treatment [7-8]. On the other hand, exposure to chronic stress may promote the development of obesity. One of the mechanisms involved may be the compensation of negative emotions with food [2, 8]. Increasingly, overeating is a way to reduce anxiety and improve mood [9-10]. Obesity is considered serious public health problem and ranks fifth as the world՚s leading cause of death. The WHO predicts that by 2030 as many as 30% of deaths around the world will be initiated by diseases of civilization. This process can only be stopped by properly identifying diseases, addressing related risk factors and a policy of behavioral involvement. Therefore, early diagnosis of obesity is crucial for effective multimodal treatment [11].
According to the 1998 WHO criteria, the body mass index (BMI) is the most widely used tool in the diagnosis of obesity [1]. However, this tool has many disadvantages [2, 8, 12]. Most importantly, the BMI does not address the distribution of body fat, while it is known that a relevant percentage of adults who are overweight but have BMI < 30 kg/m2 experience complications from excess visceral fat [13-15]. According to the research and data of the Statistics Poland (Główny Urząd Statystyczny), in 2020 BMI ≥ 30 kg/m2 concerned 18.5% of the Polish society [16]. These data are overwhelming, but it should be noted that BMI 25.0-29.9 was found in a much larger group of nearly 19 million Polish citizens [16]. Unfortunately, patients with such BMI are considered overweight and not obese, thus may be overlooked by general practitioners.
Therefore, attention should be paid to the new guidelines for the diagnosis of obesity presented by the American Association of Clinical Endocrinologists and the American College of Endocrinology (AACE/ACE) in 2016 [17] and recommended for Polish patients in 2020 by the Polish Association for the Study of Obesity (PTBO) [2]. These guidelines are not based solely on BMI, but also take into account the presence of diseases and clinical conditions that may be metabolic consequences of excess body fat, such as metabolic syndrome and insulin resistance, type 2 diabetes, cardiovascular disease, arterial hypertension, dyslipidemia, non-alcoholic fatty liver disease, female infertility, polycystic ovary syndrome, male hypogonadism, asthma, sleep apnea syndrome, hypoventilation syndrome, gastroesophageal reflux disease, osteoarthritis, stress urinary incontinence and depression [2, 17]. Obesity can be diagnosed in people with a BMI in the range of 25.0-29.9 if they also have one of the aforementioned complications [2, 17]. Thus, the new guidelines allow for an earlier diagnosis of obesity and consequently a more rapid implementation of treatment.
The main aim of our work was to rate the prevalence of obesity diagnosed according to these new criteria and to compare the results with the WHO criteria. Due to the limitations associated with the pandemic, social media users were selected for this pilot study.
Material and methods
This was an online retrospective observational survey conducted using social media in February and March 2022, during one of the waves of the SARS-CoV-2 pandemic in Poland and the outbreak of the war in Ukraine. Participation in the study was unsolicited and did not involve any financial benefits. The only inclusion criteria were age over 18 and consent to participate in the examination.
In the survey we asked about the respondents’ place of residence, education, socioeconomic status, current weight, height, waist circumference and changes in body weight over the past two years, medication used and the presence of complications of obesity that are listed above. The survey link was shared via various social media and applications (Facebook, Instagram and WhatsApp), to ensure that a diverse group of participants could be reached.
BMI was calculated based on the height and weight provided by the respondents. Based on their BMI, the respondents were classified into following four groups: underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5-24.99 kg/m2), overweight (BMI 25-29.99 kg/m2) and obese (BMI ≥ 30.0 kg/m2).
Obesity was diagnosed according to one of the following criteria:
- If the BMI ≥ 30.0 kg/m2 (WHO) [1],
- If the declared waist circumference were at ≥ 80 cm in women and ≥ 94 cm in men (International Diabetes Federation) [18],
- If BMI in the range of 25.0-29.9 kg/m2 and the respondent declared having at least one of the complications of obesity listed in the AACE/ACE guidelines [2, 17].
All statistical calculations were done by using the Statistica software (version 13.3, StatSoft, USA). Quantitative variables were presented as the mean and standard deviation (SD) and qualitative variables were presented in terms of numbers or percentages. The significance of differences between the two groups (model of unrelated variables) was tested by Student՚s t-test or the U Mann-Whitney test. Chi-square tests of independence were used for qualitative variables. The significance level of p = 0.05 was assumed in all calculations.
Results
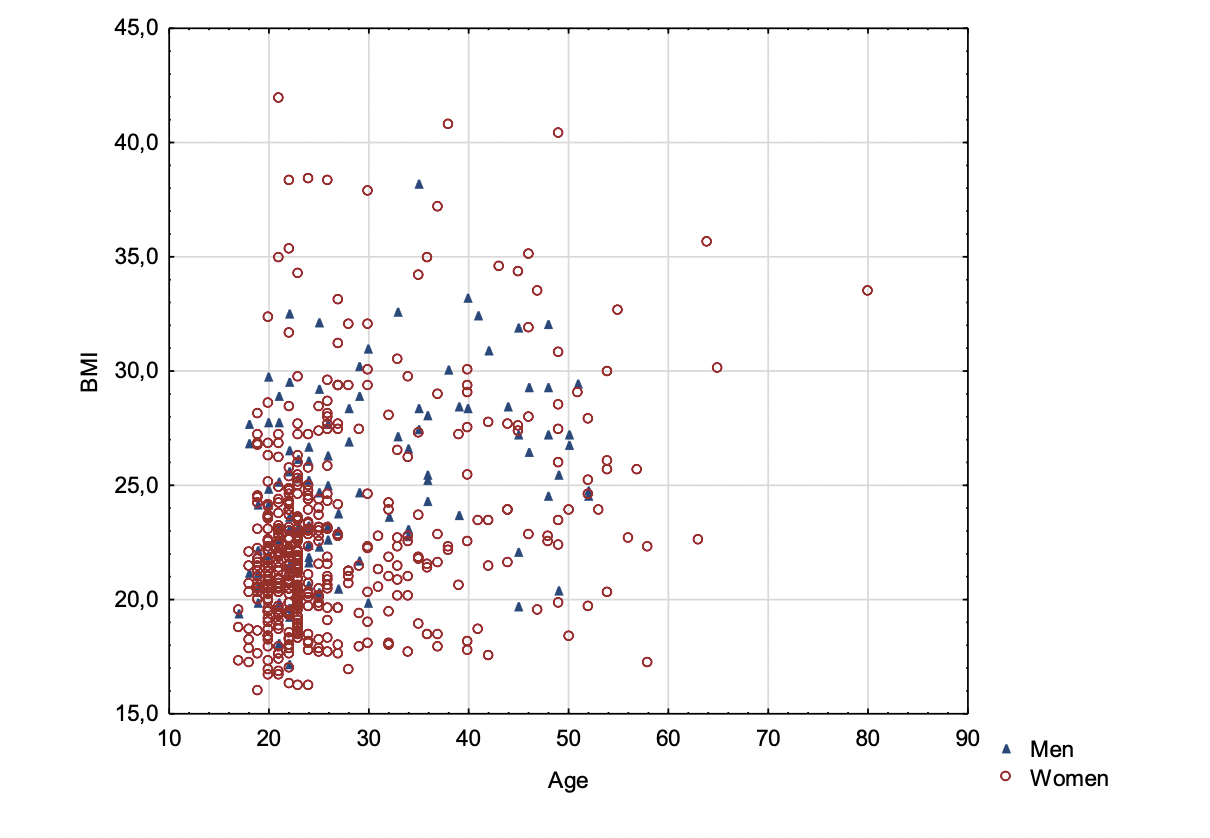
580 people aged 18 to 80 participated in our study. Most of them (65%) were from cities with > 100,000 inhabitants and declared an average financial status. As many as 81% of the respondents were women. Men were significantly older than women (mean age 30.0 ± 10.0 years vs. 27.1 ± 9.7 years, p < 0.05). Smoking cigarettes (traditional and electronic) was declared by 22% of the respondents. The respondents՚ BMI ranged from 16.0 to 40.0 kg/m2 . The classification of patients with different categories of BMI is presented in Figure 1. BMI was higher in men than in women: 25.3 ± 3.9 kg/m2 vs. 22.8 ± 4.3 kg/m2 (p < 0.05).
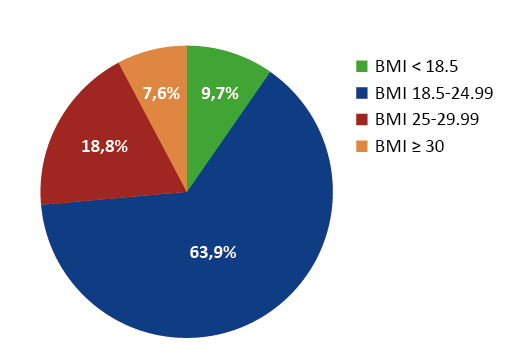
Figure 1. Categories of BMI in all respondents (n = 580)
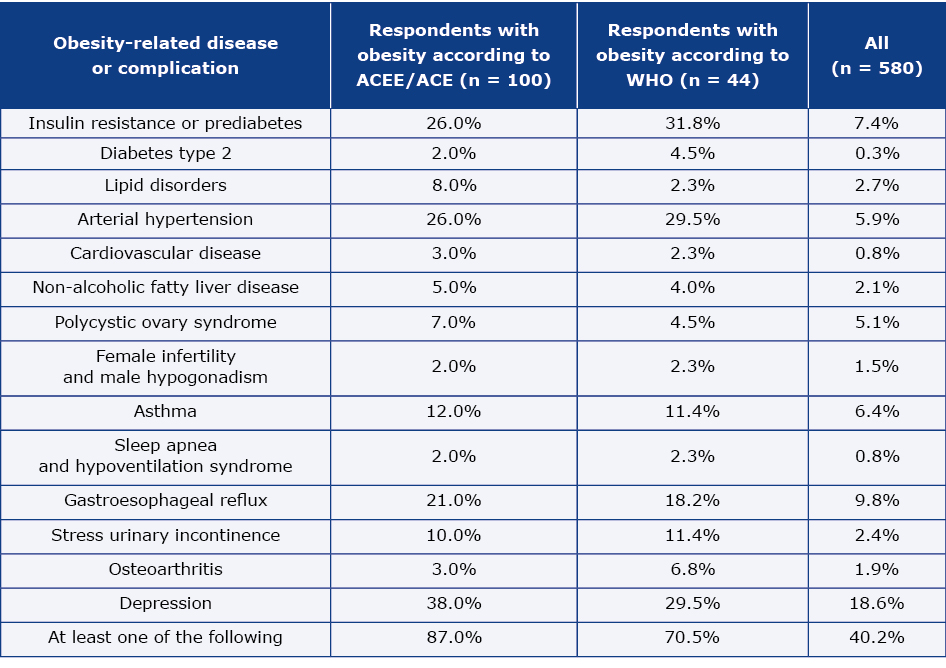
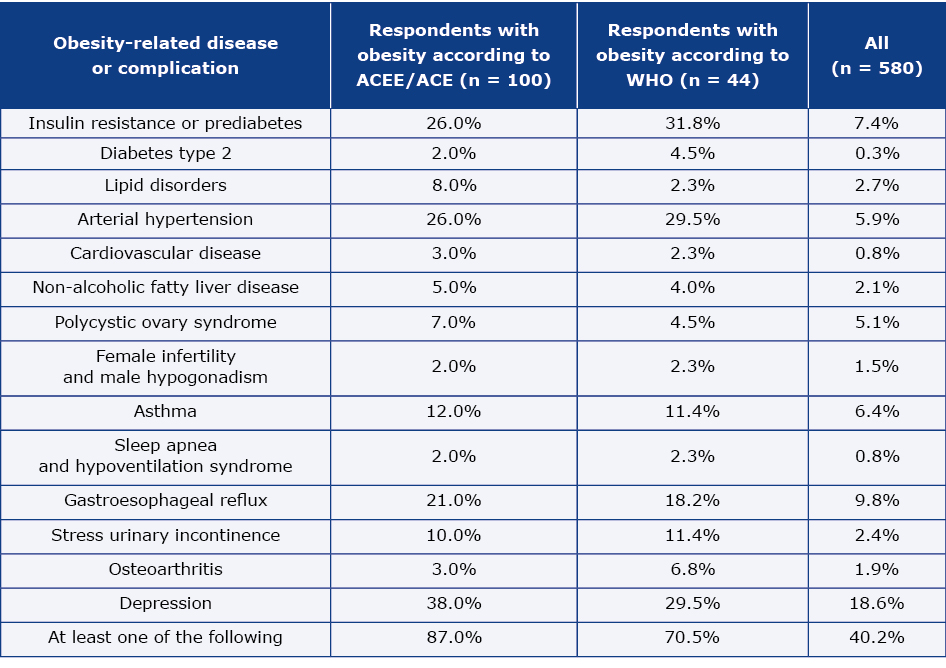
The prevalence of obesity in the studied population differed depending on which diagnostic criteria were used. As presented in Figure 1, according to the WHO criteria obesity was found in 7.6% of the respondents. However, according to ACEE/ACE criteria, its prevalence was more than twice as high (17.2%, p < 0.05). Taking into account the declared waist circumference, abdominal obesity was found in 25.2% of the respondents (Figure 2). The prevalence of obesity diagnosed according to ACEE/ACE criteria was higher in men than in women (data presented in Table 1). During the pandemic, as many as 43% of respondents experienced weight gain (6.2 ± 4.2 kg). The most common obesity-related disease or complications are presented in Table 2. The relationship between age and BMI among women and men and in the subgroup of respondents declaring a diagnosis of depression and without such a diagnosis is presented in Figures 3 and 4.
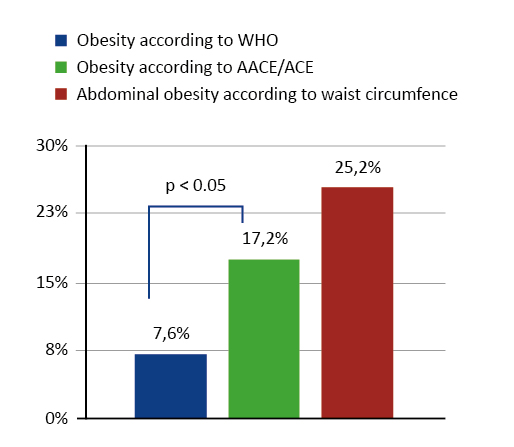
Figure 2. The prevalence of obesity diagnosed by different diagnostic criteria (n = 580)
Table 1. Prevalence of obesity according to different criteria in men and women

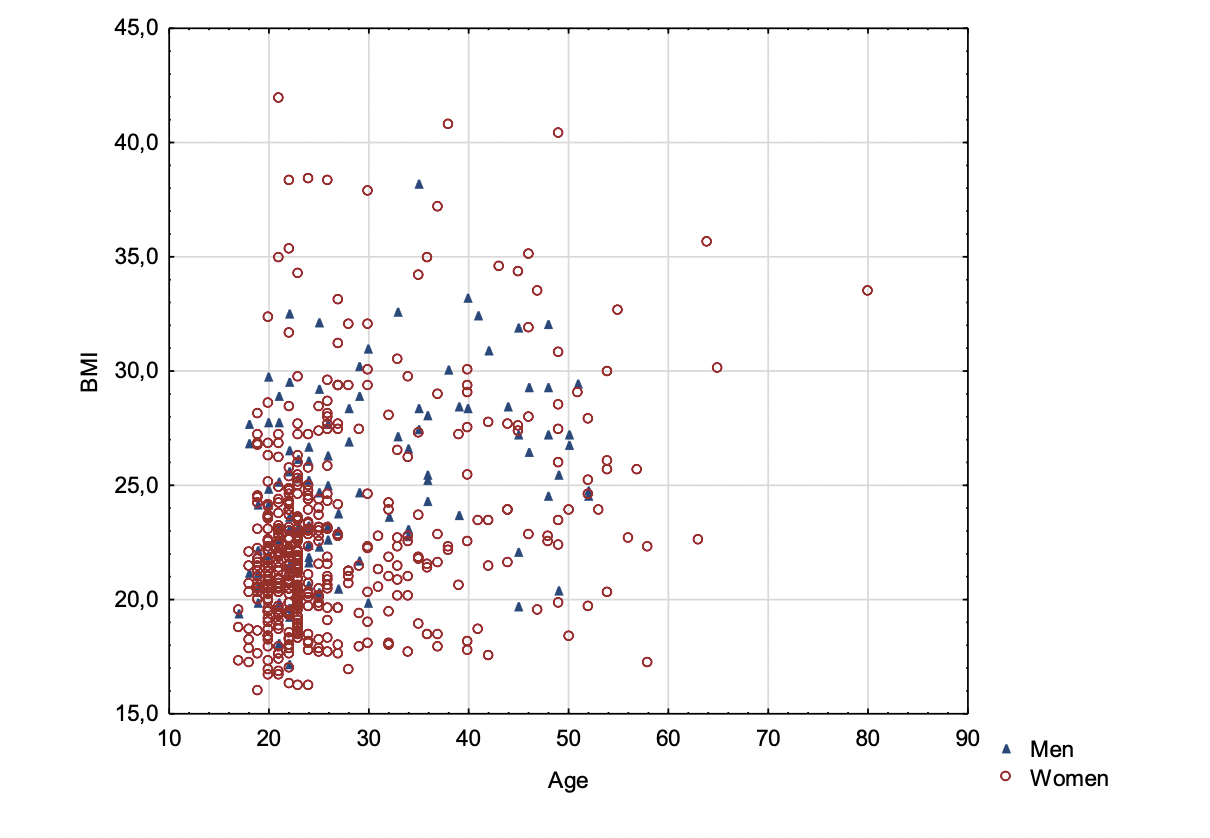
Figure 3. The relationship between age and BMI among women and men

Figure 4. The relationship between age and BMI in respondents declaring a diagnosis of depression and without such a diagnosis
Table 2. The prevalence of obesity-related disease or complication among respondents
Discussion
To our knowledge, this is the very first Polish research to diagnose obesity according to the ACEE/ACE guidelines and it was found that the prevalence according to the AACE/ACE criteria was more than twice as high as that diagnosed traditionally with WHO cut-off points for BMI. Such results may indicate the limitation of the only use of simple anthropometric measurements in such a complex diagnosis as obesity and the need to screen a patient with a BMI in the range of 25-29.9 for obesity-related complications. On the other hand, our study showed that waist circumference measurement must be included in the comprehensive patient assessment, particularly because the number of people with excess weight is seriously increasing. As many as 43% of our respondents declared that they gained an average of 6 kg over the last two years. This is similar to the data obtained in the Ipsos Covid 365+ study in a representative sample of 1,004 people [2, 8, 10]. Our results are also in line with the data from the WOBASZ study for the youngest group (20- -34.9 years) [19].
The selection of the group for our pilot study was dictated by the epidemiological situation. Nevertheless, the PTBO guidelines developed during the pandemic strongly recommended the use of telemedicine techniques to reach as many patients at risk as possible. Completing an online survey could raise health awareness in people who have never had direct contact with health services [2]. Telemedicine has been crucial during the pandemic and continues to be increasingly popular due to its convenience. Our results indirectly indicate that telemedicine can be helpful in the selection of young people at high risk of developing chronic diseases. On the other hand, through social media, health education adapted to young can and should be conducted. Experts also emphasize the importance of cooperation with a dietitian in the prevention of obesity complications. Unfortunately, lack of reimbursement for such services makes such cooperation impossible within the current the Polish healthcare system. On the other hand, the frequent coexistence of excess weight with psychological consequences indicates the need to extend the therapeutic team to mental health specialists. Obesity is associated with a wide range of mental effects, including depressed mood, low self-esteem, impaired body imagine, stress, eating disorders and poor quality of life. Comprehensive treatment, in addition to dietary recommendations and exercise, should include cognitive behavioral therapy with lifestyle interventions [7, 20]. The development of telemedicine may eliminate at least some of the barriers in access to specialists [21-22].
Our results may confirm a link between depression and being overweight described by others [7, 20]. This is a very worrying phenomenon because the majority of people suffering from depression are young [23]. The reasons for this are complex and it cannot be ruled out that broad access to new technologies plays a role here [20, 24]. The limitation of our pilot study was the small group of respondents and the lack of direct contact with the subjects. For these reasons, our results may be underestimated. The overrepresentation of women in the study group is another limitation of our work. The form of online contact with study participants made it impossible for us to measure the respondents’ weight, height and waist circumference or to perform the oral glucose tolerance test and analyze its results. Therefore, we asked also about the diagnosis of insulin resistance, as this term is more understandable for internet respondents. Taking into account that type 2 diabetes and prediabetes are underdiagnosed, this difference may not be significant. Studies on a larger representative sample are needed to confirm the results of our small pilot study.
Conclusions
The results of our study may indicate the problem of underestimating the risk of complications in young people with a BMI in the range of 25-29.9. Diagnosing obesity according to the ACEE/ACE guidelines may enable earlier diagnosis and thus earlier treatment of obesity.
Funding
None.
Conflicts of interest
There is no conflict of interest in this project.
References
| 1. |
Obesity: preventing and managing the global epidemic: report of a WHO Consultation on Obesity, Geneva, 3-5 June 1997 [Internet]. Geneva: World Health Organization; Available from: https://apps.who.int/iris/handle/10665/63854.
|
| 2. |
Olszanecka-Glinianowicz M, Dudek D, Filipiak K, Krzystanek M, Markuszewski L, Ruchała M, et al. Treatment of overweight and obesity during and after a pandemic. Let’s not wait for the development of complications – new guidelines for doctors. Arter Hypertens [Internet]. 2020;24(3):93-105. Available from: https://doi.org/10.5603/AH.a2020.0019.
|
| 3. |
Yang J, Tian C, Chen Y, Zhu C, Chi H, Li J. Obesity aggravates COVID-19: An updated systematic review and meta-analysis. J Med Virol [Internet]. 2021 May;93(5):2662-74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33200825.
|
| 4. |
Zheng KI, Gao F, Wang X-B, Sun Q-F, Pan K-H, Wang T-Y, et al. Letter to the Editor: Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism [Internet]. 2020 Jul;108:154244. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32320741.
|
| 5. |
Moriconi D, Masi S, Rebelos E, Virdis A, Manca ML, De Marco S, et al. Obesity prolongs the hospital stay in patients affected by COVID-19, and may impact on SARS-COV-2 shedding. Obes Res Clin Pract [Internet]. 2020;14(3):205-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32534848.
|
| 6. |
Stefan N, Birkenfeld AL, Schulze MB, Ludwig DS. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol [Internet]. 2020 Jul;16(7):341-2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32327737.
|
| 7. |
Chu D-T, Minh Nguyet NT, Nga VT, Thai Lien NV, Vo DD, Lien N, et al. An update on obesity: Mental consequences and psychological interventions. Diabetes Metab Syndr Clin Res Rev [Internet]. 2019;13(1):155-60. Available from: https://www.sciencedirect.com/science/article/pii/S1871402118302820.
|
| 8. |
Bąk‐Sosnowska M, Białkowska M, Bogdański P, Chomiuk T, Gałązka‐Sobotka M, Holecki M, et al. Zalecenia kliniczne dotyczące postępowania u chorych na otyłość 2022 – stanowisko Polskiego Towarzystwa Leczenia Otyłości [in Polish] [Internet]. Medycyna Praktyczna wydanie specjalne. 2022 [cited 2022 Nov 10]. p. 1-87. Available from: https://www.mp.pl/nadwaga-i-otylosc/wytyczne/303522,zalecenia-kliniczne-dotyczace-postepowania-u-chorych-na-otylosc-2022.
|
| 9. |
Dobrowolski H, Włodarek D. Body Mass, Physical Activity and Eating Habits Changes during the First COVID-19 Pandemic Lockdown in Poland. Vol. 18, International Journal of Environmental Research and Public Health. 2021.
|
| 10. |
Covid 365+. Wyniki badania po roku pandemii [in Polish] [Internet]. IPSOS. 2021 [cited 2022 Nov 10]. Available from: https://www.ipsos.com/pl-pl/covid-365-wyniki-badania-po-roku-pandemii.
|
| 11. |
Safaei M, Sundararajan EA, Driss M, Boulila W, Shapi’i A. A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput Biol Med [Internet]. 2021;136:104754. Available from: https://www.sciencedirect.com/science/article/pii/S0010482521005485.
|
| 12. |
Müller MJ, Braun W, Enderle J, Bosy-Westphal A. Beyond BMI: Conceptual Issues Related to Overweight and Obese Patients. Obes Facts [Internet]. 2016;9(3):193-205. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27286962.
|
| 13. |
Yang D, Beauvais A, Forbes WL, Beckman D, Estes J, Martinez C, et al. Relationship Between Body Mass Index and Diagnosis of Obesity in the Military Health System Active Duty Population. Mil Med [Internet]. 2022 Jul 1;187(7-8):e948-54. Available from: https://doi.org/10.1093/milmed/usab292.
|
| 14. |
Clerc PG, Mayer SB, Graybill S. Overweight BMI (25–29) in Active Duty Military: Excess Fat or More Lean Mass? A Look at the Evidence. Mil Med [Internet]. 2022 Jul 1;187(7-8):201-3. Available from: https://doi.org/10.1093/milmed/usab447.
|
| 15. |
González-Salazar LE, Serralde-Zúñiga AE, Flores-López A, Díaz-Sánchez JP, Medina-Vera I, Pichardo-Ontiveros E, et al. Prevalence of adiposity-based chronic disease and its association with anthropometric and clinical indices: a cross-sectional study. Br J Nutr [Internet]. 2022/09/22. 2022;1-10. Available from: https://www.cambridge.org/core/article/prevalence-of-adipositybased-chronic-disease-and-its-association-with-anthropometric-and-clinical-indices-a-crosssectional-study/C178748896E4FED4448CE75CD8524FC1.
|
| 16. |
Odsetek osób w wieku powyżej 15 lat według indeksu masy ciała (BMI) [in Polish] [Internet]. Główny Urząd Statystyczny. 2020 [cited 2022 Nov 10]. Available from: https://stat.gov.pl/obszary-tematyczne/zdrowie/zdrowie/odsetek-osob-w-wieku-powyzej-15-lat-wedlug-indeksu-masy-ciala-bmi,23,1.html.
|
| 17. |
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines For Medical Care of Patients with Obesity. Endocr Pract [Internet]. 2016;22:1-203. Available from: https://www.sciencedirect.com/science/article/pii/S1530891X20446300.
|
| 18. |
The IDF consensus worldwide definition of the metabolic syndrome [Internet]. Brussels: International Diabetes Federation; 2006. Available from: https://www.idf.org/component/attachments/attachments.html?id=705&task=download.
|
| 19. |
Stepaniak U, Micek A, Waśkiewicz A, Bielecki W, Drygas W, Janion M, et al. Prevalence of general and abdominal obesity and overweight among adults in Poland. Results of the WOBASZ II study (2013–2014) and comparison with the WOBASZ study (2003-2005). Polish Arch Intern Med [Internet]. 2016 Aug 18; Available from: http://pamw.pl/en/node/3499.
|
| 20. |
Swainson J, Reeson M, Malik U, Stefanuk I, Cummins M, Sivapalan S. Diet and depression: A systematic review of whole dietary interventions as treatment in patients with depression. J Affect Disord [Internet]. 2023;327:270-8. Available from: https://www.sciencedirect.com/science/article/pii/S016503272300112X.
|
| 21. |
Sculley JA, Musick H, Krishnan JA. Telehealth in chronic obstructive pulmonary disease: before, during, and after the coronavirus disease 2019 pandemic. Curr Opin Pulm Med [Internet]. 2022 Mar 1;28(2):93–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/34860202.
|
| 22. |
Major Depression [Internet]. National Institute of Mental Health. 2022 [cited 2022 Nov 10]. Available from: https://www.nimh.nih.gov/health/statistics/major-depression.
|
| 23. |
Alamoudi D, Breeze E, Crawley E, Nabney I. The Feasibility of Using Smartphone Sensors to Track Insomnia, Depression, and Anxiety in Adults and Young Adults: Narrative Review. JMIR mHealth uHealth [Internet]. 2023 Feb 17;11:e44123. Available from: http://www.ncbi.nlm.nih.gov/pubmed/36800211.
|