Abstract
Background: Transpedicular screw placement remains the gold standard technique for stabilization of the lumbar spine.
Material and methods: This is a retrospective study that analyzes patients that underwent the spinal stabilization surgical procedure. We compared results from two independent neurosurgical centers. In the years 2012-2015, the O-arm and StealthStation neuronavigation system was used for implantation of transpedicular screws. From 2018 to 2020 the transcutaneous pedicle screw placement procedure was performed using a standard C-arm device.
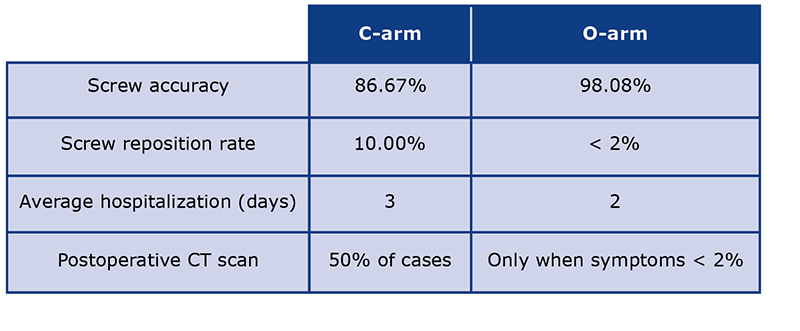
Results: In 208 procedures performed with the O-arm device, the accuracy of screw position was 98.08%. Screw repositioning was necessary in 1.92% of all cases. In the 30 procedures that were performed using the C-arm, the accuracy of the screws was 86.7% and the screw reposition procedure accounted for 10% (in one case screws were not replaced due to clinical sequelae).
Conclusions: Our data show that the spinal fusion with the O-arm tool has more accuracy, thus might be more indicated in procedures that require minimally invasive spinal stabilization.
Citation
Krakowiak M, Sokal P, Rusinek M, Rudaś M. Comparison of the O-arm and C-arm guided pedicle screw placement. Eur J Transl Clin Med. 2022;5(2):31-36Introduction
There are many causes of spinal instability e.g. to trauma, congenital abnormalities, tumor invasion and degenerative process. Changes in lifestyle of the majority of the population and increasing incidence of obesity, directly contributes to high demand for low back pain treatment because of the destabilization as the part of the degenerative process. Because of the reduction in muscle mass along with increasing body weight, the degenerative processes of the vertebral discs and facet joints lead to spinal destabilization. This process can present with spondylolisthesis of the adjacent spinal motor segments.
At the same time, patient՚s are increasingly interested in minimally invasive treatment with the maximum reduction of the stress associated with surgery (e.g. reduced time of hospitalization and reduced need for painkillers). Spinal stabilization system with neuronavigation seems to meet those demands. In this article we present the results of such procedures in comparison with C-arm technique. In the beginning of the learning curve, we encountered technical problems which contributed to the prolongation of the procedure. Nevertheless, gained experience allowed us to significantly shorten the procedure time and to preserve its safety and accuracy.
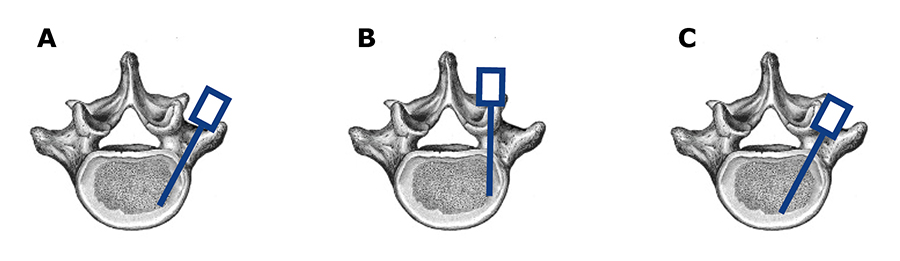
Correct placement of the screws was widely discussed in the literature (Fig. 1) [1-3]. However, still it is difficult to assess the spinal destabilization by referring to one imaging method. Secondly, sufficient level of spine stabilization differs amongst patients and directly depends on their age, lifestyle and expected quality of life. Degenerative spondylolisthesis may show that the destabilization process did occur, although due to natural progression of the degenerative process the spine became re-stabilized, therefore there is no need for screw implantation. In some neurosurgery centers, placement of intervertebral implant is a standalone indication for bilateral transpedicular stabilization. Since the removed vertebral disc accounts in 80% Comparison of the O-arm and C-arm guided pedicle screw placement for motor segment stabilization and intervertebral arthrodesis is a prolonged process. The literature does not describe clear advantages of any technique over another [4-5]. In recent years, placement of the screws could be easily planned using the O-arm navigation technique, which was first introduced in 2006. Thus, it is possible to plan the exact position of the screw not only in the pedicle and also in the vertebral body in order to avoid damage of the adjacent vessels. Although this technique seems to be very accurate with low number of side effects reported, there are still updates of inappropriate screw placement or displacement of implanted material due to insufficient bone fusion.
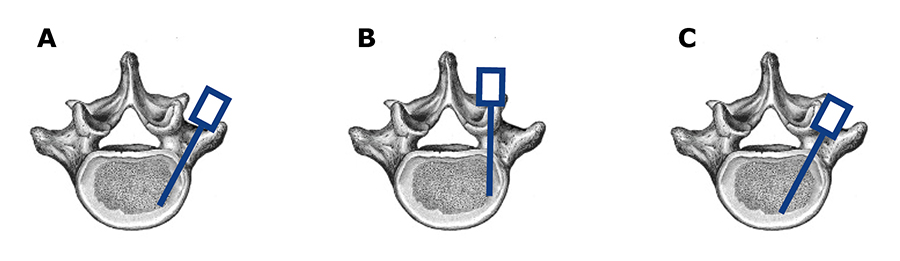
Figure 1. Types of screw corridor in transpedicular spinal fusion. A – transcortical screw placement, B – insertion through pedicle with engagement of the transverbal joint, C – insertion through pedicle without joint involvement
The exact criteria for screw reposition are still unclear. Taking into consideration only clinical criteria, e.g. post-operative pain of the spine or post-operative pain radiating to the lower limbs, seems to be insufficient to asses screw placement. Literature shows that clinical symptoms along with inappropriate screw placement that violates more than 4 mm in the pedicle, is an indication to reposition the screws [6]. More confounding might be the fact that some patients do not report any symptoms, despite the fact that their computed tomography (CT) scan shows inappropriate screw placement which violates pedicle or pierces the vertebral body. Moreover, appropriate fixation of the screws correlates not only with good transition through the pedicle but also depends on the bone density and its availability to heal.
When comparing the C-arm to O-arm stabilization, the accuracy of pedicle screw placement seems to be the main advantage pointing on the O-arm technique [7-10]. Nevertheless, there is still a concern about high radiation exposure, due to the necessity to perform a 3 dimensional (3D) CT scan before and after the procedure. We should not forget about the fact that one CT scan provides the radiation exposure that is acceptable for one patient in one year period [11]. Based on the recent literature, it seems to be clear that this radiation exposure might be substantially reduced by obtaining a low-dose 3D scan, which offers acceptable imaging quality [12-15].
Material and Methods
In a 4-year period (2012-2015) a total of 208 transpedicular stabilization procedures were performed using the O-arm Surgical Imaging with StealthStation navigation system (Medtronic USA/Ireland). Clinical data were analyzed retrospectively. There were 106 males (51%) and 102 (49%) females in the research group. Their age varied from 20 to 95 years (median 56.5 years). Majority of the patients were in 5th or 6th decade of life. Lumbar stabilization was obtained in 93% and thoracic stabilization in 7% of the cases. Trauma was the indication for the spinal stabilization in 10.6% of the cases. Screw insertion was done by the same operator in 86.5% of all cases. In summary, four surgeons where performing the transpedicular screw placement procedure. Whereas, neuronavigation planning procedure was done by other three surgeons. Standard screws with 5.5 mm diameter were used in all procedures. The length of the screws was assessed based on an intra-operative CT scan performed using the O-arm device.
In a 2-year period (2018-2020) 30 transpedicular stabilization procedures using the C-arm (Siemens, Germany) were performed. There were 12 (40%) females and 18 (60%) males in this research group. The patients’ age varied from 28 to 75 years (median 58.5 years). Lumbar stabilization was obtained in 76.7% of the cases, thoracic stabilization in 23.3%. In 30% of the cases trauma was the indication for spinal stabilization. There were more than five different operators performing surgery. In all cases standard 5.5 mm screws were used. Postoperative CT scan was done in 50% of the cases and it was always performed when patient had reported significant postoperative pain symptoms. In 3 cases (10%), reposition procedure was done with satisfactory outcome. One patient was not re-operated despite of inappropriate screw placement. Although the screw has been positioned in the S1 recess and it violated more than 4mm of the pedicle, the patient did not report any symptoms and the stability of the implanted material was not compromised, we decided not to perform surgery.
As we progressed along the learning curve, we made some modifications to the O-arm screw fusion procedure resulting in shorter operation time and lower dose of radiation applied to the patient and personnel in the operating room. In the years 2012-2013, the 3D scan was performed after every stabilization procedure. After year 2013, the 3D scan was performed only in case of suspected incorrect screw placement. Multiplanar images were assessed in the operating room by the operator and surgeon involved in planning procedure. If a 3D scan was not performed postoperatively and patient reported clinical symptoms, a CT scan was obtained (usually on the day of the operation) to precisely assess screw placement. When screw implantation of all the screws was not possible due to difficult anatomical conditions, previously placed screws were removed and only nerve root decompression was performed.
Pedicle breach was suspected post-operatively when the patient reported clinical symptoms such as radicular pain (radiating to the lower limb) or low back pain. However, post-operative pain rarely was due to inappropriate screw placement, because the pain has subsided without intervention during standard post-operative hospitalization period. CT imaging studies were reviewed by the radiologist and the operator that performed the procedure. Incorrect position of the screws was recognized on the CT scan in case of conflict of the screw with nerve structures or when the position of the screws could suggest instability of the implanted material.
Depending on the patien՚s diagnosis and clinical symptoms, additional nerve root decompression or discectomy was performed. Patient was placed in the prone position on a carbon table to ensure adequate X-ray radiation translucency. Placement of the screws was always performed through the guide rod that confirmed the proper entrance of the screws along the planned trajectory.
Side of the decompression was chosen on the basis of imaging studies and clinical symptoms of radiculopathy, such as positive straight leg raise test (positive Lasègue sign) and pain distribution consistent with a given dermatome. To qualify a patient for the procedure, clinical symptoms had to be consitent with the radiological findings. If the patient needed nerve root decompression, in all cases it was done before the stabilization procedure, in order to preserve the conditions after nerve root decompression. In patients diagnosed with spondylosis, screw fixation was done unilaterally. In all cases of spondylolisthesis bilateral stabilization was obtained to ensure appropriate segmental stabilization.
The O-arm system with Stealth Station provides 2- and 3-D images of the spine. A 3D image is necessary to plan the insertion of the screws, thus it was performed after the navigation frame was placed. The scanned image is merged and gives real-time position of the certain tools that are used intraoperatively, based on the reference frame that registers appropriate 3D image in space. Besides 3D navigation, the O-arm is still used with the C-arm function during the operation. It is based on surgeon preferences to assess appropriate placement of the wires which guide the trajectory for the screw placement. The screws are placed transcutaneously to minimize tissue trauma, in contrast to the open procedure where a large group of the paraspinal muscles has to be dissected. The length of the screws depends on anatomical conditions shown in the 3D scan. Planning was done in the operating theatre prior to the procedure.
Results
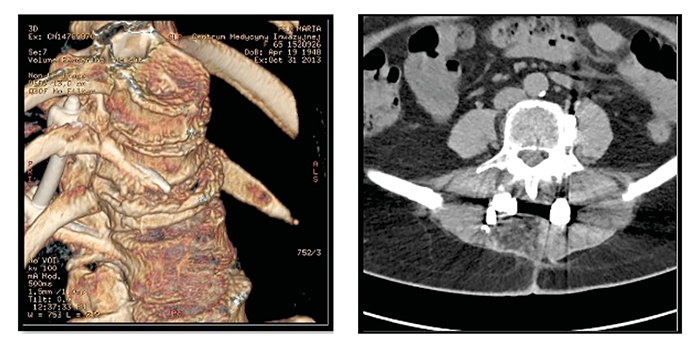
Of the 208 cases of transpedicular stabilizations performed using the O-arm device in years 2012-2015, 93% were lumbar and only 7% thoracic. Accuracy rate of the screw positioning was 98.08% and reposition rate was 1.92% (5 patients, Tab. 1). In the group of patients who required screw reposition, 4 required lumbar and one thoraco-lumbar stabilization. Among patients that needed screw revision, in 4 cases inappropriate screw position was detected in the 3D scan that was performed at the end of the operation (Fig. 2). In case of one patient the 3D scan was not done in the operating theater and the inappropriate screw position was noted in the CT scan that was ordered because of his clinical symptoms. Infection rate was 0.48% (1 patient) and multiple antibiotics were needed due to resistant infection. No screw displacement was found in that patient.
Table 1. Comparison of C-arm vs O-arm techniques
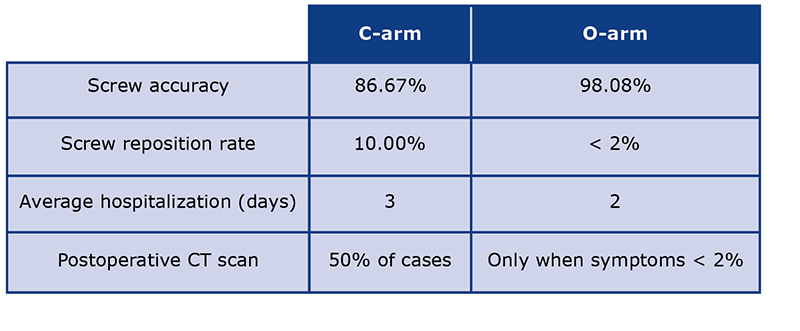
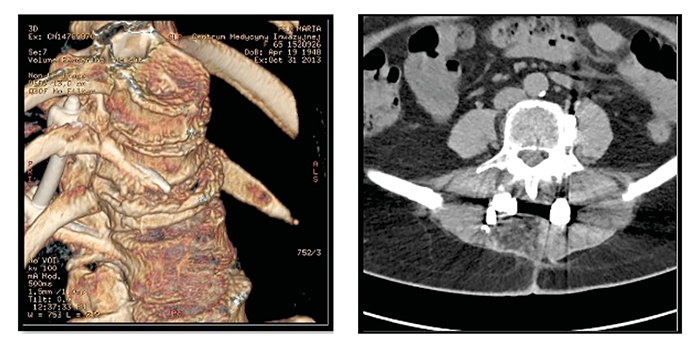
Figure 2. Post-operative CT scan revealed inappropriate screw placement, in this case outside the vertebral body, which caused insufficient support for the spinal stabilization.
In 67 cases spondylolisthesis was the indication for surgery (32.2%). Spondylosis, defined as the degeneration of intervertebral discs of different etiologies, was the indication for surgery in 42.3% of cases (88 patients). Trauma was an indication for surgery in 21 cases (10% of all cases), discopathy with low back pain 7.2% (15 patients) and tumor 2.4% (5 patients).
In the 30 procedures performed using the C-arm, the accuracy of the screws was 86.67% and the screw reposition procedure accounted for 10%. In case of one patient, the radiological exam revealed a screw inside the S1 recess. He was not qualified for the reposition procedure because of lack of symptoms. In both the C-arm and O-arm research groups there were no concerns about the stability of the entire transpedicular fixation system. In the C-arm group 23% of cases (7) were due to traumatic fracture. 73% (13) cases were due to spondylotic degenerative changes. Median hospitalization time was shorter in the O-am group (2 days), compared to the C-arm patients (3 days).
Discussion
Minimal invasiveness seems to be the most important goal from the perspective of the patients, doctors and the costs. The comparison of both groups shows advantages of the O-arm procedure in respect of the minimal invasion, accuracy and safety of the procedure. Although the price of the O-arm device might limits its universal use, one should not ignore factors such as reduction of the hospitalization time and cost of analgesia. Further health economics studies are needed to assess these factors [1, 2].
As we gained experience in performing the O-arm procedure, we observed improvement in the process and the possibility to skip some of the steps recommended by the manufacturer, allowing us to reduce the radiation exposure for patients and medical staff, without additional complications or side effects. Even the low-dose 3D O-arm scan is connected with high radiation exposure [15, 16]. It seems beneficial to not obtain the second (post-operative) 3D scan unless it is indicated. Abandoning the post-operative 3D scan was not associated with a higher need for reposition of implanted screws. In summary, 4 out of 5 inappropriately placed screws were suspected by the operator and the additional 3D scan was done to assess their position. In one case the post-operative 3D scan was not obtained, however that procedure was performed by a surgeon who did not have experience in the O-arm procedure. The accuracy rate of 98.08% is comparable to that reported in the literature (97.5%) [17].
Those results confirm that the O-arm technique is very accurate in planning and placing transpedicular screws. Furthermore, it is associated with very low incidence of infection due to the fact that small incisions were required for this procedure. Due to low traumatization of the tissue, patient group required less amounts of analgesics and typical length of postoperative hospitalization was only two days.
While gaining the experience with the O-arm implantation technique some problems appeared, which marked the importance of certain steps during the operation procedure that required additional precautions. The main issue was to implant the reference frame correctly with most stability on the spinous process and then to supervise its position to avoid picture shift during merging. Among some groups of patients, we have encountered the anatomical disproportion of the pedicles. Available screws were too large to place them safely in the pedicles without anatomical compromise of the periosteum. Amongst some of the patients, particularly in the L5-S1 region, the anatomical relations prevent appropriate titanium bar placement. In these cases, the curvatures of the spine were of great importance. The inappropriate angle between the L5 vertebrae and the iliac crest made it much more difficult or even in some cases impossible to place the titanium stabilization bar. For this reason, in some cases conversion to the open surgical procedure was necessary.
Among patients with large amounts of subcutaneous tissue in the lower back area, we observed difficulties in placing the titanium bar near the lamina, due to the limitation of the device used. Despite the fact that screw placement was planned using neuronavigation station, it was impossible to match the titanium bar with the screw cups. A preferred solution turned out to be implantation of longer screws which gave better access to their cups, where titanium bar was placed.
Analysis of the O-arm reposition group revealed that frame shift was the main cause of inappropriate screw implantation. Adequate reference frame fixation is critical, when trying to avoid shifting complications. Moreover, the analysis indicated that the planned position of the screws on the lateral side of the pedicle reduces the risk of instability of the implanted screws. In the following years, exposure to X-ray radiation was reduced by obtaining only low-dose 3D scans and by verifying the position of the screws in 2D scans, thus reducing the radiation dose both for the patient and staff.
21 patients were qualified to O-arm stabilization procedure because of trauma. Stabilization was performed by fixing the healthy vertebra with each other, one below the fracture and one above. No additional healthy vertebral levels were used to reinforce the stabilization strength. Despite the fact that no additional levels were included in transpedicular fusion, no displacement or signs of destabilization were seen. However, in the group of trauma patients, it was necessary to perform another 3D scan after unilateral stabilization, because of the change of anatomical relations and in order to prevent damage to neuronal structures.
The O-arm guided transpedicular stabilization seems to be a reliable and minimally invasive method. This observation was also confirmed in double-blinded studies at unrelated neurosurgical centers and meta-analyses [1-3].
Conclusions
Despite the initially prolonged surgical time, the O-arm guided transpedicular stabilization becomes more intuitive the more often it is used, thus the learning curve contributes to more efficient and faster procedure without side effects along the line. Consequently, the initial investment in expensive equipment might be justified by avoiding the potential cost-generating adverse effects, prolonged hospitalization and higher doses of pain medications. Nevertheless, those hypotheses have to be investigated in other studies.
Funding
None.
Conflicts of interest
None.
References
| 1. |
Feng W, Wang W, Chen S, Wu K, Wang H. O-arm navigation versus C-arm guidance for pedicle screw placement in spine surgery: a systematic review and meta-analysis. Int Orthop [Internet]. 2020 May 7;44(5):919–26. Available from: http://link.springer.com/10.1007/s00264-019-04470-3.
|
| 2. |
Shin M-H, Ryu K-S, Park C-K. Accuracy and Safety in Pedicle Screw Placement in the Thoracic and Lumbar Spines : Comparison Study between Conventional C-Arm Fluoroscopy and Navigation Coupled with O-Arm® Guided Methods. J Korean Neurosurg Soc [Internet]. 2012;52(3):204. Available from: http://jkns.or.kr/journal/view.php?doi=10.3340/jkns.2012.52.3.204.
|
| 3. |
Tabaraee E, Gibson AG, Karahalios DG, Potts EA, Mobasser J-P, Burch S. Intraoperative Cone Beam–Computed Tomography With Navigation (O-ARM) Versus Conventional Fluoroscopy (C-ARM): A Cadaveric Study Comparing Accuracy, Efficiency, and Safety for Spinal Instrumentation. Spine (Phila Pa 1976) [Internet]. 2013;38(22). Available from: https://journals.lww.com/spinejournal/Fulltext/2013/10150/Intraoperative_Cone_Beam_Computed_Tomography_With.19.aspx.
|
| 4. |
Ambati D V, Wright EK, Lehman RA, Kang DG, Wagner SC, Dmitriev AE. Bilateral pedicle screw fixation provides superior biomechanical stability in transforaminal lumbar interbody fusion: a finite element study. Spine J [Internet]. 2015;15(8):1812–22. Available from: https://www.sciencedirect.com/science/article/pii/S1529943014006469.
|
| 5. |
Chen C, Cao X, Zou L, Hao G, Zhou Z, Zhang G. Minimally invasive unilateral versus bilateral technique in performing single-segment pedicle screw fixation and lumbar interbody fusion. J Orthop Surg Res [Internet]. 2015;10(1):112. Available from: https://doi.org/10.1186/s13018-015-0253-1.
|
| 6. |
Costa F, Villa T, Anasetti F, Tomei M, Ortolina A, Cardia A, et al. Primary stability of pedicle screws depends on the screw positioning and alignment. Spine J [Internet]. 2013;13(12):1934–9. Available from: https://www.sciencedirect.com/science/article/pii/S1529943013003963.
|
| 7. |
Bolger C, Kelleher MO, McEvoy L, Brayda-Bruno M, Kaelin A, Lazennec J-Y, et al. Electrical conductivity measurement: a new technique to detect iatrogenic initial pedicle perforation. Eur Spine J [Internet]. 2007;16(11):1919–24. Available from: https://doi.org/10.1007/s00586-007-0409-8.
|
| 8. |
Tian N-F, Xu H-Z. Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop [Internet]. 2009;33(4):895–903. Available from: https://doi.org/10.1007/s00264-009-0792-3.
|
| 9. |
Kosmopoulos V, Schizas C. Pedicle Screw Placement Accuracy: A Meta-analysis. Spine (Phila Pa 1976) [Internet]. 2007;32(3). Available from: https://journals.lww.com/spinejournal/Fulltext/2007/02010/Pedicle_Screw_Placement_Accuracy__A_Meta_analysis.22.aspx.
|
| 10. |
Costa F, Cardia A, Ortolina A, Fabio G, Zerbi A, Fornari M. Spinal Navigation: Standard Preoperative: Versus: Intraoperative Computed Tomography Data Set Acquisition for Computer-Guidance System: Radiological and Clinical Study in 100 Consecutive Patients. Spine (Phila Pa 1976) [Internet]. 2011;36(24). Available from: https://journals.lww.com/spinejournal/Fulltext/2011/11150/Spinal_Navigation__Standard_Preoperative__Versus_.15.aspx.
|
| 11. |
Santos ERG, Ledonio CG, Castro CA, Truong WH, Sembrano JN. The Accuracy of Intraoperative O-arm Images for the Assessment of Pedicle Screw Postion. Spine (Phila Pa 1976) [Internet]. 2012;37(2). Available from: https://journals.lww.com/spinejournal/Fulltext/2012/01150/The_Accuracy_of_Intraoperative_O_arm_Images_for.19.aspx.
|
| 12. |
Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) [Internet]. 1990;15(1):11–4. Available from: http://europepmc.org/abstract/MED/2326693.
|
| 13. |
Esses SI, Bednar DA. The spinal pedicle screw: techniques and systems. Orthop Rev [Internet]. 1989;18(6):676–82. Available from: http://europepmc.org/abstract/MED/2664668.
|
| 14. |
Suresh P, M. LE, L. BE, Hiroyuki Y, V. PV. Pedicle Screw Placement With O-arm and Stealth Navigation. Orthopedics [Internet]. 2012 Jan 16;35(1):e61–5. Available from: https://doi.org/10.3928/01477447-20111122-15.
|
| 15. |
Abul-Kasim K, Söderberg M, Selariu E, Gunnarsson M, Kherad M, Ohlin A. Optimization of Radiation Exposure and Image Quality of the Cone-beam O-arm Intraoperative Imaging System in Spinal Surgery. Clin Spine Surg [Internet]. 2012;25(1). Available from: https://journals.lww.com/jspinaldisorders/Fulltext/2012/02000/Optimization_of_Radiation_Exposure_and_Image.8.aspx.
|
| 16. |
Su AW, Luo TD, McIntosh AL, Schueler BA, Winkler JA, Stans AA, et al. Switching to a Pediatric Dose O-Arm Protocol in Spine Surgery Significantly Reduced Patient Radiation Exposure. J Pediatr Orthop [Internet]. 2016 Sep;36(6):621–6. Available from: https://journals.lww.com/01241398-201609000-00012.
|
| 17. |
Van de Kelft E, Costa F, Van der Planken D, Schils F. A Prospective Multicenter Registry on the Accuracy of Pedicle Screw Placement in the Thoracic, Lumbar, and Sacral Levels With the Use of the O-arm Imaging System and StealthStation Navigation. Spine (Phila Pa 1976) [Internet]. 2012;37(25). Available from: https://journals.lww.com/spinejournal/Fulltext/2012/12010/A_Prospective_Multicenter_Registry_on_the_Accuracy.15.aspx.
|