Analysis of diabetes-related complications and the cost of diabetes in Poland. The methodology and the research sample used in Economedica DM-PL Survey
Abstract
Background: Knowledge about diabetes mellitus (DM)-related complications, the direct and indirect costs incurred by patients with DM is still insufficient in Poland. Economedica DM-PL (Economedica) survey was a cross-sectional observational study that aimed to assess these issues.
Material and methods: The survey was carried out in 2016 on a representative sample of 2032 diabetic patients recruited by 195 general practitioners (GP) and 48 diabetologists (D) randomly selected from the national registry of physicians. Each GP and D recruited 8 to 10 patients with DM according to the specified protocol. The study included 1938 medical questionnaires (completed by the GPs and Ds), 1938 questionnaires about costs (completed by the patients) and 1532 treatment adherence questionnaires.
Results: The Economedica survey provided new insights into DM epidemiological and cost data. 70% of patients with type-1 DM were diagnosed with the disease before the age of 40. For 76% patients with type-2 DM, it was diagnosed after the age of 50. The average monthly out-of-pocket medical costs for DM patients in 2016 reached 66.2 EUR, while their non-medical costs were 36.8 EUR.
Conclusions: The methodology applied in our study proved useful for providing new dimensions of DM epidemiological and cost data in Poland.
Citation
Bogusławski S, Wojciechowska A, Smaga A, Strojek K, Wróbel K, Wojtyniak B, Juszczyk G, Czech M, Zdrojewski T. Analysis of diabetes-related complications and the cost of diabetes in Poland. The methodology and the research sample used in Economedica DM-PL Survey. Eur J Transl Clin Med. 2023;6(1):31-40Abbreviations
CATI – computer assisted telephone interview
D – diabetologist
DM – diabetes mellitus
FFS – fee for service
GP – general practitioner
HDM – Health Data Management Ltd.
NFZ – Narodowy Fundusz Zdrowia (National Health Fund)
NIZP-PZH – Narodowy Instytut Zdrowia Publicznego –
Państwowy Zakład Higieny – Państwowy Instytut Badawczy
(National Institute of Public Health – National Institute of
Hygiene – National Research Institute)
PESEL – Powszechny Elektroniczny System Ewidencji Ludności (national ID number)
Introduction
The World Health Organisation forecasts a steady increase in the rates of obesity and diabetes mellitus (DM) [1]. It is estimated that, globally, the number of people suffering from DM will increase from 382 million in 2013 to 592 million in 2035 [2]. In 2004 the number of patients with DM in Poland was projected to reach 2.5 million by 2030 [3], but according to the available data, this number was already at 2.68 million in 2014 [4], with DM affecting 8.4% of the general adult population, similarly to the rate observed in other European populations [5]. Clinical data shows that DM, if incorrectly treated, leads to severe complications affecting most bodily organs. Therefore, DM in middle and high income countries constitutes a heavy burden on the finances of public and private payers. At the same time, the course of DM can be positively modified by early diagnosis and through the adoption of appropriate drug therapies and changes in lifestyle.
The existing data on the costs of DM in Poland, which are based on the diagnoses and the services provided to patients by National Health Fund (Narodowy Fundusz Zdrowia – NFZ), the only public payer, is incomplete [4]. The incomplete data results from widespread upcoding in the system of reported diagnoses and linking the services to diagnoses that are most cost-intensive, as well as from the gaps in the data reported by general practitioners (GPs). At the same time, the data obtained from the rapidly growing non-public sector (buying services on a fee for service basis, FFS) and through subscription and insurance companies) is quite fragmented. As a result, the number of DM patients who receive care and treatment in this manner is unknown.
The Economedica study was designed to obtain objective data from a representative sample of DM patients treated by GPs and diabetologists (Ds) in Poland about the prevalence of DM complications and various types of DM-related costs with a relatively simple and easily reproducible methodology. The goals of the Economedica survey were to evaluate:
- the prevalence of the main DM related complications in a representative sample of adult patients with DM;
- the direct medical and non-medical costs incurred by patients with DM;
- the indirect costs of treatment of DM and its complications;
- the level of adherence to treatment among patients with DM.
The aim of this paper was to describe the methodology and some results of the Economedica study.
Material and methods
Random sampling of general practitioners and diabetologists
The survey was designed as an observational study on a representative sample of DM patients treated by randomly selected GPs and Ds in Poland. The sample of GPs and Ds was drawn from the database of Health Data Management (HDM), a continuously updated address list of practicing physicians in Poland. We planned sample sizes of 200 GPs and 50 Ds working in outpatient clinics. According to the HDM data, at the time of the study there were 20944 practicing GPs and 955 practicing Ds in Poland [6]. The following quoting mechanism was proposed. In the case of the GP sample, geographical strata were created on the basis of Poland’s 16 provinces (województwa) and three types of locations: village/town with a population < 20000; town/city with a population between 20001 and 100000; and city with a population > 100000. For the D sample, two location categories were adopted: < 100000 and > 100000 population. In case of refusals, the remaining physicians were recruited using quota sampling. Ultimately, 243 physicians took part in the study: 195 GPs and 48 Ds.
Random sampling of patients with DM
Each participating GP recruited 8 patients with DM (including one patient with type-1 DM) to the study, completed medical questionnaires about them and asked patients to complete cost questionnaires. Each D recruited 10 patients (including 6 with type-1 DM). The inclusion criteria were: patient > 18 years with a prescription for at least one hypoglycemic medication during the visit. Among those patients who met the inclusion criteria, the GPs qualified the first patient with type-1 DM and every third patient with type-2 DM, while the Ds qualified every second patient with type-1 DM and every third patient with type-2 DM. Additionally, the GPs and Ds prepared a register of all the patients they consulted over a period of two weeks, including their age, sex and diagnosis. The diagnosis of type-1 or 2 DM was based on the patients’ medical records. The study was carried out between March and July 2016.
Study design
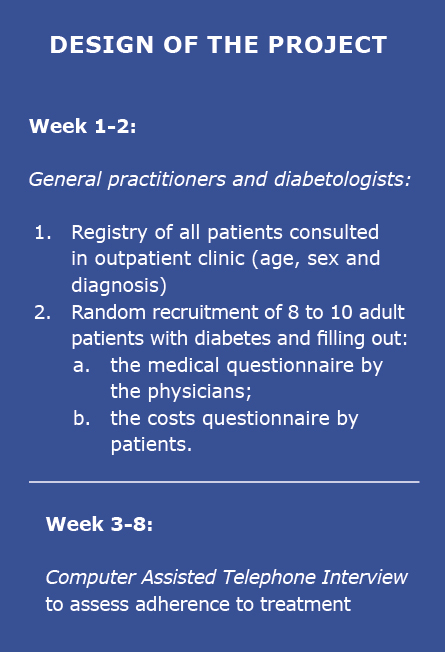
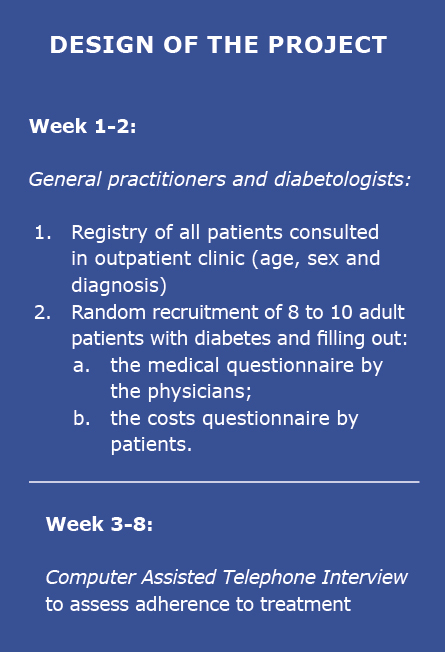
Figure 1. Design of the Economedica DM-Pl Survey
The Economedica survey involved:
- registration of all patients (including data about the age, sex, diagnosis) consulted by the GPs and Ds in their clinical practice;
- random recruitment (in the order described above) of patients with DM during routine visits: 8 in the case of the GP’s and 10 in the case of Ds. For all the recruited patients, the physicians completed a medical questionnaire, whereas the patients completed questionnaires about costs [including medical and non-medical costs incurred by the patients as well as indirect costs of DM, e.g. absenteeism (absence from work) and presenteeism (working while sick, resulting in reduced work effectiveness)] [7-8];
- a computer assisted telephone interview (CATI) carried out during the subsequent 6 weeks (weeks 3 to 8), to assess whether the patients adhered to the treatment they were prescribed after their consultation with the GP or D.
The medical questionnaire completed by the physicians included the following information:
- age, sex, type of DM and its treatment, BMI, blood pressure;
- presence of confirmed DM-related complications, e.g. ischemic heart disease, chronic heart failure, stroke, peripheral vascular disease, diabetic foot syndrome, amputation associated with peripheral vascular disease/diabetic foot syndrome, diabetic nephrectomy, kidney transplant, diabetic retinopathy, diabetic maculopathy, secondary glaucoma, diabetic neuropathy and depression/depression treatment;
- occurrence of hypoglycemic episodes and a description of the episodes;
- presence of risk factors: hypercholesterolemia, hypertriglyceridemia, arterial hypertension, tobacco smoking, lack of physical activity, a diet high in saturated fats;
- last HbA1c and lipid profile laboratory results.
The costs questionnaire, which was completed anonymously by the patients during their visit with the GP or D included the following information:
- the medical costs of DM and/or its complication incurred in the last 4 weeks;
- the non-medical costs of DM and/or its complication incurred in the last 4 weeks (e.g. food, cosmetics, transport, care, etc.);
- the level of income lost by the patient’s family members in connection with DM patient care and its complications;
- absenteeism or presenteeism due to DM and/or its complications, the use of medical services (visits to specialists in the last 4 weeks) and/or hospital treatment;
- data concerning the glycaemia measurement methods used by the patient (based on the patient’s declaration);
- education and per capita household income.
The Computer-Assisted Telephone Interviews were carried out with patients on average 30 days after the visit to the physician (between weeks 3 and 8 of the study) and focused on the results of glycaemia measurements, the details of the use of antidiabetic drugs in relation to the physician’s instructions and the reasons for potential non-adherence, as well as the occurrence of hypoglycemic episodes. All the questionnaires and the CATI data were coded with unique, anonymous identifiers, which allowed the data from different sources to be linked.
The characteristics of the random sample of patients with DM in the study
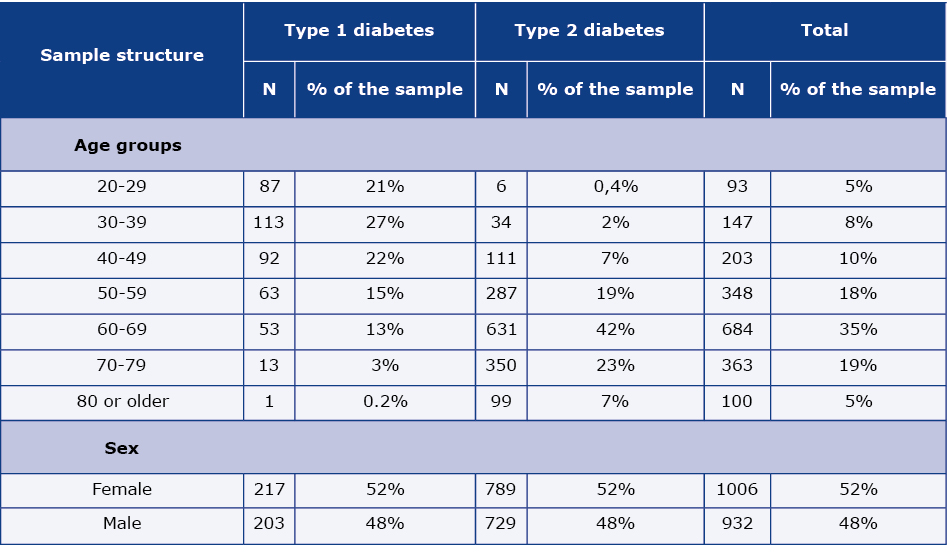
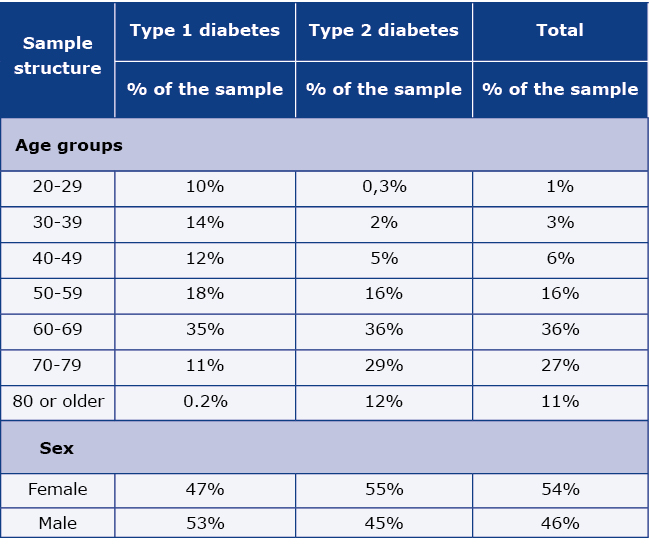
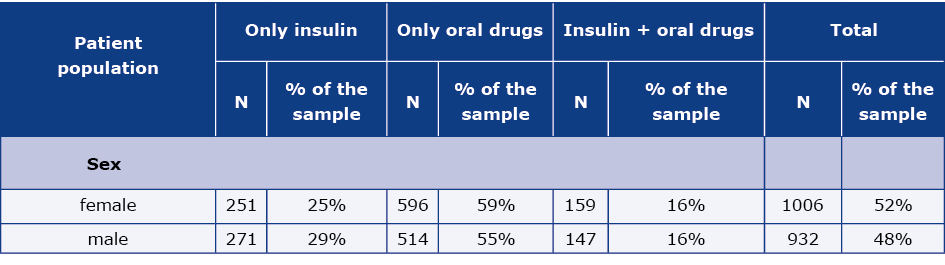
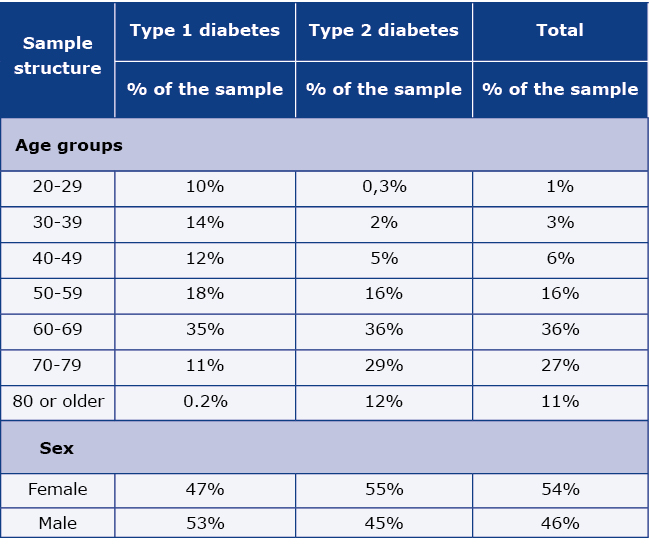
A random-quota sampling was used to obtain at least 60 patients with type1 DM described by the GPs for each of the three types of locations and at least 120 patients with type-1 DM described by the Ds for each of the two types of locations. In total, a sample of 2032 patients with DM was obtained, 96.8% of the planned sample size. A complete set of data (the medical questionnaire completed by the physician and the costs questionnaire completed by the patient) was obtained for 1938 DM patients and it was put into the survey datafile for further analysis. The age and gender structure of survey participants is shown in Table 1: females accounted for 52% and males for 48% of the sample. 1532 patients with DM agreed to take part in the CATI. Projected data is shown in Table 1a.
Table 1. Age and gender structure of the DM patients’ sample (raw data)
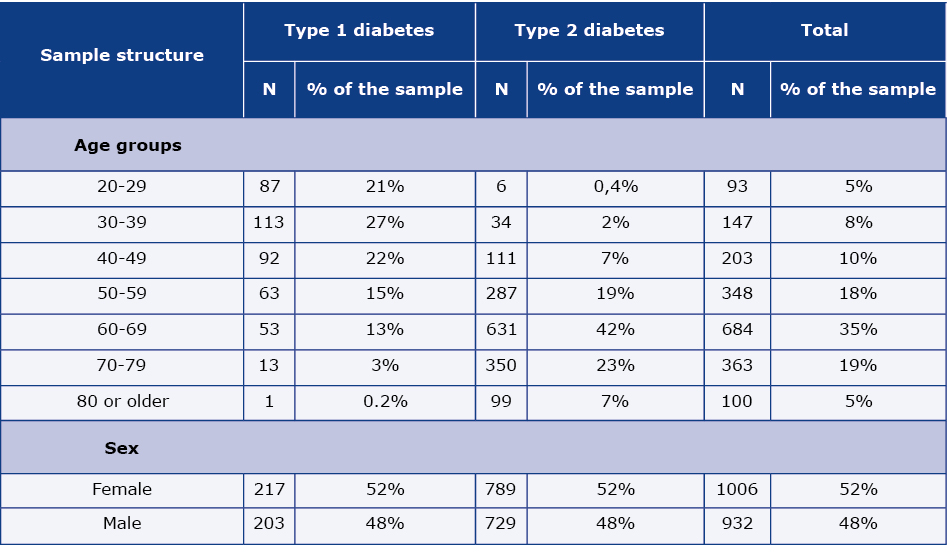
N – number of individual patients
Table 1a. Age and gender structure of the DM patients’ population after projection (weighted data)
Data analysis
In order to estimate the prevalence of selected conditions in the general DM patient population, multi-dimensional data weighting was carried out on the sample. The following factors were taken into account in designing the weights:
- data on the number of physicians – weights were used to adjust the proportion between the number of GPs and Ds, on the basis of HDM data on the general population of physicians in Poland [6];
- data on the average number of all patients seen daily, weekly and monthly by the GP or D based on a two-week detailed register compiled by the physicians during the study;
- data on the physicians’ average number of working days in a month, adjusted for days taken off from work and holidays (based on two-weeks of detailed registers) [7-8];
- data on the frequency of patients’ visits to the GPs or Ds based on average intervals between visits.
Weights used in the Economedica survey were obtained using:
- Data from NFZ for the randomly selected sample of DM patients in Poland within each of the 16 provinces. 384000 patients, who were > 18 years of age in 2017, were randomly selected from a database of 37.97 million PESEL numbers (Polish national ID numbers – Powszechny Elektroniczny System Ewidencji Ludności). For the 384,000 PESEL numbers, the NFZ obtained information about all the medical procedures and products (e.g. drugs, medical devices, nutritional products) financed by the NFZ. The anonymised data was forwarded to the National Institute of Public Health (NIZP – Narodowy Instytut Zdrowia Publicznego), which conducted the analysis.
- NFZ datafile on the volume of drugs reimbursed in pharmacies on the basis of prescriptions [9].
- NFZ data on the structure of the DM patient population according to age, gender and type of DM [4].
- Data on the number of packs of drugs used in the treatment of DM, prescribed by GPs and Ds in Poland in 2016, which was obtained from PEX PharmaSequence’s RECEPTOmetr service. RECEPTOmetr is a commercially available, on-going database service for monitoring medical prescriptions, which used a monthly random survey among approximately 10 million medical prescriptions. In 2016 the data was collected from a sample of 4300 pharmacies, out of an estimated total of 14500 pharmacies in Poland, proportionally distributed across 16 provinces and types of locations. The patient age structure in the RECEPTOmetr database is in line [+/- 0.8%] with the data reported by the NFZ. The age structure of patients with type-2 DM was adjusted based on the PEX PharmaSequence’s RECEPTOmetr prescription data.
Results
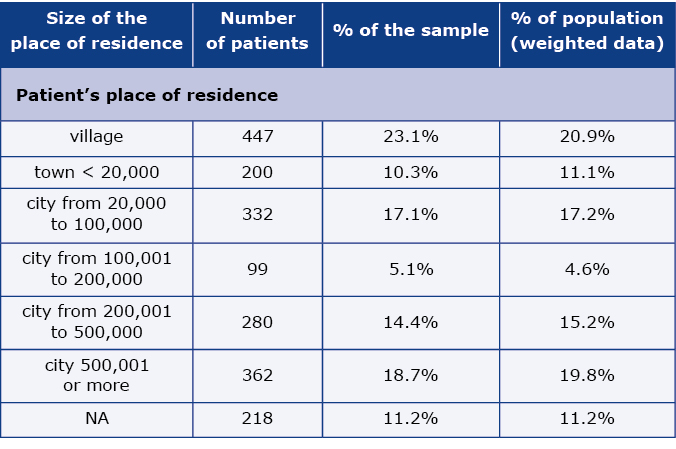
The weighted structure of the population of DM patients’ according to the place of residence is shown in Table 2. While every 3rd patient lived in a location where the population was < 20000, every 5th was a resident of the largest cities in Poland. Regardless of their place of residence, we observed that the patients included in the study more often visited physicians who work in large cities.
Table 2. DM patients’ population by the patient’s place of residence
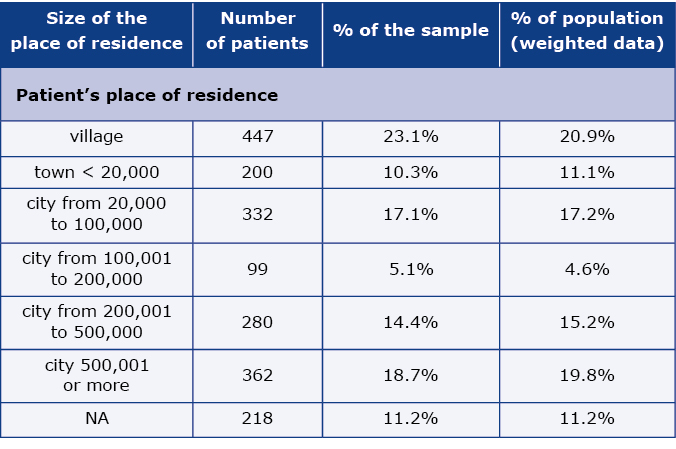
N – number of individual patients
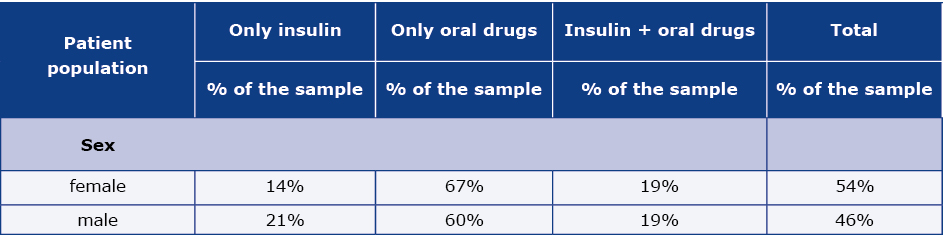
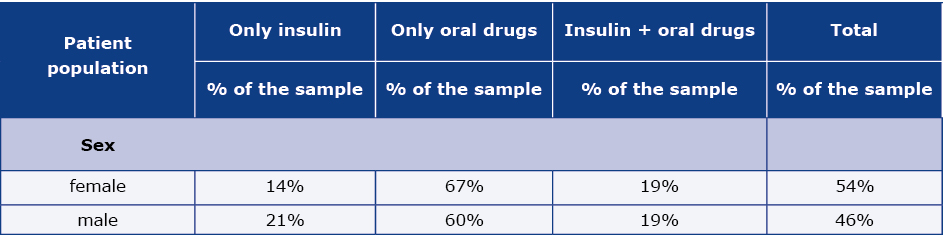
The distribution of the pharmacotherapy patterns of DM in the examined random sample of adults is presented in the Table 3, while weighted results are shown in the Table 3a. The projected data indicates that DM patients are predominantly treated only with oral drugs (67% of females and 60% of males). 19% of the female patients in the study and the same proportion of males were treated with a combination of oral drugs and insulin, while the remaining patients (14% of females and 21% of males) were treated only with insulin.
Table 3. DM patients’ sample structure according to the way of DM treatment (raw data)
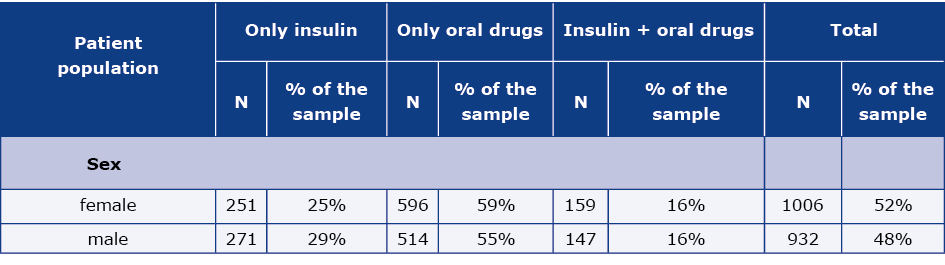
N – number of individual patients
Table 3a. DM patients sample structure according to the way of DM treatment (weighted data)
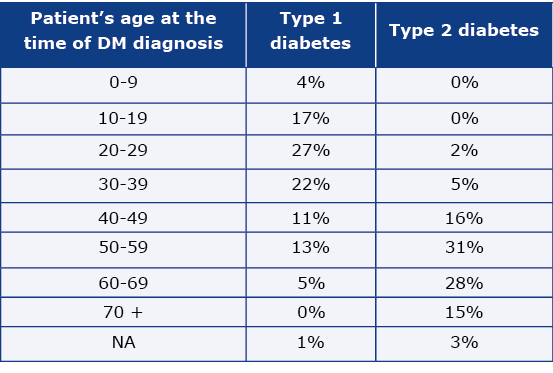
Weighted results show that the group of patients with type-1 DM is dominated by those whose disease started before the age of 40 (70%). In contrast, the group of patients with type-2 DM, the majority (76%) are patients whose DM was diagnosed after the age of 50 (Table 4).
Table 4. Distribution of DM patients according to the type of DM and patient’s age at the time of DM diagnosis
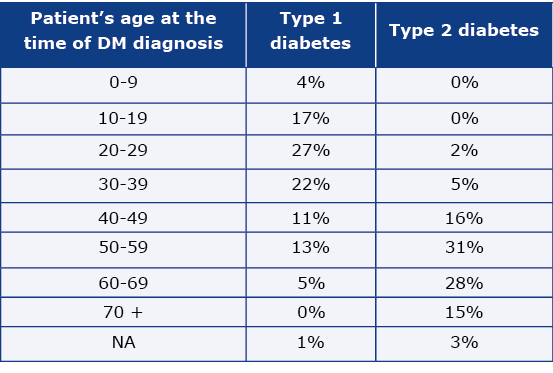
NA – data non available
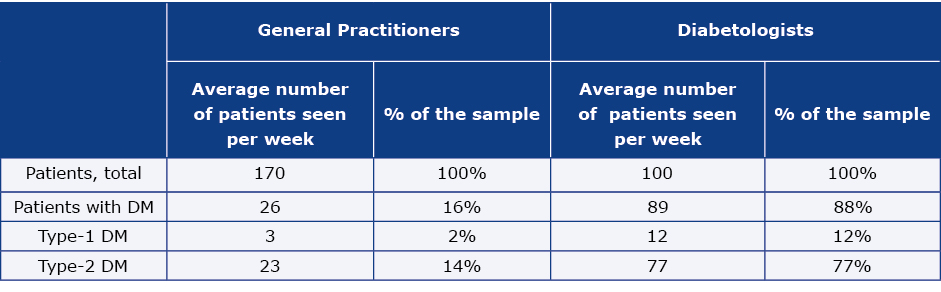
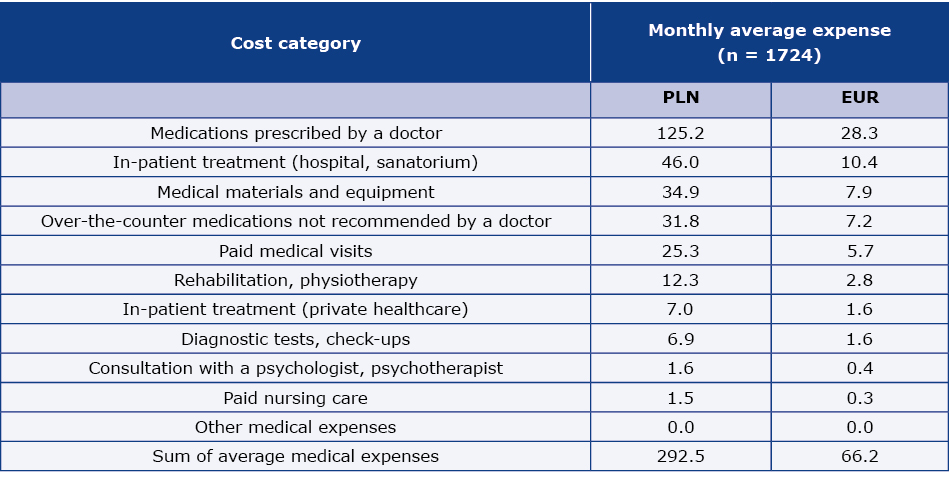
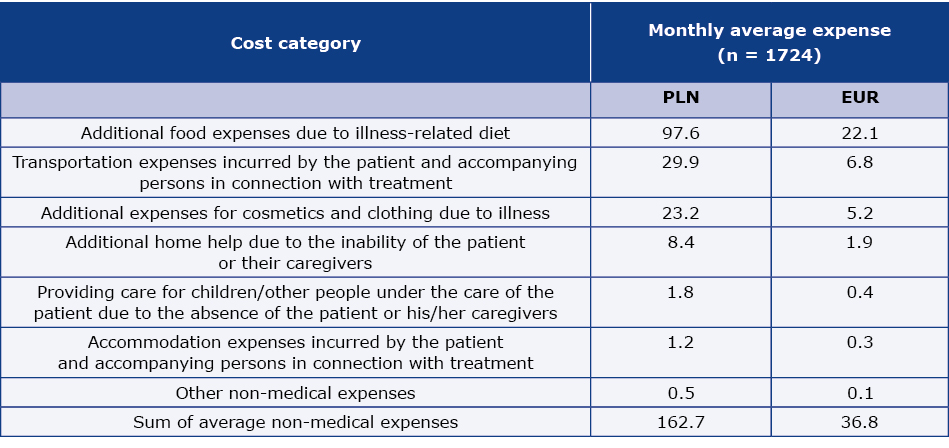
On the basis of the physicians’ registers of patient visit over a period of two weeks, we estimated that patients with DM accounted for 16% of all the patients seen by GPs and 88% of all the patients seen by Ds (Table 5). In the whole examined sample, 87.5% were patients with type-2 DM. The average (per patient) monthly medical costs directly incurred by patients related to DM and/or DM-related complications reached 292.5 PLN (66.2 EUR) (Table 6, weighted data). The costs of the medications prescribed by doctors reached 42.8% of the patients’ total medical expenses. The average (per patient) monthly non-medical costs directly incurred by patients and that were related to DM and/or DM related complications reached 162.7 PLN (36.8 EUR) (Table 7, weighted data). These costs were dominated by additional food expenses due to illness-related diet, which amounted to 60% of the patients’ non-medical costs.
Table 5. Average number of patients admitted by the physician per week, including the percentage of patients diagnosed with DM (raw data)
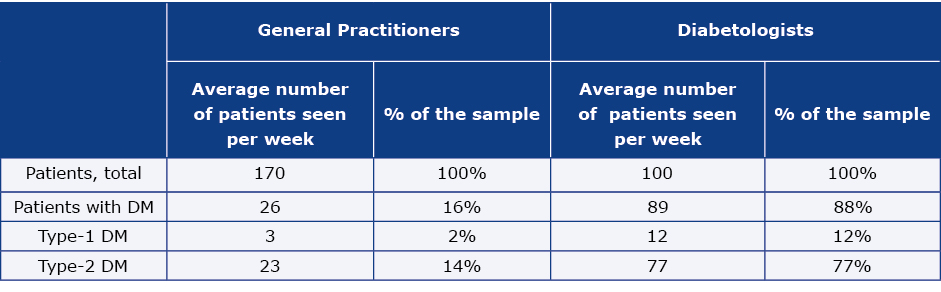
Table 6. Average monthly medical costs per patient – costs directly incurred by patients related to DM and/or DM related complications (weighted data) as declared by the patients
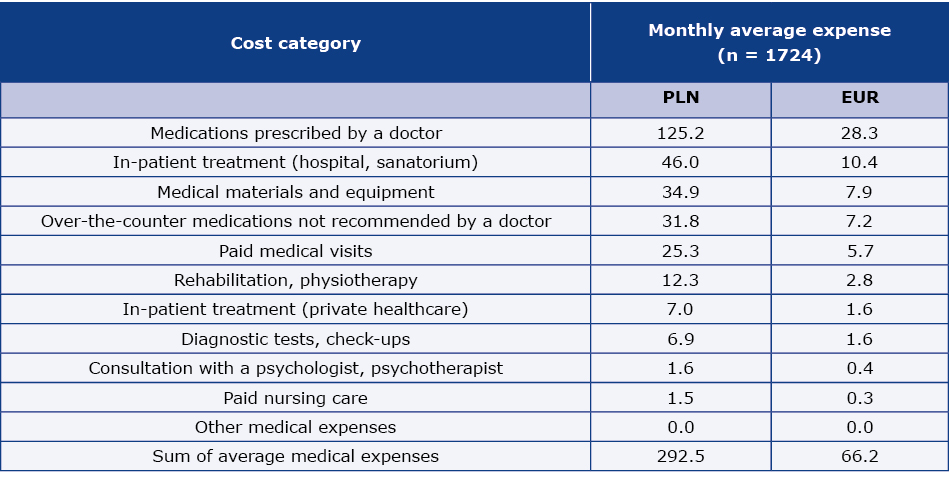
N – number of patients
Adopted euro exchange rate – 4.42 PLN (2016.12.30)
Table 7. Average monthly non-medical costs per patient (costs directly incurred by patients related to DM and/or DM related complications), as declared by the patients
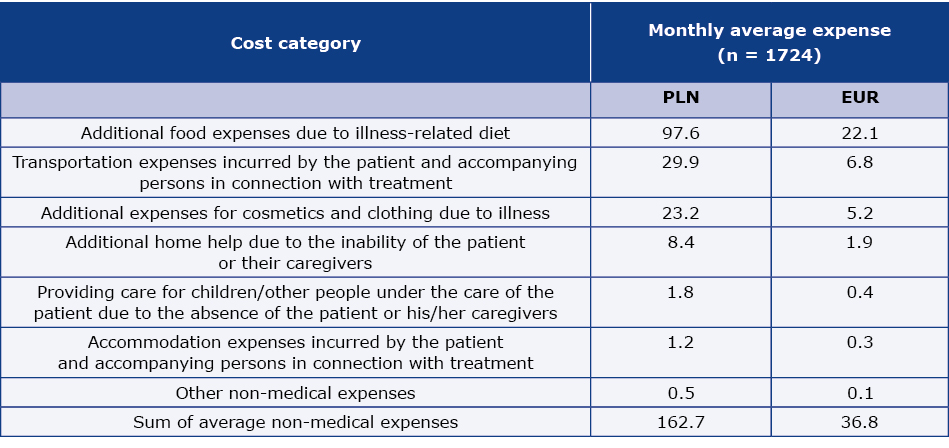
N – number of patients
Adopted euro exchange rate – 4.42 PLN (2016.12.30)
Discussion
The Economedica study was primarily designed to broaden the scope of current data related to the diagnosis and treatment of individuals suffering from DM in Poland. In many countries around the world, epidemiological data on morbidity and prevalence is neither complete nor systematically collected. This is the case also in Poland. Although several important studies have been carried out and many articles on the epidemiology of DM patients have been published in recent years, the epidemiological situation is still not well described. It is important to note the value of studies such as NATPOL and WOBASZ, which estimate the current incidence of DM in Poland at 6.7%-8.4% [5, 10-12]. Thanks to the fact that these studies were repeated regularly over 10 years, they provide a meaningful picture of the changes that have taken place over this time. Nonetheless, these epidemiological studies only create the foundations for knowledge about DM by describing the prevalence of the disease. There is still a lack of up-to-date data that reflects a broad range of epidemiological factors on DM complications, which can account for a significant cost both for public finances and for patients [13-14].
The study presented in this article aimed to provide the most detailed description of the selected sample of DM patients with attention to the differences between cases of type-1 and type-2 DM. Since DM-related complications occur at a different frequency in each of the two types of DM and the disease-related costs can also differ, we planned to test a sufficiently high number of patients with type-1 DM – 500 individuals, which constituted 24% of all the respondents in the study. It should be noted that this percentage does not correspond to the prevalence of type-1 DM among all DM patients. Nonetheless, it was already assumed at the planning stage of the study that we would adjust for the frequency of estimated complications in the two patient groups by referencing the most recent published epidemiological data.
Although the main goal of our study was to evaluate the prevalence of DM-related complications and to obtain data on the costs related to treatment of DM, the data collected in the study show that having applied the weights and adjustments described in the methodology, the age and gender structure of the patients participating in our survey does not significantly differ from the age and gender structure of the general DM patient population in Poland in 2013, as described by Topór-Mądry et al. [4]. The prevalence of DM increases with age and DM dominates older patient groups. This distribution coincides with observations from other European studies [15-16]. On the other hand, there are more females in the population of the study in Poland, which differs from the data presented by the International Diabetes Federation (IDF) where the prevalence of DM is higher among males [16]. This may result from the fact that only those who are aware of their disease were included in the study. Data in the IDF’s Diabetes Atlas presents estimates of DM prevalence. This data also takes into account the general lack of awareness about DM, which in Poland is greater among men [10-11].
It is important to emphasize that this study is not based on a random, representative sample of all patients suffering from DM in Poland. Instead, it should be treated as a description of the population of patients seeking medical advice concerning DM from GPs and Ds. In Poland diabetological care is predominantly the domain of these two medical specialists and the RECEPTOmetr data for 2017 shows that 84.1% of drugs packs from the A10 group were prescribed by GPs and Ds.
Additionally, observations from this study show that the percentage of DM patients’ visits to GPs is high in relation to morbidity. DM patients’ visits accounted for 16% of all visits to GPs. This clearly indicates a high workload for this group of physicians connected to managing DM patients. Determining what percentage of these patients have uncontrolled DM is an important task in terms of healthcare system management in Poland. Potential measures aimed at improving the control of DM may involve reducing the workload of GPs, especially that a general shortage of GPs is consistently observed throughout the country.
It is worth noting that DM creates a heavy financial burden on patients. The results of this study indicate that the average monthly out-of-pocket medical expenditures made by the patient reached almost 300 PLN (mainly for prescription drugs, which amount to 60% of the total medical costs). After adding the non-medical costs, the total amount was to close to 450 PLN monthly. The majority of the surveyed patients were over the age of 60, thus such costs can easily reduce their patients’ adherence to the treatment.
Conclusions
The diagnosis and treatment of DM causes a heavy burden on public finances, also in terms of social insurance [17-21]. These costs significantly increase when there is a dynamic increase in the number of newly diagnosed DM patients. Although financing the DM diagnostic process and treatment is an increasing challenge, particularly due to the limited public funds earmarked for public health in Poland, a detailed cost structure (including the costs associated with DM-related complications and the different courses of concomitant diseases) is yet to be thoroughly explored [22-23].
As in the case of many other countries, there is no register of patients with DM in Poland, therefore the Economedica study can be used as a model to monitor the most important epidemiological, therapeutic, and cost trends among patients affected by DM. We agree that further detailed analysis of the data from this survey, coupled with the data obtained from the NFZ by the NIZP, will enable an extended assessment of the prevalence of DM and its complications. It will also allow for the calculation of the additional burden on NFZ budget, which results from different courses of concomitant diseases in patients with DM as compared to patients not diagnosed with DM.
Acknowledgements
The study was carried out by Sequence Sp. z.o.o (now PEX PharmaSequence Sp. z o.o.) in co-operation with the National Institute of Public Health – National Institute of Hygiene and the DM Epidemiology Group from the Public Health Committee of the Polish Academy of Sciences. The study was financed by Sequence (now PEX PharmaSequence Sp. z o.o.)
Funding
None.
Conflicts of interest
There is no conflict of interest in this project.
References
| 1. |
Smolen JS, Burmester GR, Combeet B. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016; 387: 1513-30 – In this Article, Catherine Pelletier. 2016; Available from: https://doi.org/10.1016/S0140-6736(16)32060-8.
|
| 2. |
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract [Internet]. 2014;103(2):137-49. Available from: https://www.sciencedirect.com/science/article/pii/S0168822713003859.
|
| 3. |
Wild S, Roglic G, Green A, Sicree R, King H. Global Prevalence of Diabetes. Diabetes Care [Internet]. 2004;27(5):1047-53. Available from: https://doi.org/10.2337/diacare.27.5.1047.
|
| 4. |
Topor‐Madry R, Wojtyniak B, Strojek K, Rutkowski D, Bogusławski S, Ignaszewska‐Wyrzykowska A, et al. Prevalence of diabetes in Poland: a combined analysis of national databases. Diabet Med [Internet]. 2019;36(10):1209-16. Available from: https://doi.org/10.1111/dme.13949.
|
| 5. |
Rutkowski M, Wojciechowska A, Śmigielski W, Drygas W, Piwońska A, Pająk A, et al. Prevalence of diabetes and impaired fasting glucose in Poland in 2005-2014: results of the WOBASZ surveys. Diabet Med [Internet]. 2020;37(9):1528-35. Available from: https://doi.org/10.1111/dme.14333.
|
| 6. |
Baza lekarzy, placówek medycznych, aptek, farmaceutów [in Polish] [Internet]. Farma Prom. [cited 2023 Mar 10]. Available from: https://www.farmaprom.pl/pl/bazy-danych.
|
| 7. |
Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med [Internet]. 2003;45(2):156-74. Available from: http://www.jstor.org/stable/44997208.
|
| 8. |
Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, et al. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to Evaluate the Indirect Workplace Costs of Illness. J Occup Environ Med [Internet]. 2004;46(6):S23-37. Available from: http://www.jstor.org/stable/44996637.
|
| 9. |
Recepty i leki [in Polish] [Internet]. NFZ. [cited 2023 Mar 10]. Available from: https://www.nfz.gov.pl/dla-pacjenta/recepty-i-leki/.
|
| 10. |
Rutkowski M, Bandosz P, Czupryniak L, Gaciong Z, Solnica B, Jasiel-Wojculewicz H, et al. Prevalence of diabetes and impaired fasting glucose in Poland – the NATPOL 2011 Study. Diabet Med [Internet]. 2014;31(12):1568-71. Available from: https://doi.org/10.1111/dme.12542.
|
| 11. |
Zdrojewski T, Bandosz P, Szpakowski P i wsp. Rozpowszechnienie głównych czynników ryzyka chorób układu sercowo-naczyniowego w Polsce. Wyniki badania NATPOL PLUS [in Polish]. Kardiol Pol. 2004;61(supl 4):1-26.
|
| 12. |
Polakowska M, Piotrowski W. Incidence of diabetes in the Polish population: results of the Multicenter Polish Population Health Status Study – WOBASZ. Pol Arch Med Wewn [Internet]. 2011;121(5):156-63. Available from: http://europepmc.org/abstract/MED/21610663.
|
| 13. |
Ward A, Alvarez P, Vo L, Martin S. Direct medical costs of complications of diabetes in the United States: estimates for event-year and annual state costs (USD 2012). J Med Econ [Internet]. 2014;17(3):176-83. Available from: https://doi.org/10.3111/13696998.2014.882843.
|
| 14. |
Candrilli SD, Meyers JL, Boye K, Bae JP. Health care resource utilization and costs during episodes of care for type 2 diabetes mellitus-related comorbidities. J Diabetes Complications [Internet]. 2015;29(4):529-33. Available from: https://www.sciencedirect.com/science/article/pii/S1056872714004061.
|
| 15. |
Group TDS. Age- and Sex-Specific Prevalences of Diabetes and Impaired Glucose Regulation in 13 European Cohorts. Diabetes Care [Internet]. 2003;26(1):61-9. Available from: https://doi.org/10.2337/diacare.26.1.61.
|
| 16. |
IDF Diabetes Atlas [Internet]. 8th ed. International Diabetes Federation; 2017. Available from: https://diabetesatlas.org/upload/resources/previous/files/8/IDF_DA_8e-EN-final.pdf.
|
| 17. |
Moćko P, Kawalec P, Malinowski K. Analysis of Costs of Diabetes in Poland in 2012 and 2013. Zesz Nauk Ochr Zdrowia, Zdr Publiczne i Zarządzanie [Internet]. 2016;14(3). Available from: https://www.ceeol.com/search/article-detail?id=516015.
|
| 18. |
Kinalska I, Niewada M, Głogowski C, Krzyżanowska A, Gierczyński J, Łatek M, et al. Koszty cukrzycy typu 2 w Polsce (Badanie CODIP) [in Polish]. Diabetol Klin [Internet]. 2004;5(1):1-8. Available from: https://core.ac.uk/reader/268454340.
|
| 19. |
Kawalec P, Kielar M, Pilc A. Koszty leczenia cukrzycy typu 1 i 2 w Polsce [in Polish]. Diabetol Prakt [Internet]. 2006;7(5). Available from: https://ruj.uj.edu.pl/xmlui/handle/item/245353.
|
| 20. |
Kissimova-Skarbek K, Pach D, Płaczkiewicz E, Szurkowska M, Szybiński Z. Ocena ekonomicznego obciążenia cukrzycą społeczeństwa Polski. Pol Arch Med Wewnętrznej. 2001;106(3):9.
|
| 21. |
Leśniowska J, Schubert A, Wojna M, Skrzekowska-Baran I, Fedyna M. Costs of diabetes and its complications in Poland. Eur J Heal Econ [Internet]. 2014;15(6):653-60. Available from: https://doi.org/10.1007/s10198-013-0513-0.
|
| 22. |
Marchildon GP, Schrijvers K. Physician Resistance and the Forging of Public Healthcare: A Comparative Analysis of the Doctors’ Strikes in Canada and Belgium in the 1960s. Med Hist [Internet]. 2012/05/17. 2011;55(2):203-22. Available from: https://www.cambridge.org/core/article/physician-resistance-and-the-forging-of-public-healthcare-a-comparative-analysis-of-the-doctors-strikes-in-canada-and-belgium-in-the-1960s/313899464C10EDEA7023DE4F00F67152.
|
| 23. |
OECD – Poland [Internet]. [cited 2023 Mar 10]. Available from: https://www.oecd.org/poland/.
|