Abstract
Background: For about 20 years we have been observing the development of three-dimensional (3D) printing. The aim of this study was to systematize the current knowledge on the use of 3D printing technology in neurosurgery and to attempt an outline the future paths of its development.
Material and methods: The analysis was based on English-language literature from 2017-2021 indexed in the Mendeley and Scopus databases.
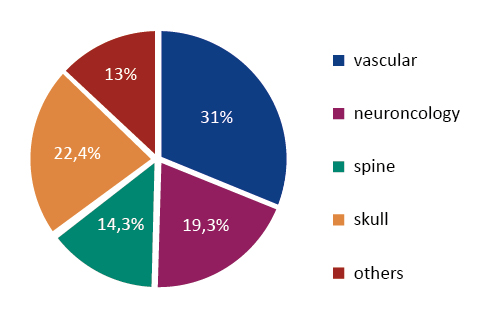
Results: The application of 3D printing in neurosurgery concerns: 1) teaching students, 2) training of residents neurosurgeons, 3) individualized surgery planning, 4) dedicated cranial and spinal implants, 5) the future of 3D printing in neurosurgical implantology. There were 5 main neurosurgery subtopics in which 3D printing was used: “vascular neurosurgery” (31%), “skull, cranial neurosurgery” (22.4%), “neuro-oncology” (19.3%), “spine” (14.3%) and “others” (13%). The number of published articles has been steadily increasing by 11-33% annually.
Conclusion: 3D printing has an enormous potential for clinical use and in the we will continue to observe its dynamic development. In neurosurgery 3D prints are currently most commonly used for didactic purposes as detailed anatomical models, for training residents and young surgeons and by specialists for the simulation of complex or innovative surgeries. The future of the use of additive 3D printing in neurosurgery lies in the biological 3D printing, the creation of artificial organs and the development of biological implants in tissue engineering.
Citation
Dzierżanowska N, Krakowiak M, Sokal P, Myszkowska B. The application of 3D printing in neurosurgery: present and future. Eur J Transl Clin Med. 2023;6(1):70-78Introduction
In recent decades we have observed a dynamic, even aggressive, introduction of modern technologies into medical practice. This includes computerization, implantology, transplantation, new techniques of macroscopic and microscopic imaging, endoscopy, navigation and finally the introduction of surgical robots such as Da Vinci systems, ROSA (Robotic Surgical Assistant) and others [1-3]. Altogether technology has opened new possibilities for modern medicine, science, teaching, standardization and repeatability of surgical techniques, shortening the operation time, increasing its safety and many others. The exact same benefits can be derived from the introduction of three-dimensional (3D) printing in neurosurgery. Simple anatomical models of individual organs made of clay or plaster have been known for hundreds of years and were used mainly as teaching aids. The 1980s marked the beginning of the development of 3D printing (at the time it was called stereolithography) pioneered by Charles Hull [4] mainly in the automotive and aerospace industries. The end of the 1990s witnessed the first 3D models of intracranial vascular pathologies (aneurysms and arteriovenous malformations) created for educational purposes [5]. Further development of computing power, modern methods of 2D radiological imaging, software-generated 3D images, printing of such models and the development of new materials imitating physical properties of human tissue has opened almost unlimited possibilities of using 3D models in science, education, surgical training or intraoperative implantology [6-14].
The aim of this study was to analyze both quantitatively and subject-wise the scientific literature concerning the use of additive (3D) printing technology in neurosurgery over the past 5 years, to demonstrate the trends in the use of this technology and its potential paths of future development.
Material and methods
We have analyzed the English-language full-text papers available in Scopus and Mendeley databases. One independent Author (ND) searched the databases using the keywords “neurosurgery” and “3D” and “print” or “printing” used in the title and/or abstract [15]. We narrowed the search to articles published in 2017-2021 with the following inclusion criteria: complete English-language text, original article, review paper, case report. Publications written in a language other than English, lacking full text, repeated in different scientific literature databases, not relevant to the topic, conference reports and book chapters were excluded from further analysis. We then performed a quantitative and qualitative analysis of the eligible papers. In the quantitative assessment, we calculated how the number and topics of the articles have changed over the years. For this purpose, consecutive keywords “tumor”, “vascular”, “aneurysm”, “malformation”, “spine”, “skull” and “cranial” were entered. In the qualitative analysis we assessed didactic and practical use of 3D printing by medical students, neurosurgery residents, specialists and researchers as well as weaknesses and most importantly, the future of 3D technology in neurosurgery.
Results
Quantitative evaluation
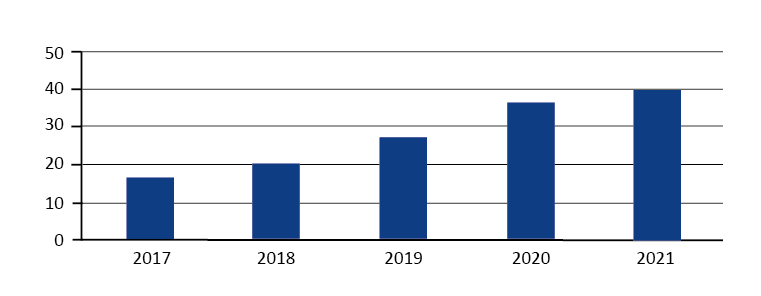
We initially found a total of 191 articles in the Scopus and 153 in the Mendeley database. Restricting the year of publish to 2017-2021, these values were respectively 141 and 94, resulting in a total of 235 papers on the use of additive printing in neurosurgery. Following the PRISMA protocol [15], applying the inclusion and exclusion criteria described above, a total of 140 articles were included for further detailed analysis. The number of published articles has been steadily increasing by 11% to 33% per year (Fig. 1).
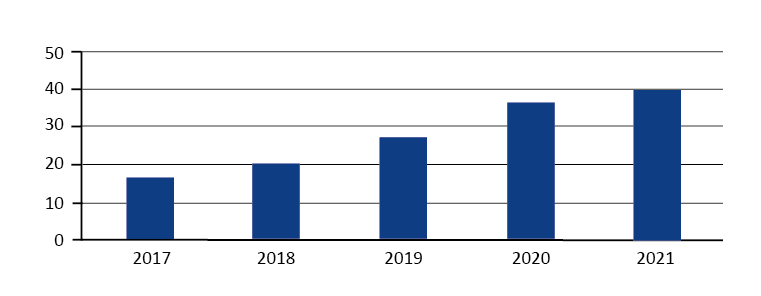
Figure 1. The number of articles about “neurosurgery and 3D printing” successively increased in the years 2017-2021
Articles were mainly written by authors from countries with a high index of technological, IT and industrial development: the United States, China and Germany. Despite the explicit keywords applied, the search yielded articles covering quite a few scientific disciplines including medicine, computer science, materials science, biochemistry, engineering, genetic engineering, etc. This made the study topic interesting and challenging because it required selection of the articles to those with medical application.
Subject evaluation
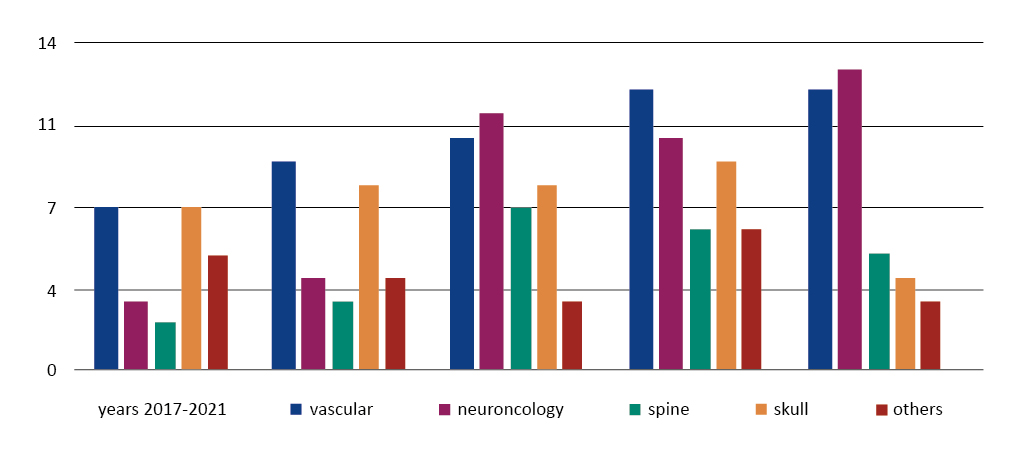
There were 4 main neurosurgery subtopics in which 3D printing was used: neuro-oncology, cerebrovascular anatomy and pathology (aneurysms, arteriovenous malformations), spine implantology and reconstruction of the skull bone defect. Some of the articles covered several topics in the use of 3D printing, hence quantitative percentage relationships were presented rather than absolute numbers. There was also an additional group “others” which accounted for as much as 13% of all topics and was dominated by such subjects as biopsy, insertion of DBS (deep brain stimulation), endoscopy, anatomy of nervous structures, morphometry, and tractography. Out of 140 articles we analyzed, 31% were focused on “vascular neurosurgery,” 22.4% on “skull, cranial neurosurgery,” 19.3% on “neuro-oncology,” 14.3% on “spine” and 13% concerned “others” (Fig. 2 and 3).
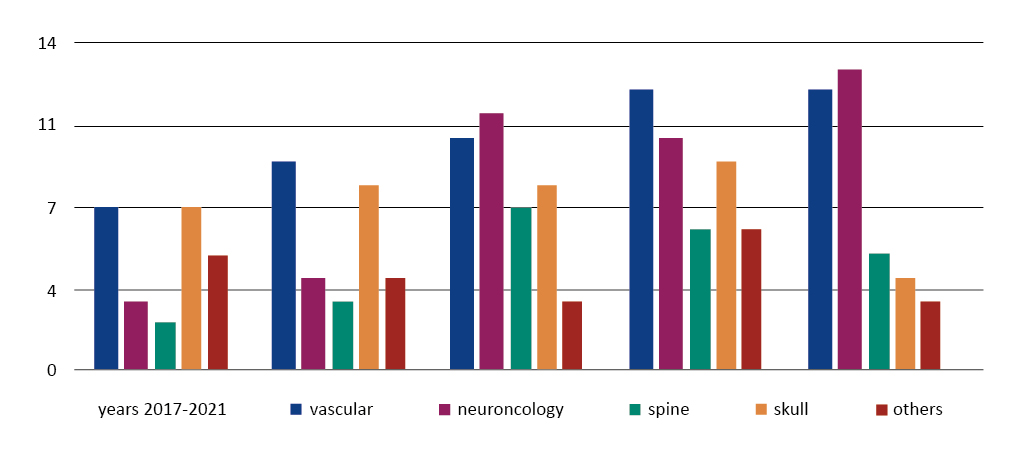
Figure 2. The number of articles focused on the 5 main subtopics published in each year from 2017 to 2021
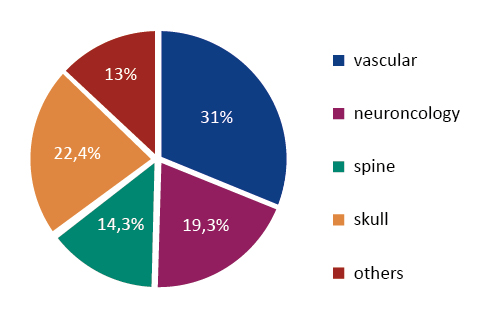
Figure 3. The percentage of “3D printing in neurosurgery” work in the context of the 5 main subtopics for the analysed time period 2017-2021
In the data we analyzed, it was possible to identify 6 themes that dominate the “neurosurgery vs. 3D printing” research. These are: 1) teaching of medical students, 2) training of residents and young neurosurgeons, 3) surgical planning, 4) custom/individual implants, 5) disadvantages of 3D printing and areas for improvement and 6) future developments in 3D printing development (near and distant future).
Discussion
In the literature we analyzed there was a significant increase in the number of articles on the topic of “neurosurgery vs. 3D printing” with 17 articles in 2017 and 40 in 2021 (11-33% increase per year). This confirms the general opinion about the interest of the science and industry communities in this topic, the progressive development of additive printing technology and its clinical or didactic usefulness. The largest amount of studies was related to “neuro-oncology”, “cerebrovascular” and “skull” and these are mainly models for training, surgery planning, new applications etc. [8, 10, 16-22]. This was a bit of a surprise, as other surgical specialties (e.g. general surgery, maxillofacial surgery) or dentistry are dominated by the topic of implantology and intraoperative use of models [23]. It would seem that it should be analogous in neurosurgery (spinal implants, dedicated interbody cages, stabilizing screws) [24-30]. The reason for this discrepancy may lie in the potential costs of such implants, which are so far higher than the standard spinal surgery implants [24-25, 30-32]. The same applies to the cost of printing cranial defects in reparative surgery compared to intraoperative manual fabrication of such defects from a plastic mass (polymethyl methacrylate, PMMA) [11, 14, 19, 33]. Whereas the guides and components of dental implants are made of fairly simple materials that are not subjected to the same forces as spinal implants. Moreover, they are printed quite commonly, so their cost is lower compared to the cost of neurosurgical implants. In general, the issue of cost is one of the disadvantages of 3D printing and is discussed later in the paper. We did not separate the articles about pediatric neurosurgery, as there were only 15 articles regarding this patient group and were focused on training for brain tumor biopsy, ventriculocisternostomy in hydrocephalus, treatment of skull deformities in the course of craniosynostosis [7, 11-12, 14, 20].
Medical student education
The educational usefulness of 3D prints in medicine has been observed ever since their introduction [6, 34]. As their shapes and availability improve, the market is actively growing. This is due to the cost of such models, which are reusable and can last for years, the limited number of professional anatomy laboratories, the limited number of human models to teach medical students. It is important to bear in mind the ever-increasing number of students, not only of medicine and dentistry, but also of other health sciences e.g. physiotherapy, radiology technology, dietetics, nursing sub-specialties. Let’s not forget the fine arts and physical education students.
Training of residents and young neurosurgeons
For quite many years it has been possible to notice a change in the type of training of residents from the form of gaining experience in the operating room to maximizing learning on phantoms and 3D radiological images. This is obviously due to ethical (ensuring patient safety) and legal reasons. The use of reconstructed images of MRI, CT examinations for this purpose is very useful, but not sufficient. It is the printed spatial models that help teach how the position of anatomical structures will change when the angle of view of the surgical field shifts during aneurysm clipping or how to safely bypass eloquent fields (motor and sensory pathways) in brain tumor resection [8, 16-17, 20, 35]. They can also be used to practice simple surgical procedures like biopsy, craniotomy or spinal canal decompression [19, 29-30, 37]. Moreover, 3D Prints help clarify the communication with patients, e.g. explain the surgical procedure and obtain the informed consent. [10-13, 28, 33-36].
Planning operations, new techniques and surgical accesses
Regular training of the acquired skills is necessary to maintain high professional qualifications of the neurosurgeon. For this purpose, during courses neurosurgeons can perform simulated operations either on fresh frozen human cadavers or anaesthetized animals (e.g. pigs). 3D phantoms can significantly help to organize such courses. In addition, the surgeon can plan the individual steps of the operation based on a specific case after preparing an additive model of a tumor, aneurysm or the patient's spine [8,11-13, 18, 25-27, 38-39]. Here we enter the domain of personalized medicine, dedicated to a specific patient. Such models can also serve as material for research on modifying the surgical approach or even developing innovative spinal or cranial repair procedures [16, 21-22, 31, 40].
Intraoperative use of 3D implants
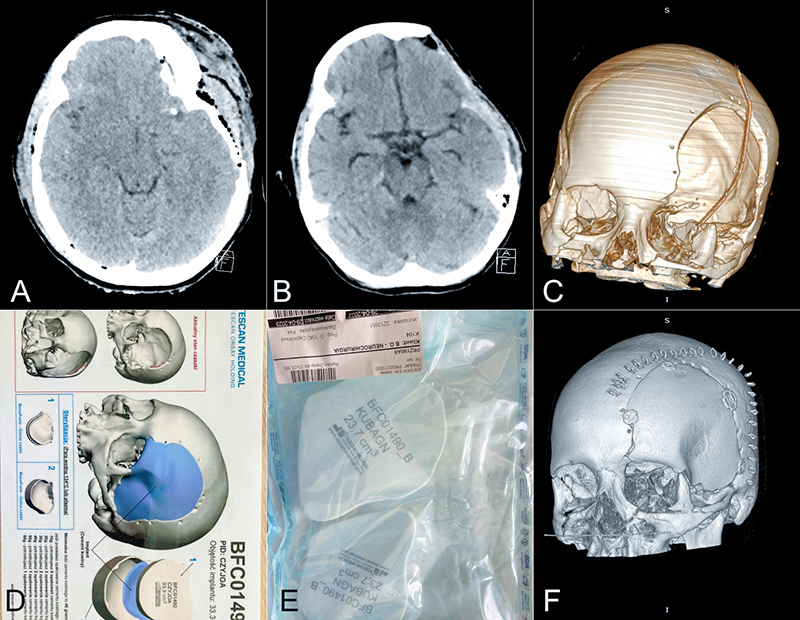
Currently in the literature, the use of additive printing in neurosurgery focuses on cranial bone repair surgeries and much less frequently on spinal surgeries [14, 25-26, 41]. Restorative operations include craniosynostosis-related procedures in the pediatric patients and in adults, the replenishment of the cranial bone after a craniectomy [11, 14, 41]. Currently, in the intraoperative setting the neurosurgeon prepares a specific fragment by hand from PMMA mass and attaches it in place of the defect [41-42]. In children, various proprietary material such as ribs are used. Intraoperative preparation of the synthetic component requires time, which may increase the overall cost of surgery and the final cosmetic results are not as good as with a computer-prepared implant. Based on a preoperative CT scan of the skull bone (mirror-image), 3D files of the missing bone fragment are prepared, which can then be printed and transplanted to the patient after sterilization [11, 14, 31, 33, 41-42] – see the Fig. 4. The downside of course is still the cost, as mentioned below [41, 43].
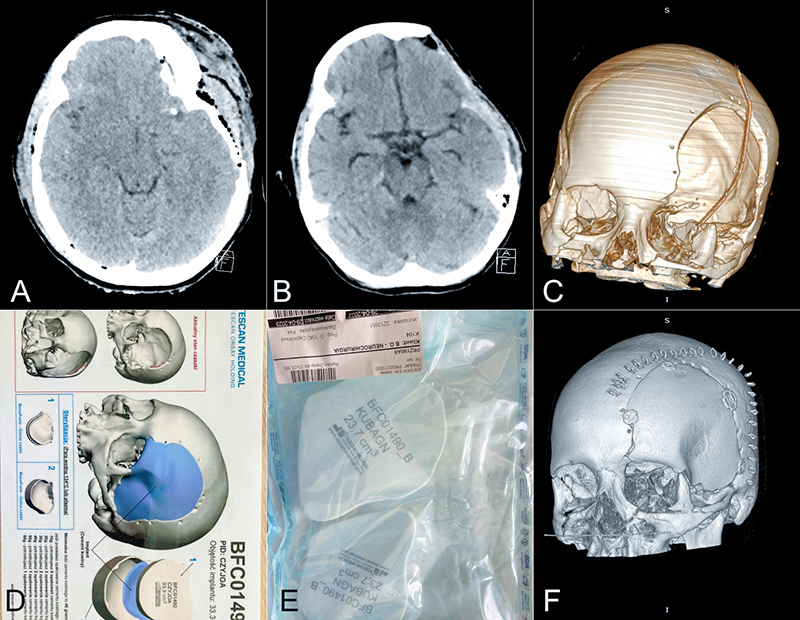
Figure 4. A) CT scan of the head (transverse section) – patient age 29, craniofacial trauma, fracture of left temporal and frontal bone with compression of the brain tissue and subdural hematoma, B) follow-up head CT after decompression surgery (in this case a fronto-temporal craniectomy), C) 3D reconstruction of the skull with a visible post-craniectomy bone defect, D) package with the material for 3D printing of cranial bone flap, E) 3D prints of cranial bone cavity flap prepared for sterilization, F) 3D reconstruction of the skull after surgery cranioplasty
The near future of 3D printing
Short-term developments are consequences of today's limitations of the 3D printing technology: cost, print quality, preparation time and material available. The cost of printing ranges from a few tens of US dollars (USD) to several thousand (these are the costs of materials, software, processing, human labor by computer scientists, engineers, technicians, doctors, etc.) [43]. Currently, this is one of the main factors limiting the widespread clinical use of this technology. The cost of the 3D printer itself is an expense of several to several hundred thousand USD, not to mention the costs of hardware, software, printing material and involvement of people in the production of the final product. The authors emphasize that the widespread use and availability of 3D printing technology will drive the further development of the hardware and software as well as the decrease in costs on the basis of competition. It must be remembered that models have a limited life span due to wear and tear during training and must be successively replaced [19, 44].
Further 3D print development depends on materials used and thus requires improvement
The development of, bioengineering, creation of new materials imitating the physical properties of human tissue and organ fragments, printing with multiple materials simultaneously, must go hand in hand [45-46]. Further development of increased resolution of computed tomography (CT), magnetic resonance (MR) and other examinations is necessary [46-47]. The time of print preparation ranges from several hours to even a few days. It is crucial to reduce this time in order to increase the neurosurgeons’ interest in using 3D prints for scheduled and in urgent operations, e.g. intraoperative printing in case of post-traumatic skull bone defects. This creates the need for technical development of printers, fast computer processors as well as durable, efficient mechanical components [47]. Another element is the involvement of IT specialists, radiologists, technicians, neurosurgeons (e.g. residents) within the hospital to introduce procedures that will allow rapid implementation of treatment offered by 3D printing. The scope of printing is most often limited to a given organ or anatomical structure and is devoid of adjacent tissues and structures that are of colossal importance during surgery. Thus, further development should aim towards printing entire models with simultaneous use of multiple materials, something along the lines of a print that is done on an already printed part (print-in-print-out) [45].
The distant future of 3D printing
The 3D printing has great potential to revolutionize personalized medicine, i.e. individualized treatment for a specific patient, especially in the field of implantology. In the case of neuro-traumatology, this is already happening (cranial bone defects, spinal implants for stabilization, artificial discs). However, looking into the future, the most promising route is that of bioprinting of complex tissues, molecular printing, so-called “living” implants. That is, on the one hand, targeted stimulation of stem cell growth into a specific cell line and, on the other hand, biomatrices on which the growth and development of tissues or organ fragments will be postulated [48-50]. Currently, it remains at the laboratory stage and in order to have a clinical application many elements need to be improved (or developed), e.g. increasing the resolution to the sub-cellular level (moving on the nanometric scale) [49-51]. Another challenge is the viability of bioprints, a suitable interface with sufficient mechanical properties to allow adequate interaction with the rest of the tissue or organ. This interaction concerns activities such as blood flow, growth, oxidation, neurological stimulation, secretory, functionality, etc. [50, 52]. Another expected advance is 3D in situ printing, which involves real-time fabrication of specific tissues during surgical intervention. Here, developments in engineering, computer science are needed to achieve printing speeds for utility [49, 51].
Limitations
One of the limitations of our analysis is that the articles generally emphasized the clinical, intraoperative utility of 3D printing, which we also cite. It would be worthwhile to expand the research on this issue with a meta-analysis of clinical papers to find out whether and by how much the time of surgery decreased, by how much the cost of surgery actually changed, to what extent the use of 3D prints increased the safety of surgery or reduced the complications. Most papers are dominated only by the surgeon's subjective feelings. Such an analysis is difficult because clinical papers cover very heterogenous cases (central nervous system tumors, spine instrumentation procedures, peripheral nerve treatment) and low repeatability of cases. Another issue concerns the future of bioprinting, i.e. the use of tissue that imitates the properties of living tissue. However, this topic has been described laconically in the reviewed papers as the future rather than an advancement of current research. The programming of tissue culture matrices or other bio-elements, the use of induced stem cells are mentioned [48]. The problem itself is extremely perplexing and worth extending. However, the literature selection protocol we used (PRISMA) limited our analysis only to already existing applications in neurosurgery or “smuggled out” some futurological issues [15]. Thus, it is worthwhile to focus separately only on the topic of "future of 3D printing applications" and analyze articles in the field of tissue engineering, genetic engineering, molecular biology, transplantology, etc. Moreover, Further work of highly-qualified specialists in complex multidisciplinary teams is crucial to ensure the development of the 3D printing technology, because the knowledge of medicine seems to be clearly insufficient for such a complex task.
Conclusions
Based on our analysis of the literature, five basic conclusions can be drawn regarding 3D printing in neurosurgery:
- It has an enormous potential for clinical use and the constantly increasing number of published studies about it confirms that in the upcoming years we will see a dynamic development in this field.
- Research on 3D printing in neurosurgery is most often focused on neuro-oncology and cerebrovascular diseases.
- Currently in neurosurgery, 3D prints are most commonly used for educational purposes as detailed anatomical models, for training residents and young surgeons and by specialists for the simulation of complex or innovative operations.
- The future of the use of additive printing in neurosurgery lies in implantology and the spine and skull reconstruction fields are the most advanced in this matter.
- The development of biological 3D printing, the creation of artificial organs, the advancement of biological implants (tissue engineering) may bring the greatest clinical benefits
Funding
None.
Conflicts of interests
None.
References
| 1. |
Liu L, Mariani SG, De Schlichting E, Grand S, Lefranc M, Seigneuret E, Chabardès S. Frameless ROSA® Robot-Assisted lead implantation for deep brain stimulation: technique and accuracy. Oper Neurosurg (Hagerstown). 2020 Jul;19(1):57-64. Available from: https://journals.lww.com/onsonline/Fulltext/2020/07000/Frameless_ROSA__Robot_Assisted_Lead_Implantation.9.aspx.
|
| 2. |
Marcus HJ, Hughes-Hallett A, Cundy TP, Yang GZ, Darzi A, Nandi D. da Vinci robot-assisted keyhole neurosurgery: a cadaver study on feasibility and safety. Neurosurg Rev. 2015 Apr;38(2):367-71. Available from: https://doi.org/10.1007/s10143-014-0602-2.
|
| 3. |
Bonda DJ, Pruitt R, Goldstein T, Varghese A, Mittler M, Schneider S, Shah A, Rodgers S. Robotic Surgical Assistant (ROSA™) Rehearsal: using 3-dimensional printing technology to facilitate the introduction of stereotactic robotic neurosurgical Equipment. Oper Neurosurg (Hagerstown). 2020 Jul;19(1):94-97. Available from: https://journals.lww.com/onsonline/Fulltext/2020/07000/Robotic_Surgical_Assistant__ROSA___Rehearsal_.13.aspx.
|
| 4. |
Hull CW. Apparatus for production of three-dimensional objects by stereolithography, U.S. Patent No. 4,575,330. Washington, D.C.: U.S. Patent and Trademark Office, 1986.
|
| 5. |
D'Urso PS, Hall BI, Atkinson RL, Weidmann MJ, Redmond MJ. Biomodel-guided stereotaxy. Neurosurgery. 1999 May;44(5):1084-1093. Available from: https://europepmc.org/article/med/10232542.
|
| 6. |
Waqas M, Mokin M, Lim J, Vakharia K, Springer ME, Meess KM, Ducharme RW, Ionita CN, Nagesh SVS, Gutierrez LC, Snyder KV, Davies JM, Levy EI, Siddiqui AH. Design and physical properties of 3-dimensional printed models used for neurointervention: A systematic review of the literature. Neurosurgery. 2020 Sep;87(4):E445-E453. Available from: doi: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8101092/.
|
| 7. |
Parthasarathy J, Krishnamurthy R, Ostendorf A, Shinoka T, Krishnamurthy R. 3D printing with MRI in pediatric applications. J Magn Reson Imaging. 2020 Jun;51(6):1641-1658. Available from: https://doi.org/10.1002/jmri.26870.
|
| 8. |
Lan Q, Zhu Q, Xu L, Xu T. Application of 3D-printed craniocerebral model in simulated surgery for complex intracranial lesions. World Neurosurg. 2020 Feb;134:e761-e770. Available from: https://doi.org/10.1016/j.wneu.2019.10.191.
|
| 9. |
Leal A, Souza M, Nohama P. Additive Manufacturing of 3D biomodels as adjuvant in intracranial aneurysm clipping. Artif Organs. 2019 Jan;43(1):E9-E15. Available from: https://doi.org/10.1111/aor.13303.
|
| 10. |
Kosterhon M, Neufurth M, Neulen A, Schäfer L, Conrad J, Kantelhardt SR, Müller WEG, Ringel F. Multicolor 3D printing of complex intracranial tumors in neurosurgery. J Vis Exp. 2020 Jan 11;(155). Available from: https://www.jove.com/t/60471/multicolor-3d-printing-of-complex-intracranial-tumors-in-neurosurgery.
|
| 11. |
Cheng D, Yuan M, Perera I, O'Connor A, Evins AI, Imahiyerobo T, Souweidane M, Hoffman C. Developing a 3D composite training model for cranial remodeling. J Neurosurg Pediatr. 2019 Sep 20:1-10. Available from: https://doi.org/10.3171/2019.6.PEDS18773.
|
| 12. |
Weinstock P, Rehder R, Prabhu SP, Forbes PW, Roussin CJ, Cohen AR. Creation of a novel simulator for minimally invasive neurosurgery: fusion of 3D printing and special effects. J Neurosurg Pediatr. 2017 Jul;20(1):1-9. Available from: https://doi.org/10.3171/2017.1.PEDS16568.
|
| 13. |
Ganguli A, Pagan-Diaz GJ, Grant L, Cvetkovic C, Bramlet M, Vozenilek J, Kesavadas T, Bashir R. 3D printing for preoperative planning and surgical training: a review. Biomed Microdevices. 2018 Aug;20(3):65. Available from: https://link.springer.com/article/10.1007/s10544-018-0301-9.
|
| 14. |
Ghizoni E, de Souza JPSAS, Raposo-Amaral CE, Denadai R, de Aquino HB, Raposo-Amaral CA, Joaquim AF, Tedeschi H, Bernardes LF, Jardini AL. 3D-printed craniosynostosis Model: New simulation surgical tool. World Neurosurg. 2018 Jan;109:356-361. Available from: https://doi.org/10.1016/j.wneu.2017.10.025.
|
| 15. |
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. Available from: https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
|
| 16. |
Mooney MA, Cavallo C, Zhou JJ, Bohl MA, Belykh E, Gandhi S, McBryan S, Stevens SM, Lawton MT, Almefty KK, Nakaji P. Three-dimensional printed models for lateral skull base surgical training: Anatomy and simulation of the transtemporal approaches. Oper Neurosurg (Hagerstown). 2020 Feb;18(2):193-201. Available from: https://journals.lww.com/onsonline/Fulltext/2020/02000/Three_Dimensional_Printed_Models_for_Lateral_Skull.10.aspx.
|
| 17. |
Błaszczyk M, Jabbar R, Szmyd B, Radek M. 3D printing of rapid, low-cost and patient-specific models of brain vasculature for use in preoperative planning in clipping of intracranial aneurysms. J Clin Med. 2021;10(6):1201. Available from: https://doi.org/10.3390/jcm10061201.
|
| 18. |
Wang JL, Yuan ZG, Qian GL, Bao WQ, Jin GL. 3D printing of intracranial aneurysm based on intracranial digital subtraction angiography and its clinical application. Medicine (Baltimore). 2018 Jun;97(24):e11103. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6023659/.
|
| 19. |
Todnem N, Nguyen KD, Reddy V, Grogan D, Waitt T, Alleyne CH. A simple and cost-effective model for ventricular catheter placement training: technical note. J Neurosurg. 2020 May;134(5):1640-1643. Available from: https://doi.org/10.3171/2020.2.JNS19161.
|
| 20. |
Coelho G, Chaves TMF, Goes AF, Del Massa EC, Moraes O, Yoshida M. Multimaterial 3D printing preoperative planning for frontoethmoidal meningoencephalocele surgery. Childs Nerv Syst. 2018 Apr;34(4):749-756. Available from: https://link.springer.com/article/10.1007/s00381-017-3616-6.
|
| 21. |
Ding CY, Yi XH, Jiang CZ, Xu H, Yan XR, Zhang YL, Kang DZ, Lin ZY. Development and validation of a multi-color model using 3-dimensional printing technology for endoscopic endonasal surgical training. Am J Transl Res. 2019 Feb;11(2):1040-1048. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6413258.
|
| 22. |
Okonogi S, Kondo K, Harada N, Masuda H, Nemoto M, Sugo N. Operative simulation of anterior clinoidectomy using a rapid prototyping model molded by a three-dimensional printer. Acta Neurochir (Wien). 2017 Sep;159(9):1619-1626. Available from: https://ci.nii.ac.jp/naid/500001083542/.
|
| 23. |
Tack P, Victor J, Gemmel P, Annemans L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online. 2016 Oct;15(1):115. Available from: https://link.springer.com/article/10.1186/s12938-016-0236-4.
|
| 24. |
Tu Q, Ceh H, Ding HW, Tu GW, Miao QJ, Shen JJ, Huang XH, Tango Y, Xia H, Xu JZ. Three-dimensional printing technology for surgical correction of congenital scoliosis caused by hemivertebrae. World Neurosurgery 2021 May;149:969-981. Available from: https://doi.org/10.1016/j.wneu.2021.01.063.
|
| 25. |
Chen YY, Chao LC, Fang JJ, Lee EJ. 3D-customized guiding template for posterior fixation in complex atlantoaxial instability-preliminary experiences of National Cheng Kung University Hospital. J Neurol Surg Rep. 2020 Jan;81(1):20-27. Available from: https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0039-1695795.
|
| 26. |
Zhao Y, Ma Y, Liang J, Luo H, Cai X, Xu Y, Lu S. Comparison of the 3D-printed operation guide template technique and the free-hand technique for S2-alar-iliac screw placement. BMC Surg. 2020;20(1):258. Available from: https://link.springer.com/article/10.1186/s12893-020-00930-5.
|
| 27. |
Parthasarathy J, Sribnick EA, Ho ML, Beebe A. Customised hybrid CT-MRI 3D-printed model for grade V spondylolisthesis in an adolescent. BMJ Case Rep. 2021 Mar 1;14(3):e239192. Available from: https://casereports.bmj.com/content/14/3/e239192.abstract.
|
| 28. |
Rashim K, Pawan VK, Sinha VD. Increasing the safety of surgical treatment for complex Cranio-vertebral anomalies using customized 3D printed models. J Clin Neurosci. 2018 Feb;48:203-208. Available from: https://doi.org/10.1016/j.jocn.2017.10.061.
|
| 29. |
Clifton W, Nottmeier E, Edwards S, Damon A, Dove C, Refaey K, Pichelmann M. Development of a novel 3D printed phantom for teaching neurosurgical trainees the freehand technique of C2 laminar screw placement. World Neurosurg. 2019 Sep;129:e812-e820. Available from: https://doi.org/10.1016/j.wneu.2019.06.038.
|
| 30. |
Yu C, Ou Y, Xie C, Zhang Y, Wei J, Mu X. Pedicle screw placement in spinal neurosurgery using a 3D-printed drill guide template: a systematic review and meta-analysis. J Orthop Surg Res. 2020 Jan;15(1):1. Available from: https://link.springer.com/article/10.1186/s13018-020-1548-4.
|
| 31. |
Nguyen B, Ashraf O, Richards R, Tra H, Huynh T. Cranioplasty using customized 3-dimensional–printed titanium implants: An international collaboration effort to improve neurosurgical care. World Neurosurg. 2021 May;149:174-180. Available from: https://doi.org/10.1016/j.wneu.2021.02.104.
|
| 32. |
Zhang L, Yang G, Johnson BN, Jia X. Three-dimensional (3D) printed scaffold and material selection for bone repair. Acta Biomater. 2019 Jan 15;84:16-33. Available from: https://doi.org/10.1016/j.actbio.2018.11.039.
|
| 33. |
Kwarcinski J, Boughton P, van Gelder J, Damodaran O, Doolan A, Ruys A. Clinical evaluation of rapid 3D p rint‐formed implants for surgical reconstruction of large cranial defects. ANZ J Surg 2021 Sep;91:1226–1232. Available from: https://doi.org/10.1111/ans.16361.
|
| 34. |
Gargiulo P, Árnadóttir I, Gíslason M, Edmunds K, Ólafsson I. New directions in 3D medical modeling: 3D-printing anatomy and functions in neurosurgical planning. J Healthc Eng. 2017;2017:1439643. Available from: https://doi.org/10.1155/2017/1439643.
|
| 35. |
Gomez-Feria J, Narros JL, Ciriza GG, Roldan-Lora F, Schrader IM, Martin-Rodríguez JF, Mir P. 3D printing of diffuse low-grade gliomas involving eloquent cortical areas and subcortical functional pathways: Technical note. World Neurosurg. 2021 Mar;147:164-171.e4. Available from: https://doi.org/10.1016/j.wneu.2020.12.082.
|
| 36. |
Damon A, Clifton W, Valero-Moreno F, Quinones-Hinojosa A. Cost-effective method for 3-dimensional printing dynamic multiobject and patient-specific brain tumor models: technical note. World Neurosurg. 2020 Aug;140:173-179. Available from: https://doi.org/10.1016/j.wneu.2020.04.184.
|
| 37. |
Byvaltsev V, Polkin R, Bereznyak D, Giers MB, Hernandez PA, Shepelev V, Aliyev M. 3D-printed cranial models simulating operative field depth for microvascular training in neurosurgery. Surg Neurol Int. 2021 May 10;12:213. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8168712/.
|
| 38. |
Dho YS, Lee D, Ha T, Ji SY, Kim KM, Kang H, Kim MS, Kim JW, Cho WS, Kim YH, Kim YG, Park SJ, Park CK. Clinical application of patient-specific 3D printing brain tumor model production system for neurosurgery. Sci Rep. 2021 Mar;11(1):7005. Available from: https://link.springer.com/content/pdf/10.1038/s41598-021-86546-y.pdf.
|
| 39. |
Huang X, Liu Z, Wang X, Li XD, Cheng K, Zhou Y, Jiang XB. A small 3D-printing model of macroadenomas for endoscopic endonasal surgery. Pituitary. 2019 Feb;22(1):46-53. Available from: https://link.springer.com/article/10.1007/s11102-018-0927-x.
|
| 40. |
Pöppe JP, Spendel M, Schwartz C, Winkler PA, Wittig J. The "springform" technique in cranioplasty: custom made 3D-printed templates for intraoperative modelling of polymethylmethacrylate cranial implants. Acta Neurochir (Wien). 2021 Dec; 6:1-10. Available from: https://link.springer.com/article/10.1007/s00701-021-05077-7.
|
| 41. |
Dabadi S, Dhungel RR, Sharma U, Shrestha D, Gurung P, Shrestha R, Pant B. Customized Cost-Effective Polymethyl-Methacrylate Cranioplasty Implant Using Three-Dimensional Printer. Asian J Neurosurg. 2021 Mar 20;16(1):150-154. Available from: https://www.thieme-connect.com/products/ejournals/html/10.4103/ajns.AJNS_441_20.
|
| 42. |
Kim MJ, Lee HB, Ha SK, Lim DJ, Kim SD. Predictive Factors of Surgical Site Infection Following Cranioplasty: A Study Including 3D Printed Implants. Front Neurol. 2021 Nov 2;12:745575. Available from: https://doi.org/10.3389/fneur.2021.745575.
|
| 43. |
Maclachlan LR, Alexander H, Forrestal D, Novak JI, Redmond M. Properties and Characteristics of Three-Dimensional Printed Head Models Used in Simulation of Neurosurgical Procedures: A Scoping Review. World Neurosurg. 2021 Dec;156:133-146.e6. Available from: doi: https://doi.org/10.1016/j.wneu.2021.09.079.
|
| 44. |
Nicolosi F, Pessina F, Clarissa Ann EG, Belotti F, Mahoney D, Agosti E, Serioli S, Saraceno G, Dimitrov A, Rossini Z, Spena G. New neuroanatomy learning paradigms for the next generation of trainees: A novel literature-based 3D methodology. Clin Neurol Neurosurg. 2021;210. Available from: http://dx.doi.org/10.1016/j.clineuro.2021.106948.
|
| 45. |
Watanabe N, Yamamoto Y, Fujimura S, Kojima A, Nakamura A, Watanabe K, Ishi T, Murayama Y. Utility of multi-material three-dimensional print model in preoperative simulation for glioma surgery. J Clin Neurosci. 2021 Nov;93:200-205. Available from: https://doi.org/10.1016/j.jocn.2021.09.017.
|
| 46. |
McGuire LS, Fuentes A, Alaraj A. Three-Dimensional Modeling in Training, Simulation, and Surgical Planning in Open Vascular and Endovascular Neurosurgery: A Systematic Review of the Literature. World Neurosurg. 2021 Oct;154:53-63. Available from: https://europepmc.org/article/med/34293525.
|
| 47. |
Pucci JU, Christophe BR, Sisti JA, Connolly ES Jr. Three-dimensional printing: technologies, applications, and limitations in neurosurgery. Biotechnol Adv. 2017 Sep;35(5):521-529. Available from: https://doi.org/10.1016/j.biotechadv.2017.05.007.
|
| 48. |
Jovanovich N, Habib A, Kodavali C, Edwards L, Amankulor N, Zinn PO. The Evolving Role of Induced Pluripotent Stem Cells and Cerebral Organoids in Treating and Modeling Neurosurgical Diseases. World Neurosurg. 2021 Nov;155:171-179. Available from: https://doi.org/10.1016/j.wneu.2021.08.081.
|
| 49. |
Li X, Liu B, Pei B, Chen J, Zhou D, Peng J, Zhang X, Jia W, Xu T. Inkjet bioprinting of biomaterials. Chem Rev. 2020 Oct;120(19):10793-10833. Available from: https://doi.org/10.1021/acs.chemrev.0c00008.
|
| 50. |
Zhu W, Ma X, Gou M, Mei D, Zhang K, Chen S. 3D printing of functional biomaterials for tissue engineering. Curr Opin Biotechnol. 2016 Aug;40:103-112. Available from: https://doi.org/10.1016/j.copbio.2016.03.014.
|
| 51. |
Liu G, David BT, Trawczynski M, Fessler RG. Advances in pluripotent stem cells: history, mechanisms, technologies, and applications. Stem Cell Rev Rep. 2020 Feb;16(1):3-32. Available from: https://link.springer.com/article/10.1007/s12015-019-09935-x.
|
| 52. |
Agarwal T, Banerjee D, Konwarh R, Esworthy T, Kumari J, Onesto V, Das P, Lee BH, Wagener FADTG, Makvandi P, Mattoli V, Ghosh SK, Maiti TK, Zhang LG, Ozbolat IT. Recent advances in bioprinting technologies for engineering hepatic tissue. Mater Sci Eng C Mater Biol Appl. 2021 Apr;123:112013. Available from: https://doi.org/10.1016/j.msec.2021.112013.
|