Abstract
Fast-tracking in cardiac care refers to the complex intervention including early extubation, care during anesthesia, mobilization and hospital discharge to reduce perioperative morbidity, costs, and length of stay in the intensive care unit and the hospital. This review was designed to evaluate early extubation protocols, the differences in early and late extubation, the safety and efficacy of early extubation among the patients in surgical intensive care after coronary artery bypass graft (CABG) surgery. The analyzed studies showed many significant differences in the mortality and postoperative complications of time-directed extubation practices and low dose-based general anesthesia in patients with low to moderate risk undergoing early extubation (fast-track) and the conventional care methods. Different fast-track interventions could diminish extubation time, costs, and the length of hospital stay. However, several factors including patient’s stay in the intensive therapy ward vs general ward, patient selection, skills and experience of the staff, and fast-track anesthesia methods could be considered to perform safe fast-tracking in patients undergoing cardiac surgery. On the other hand, to achieve this safety for high-risk cardiosurgery patients multidisciplinary coordination is needed.
Citation
Jannati M. Early extubation protocol post-coronary artery bypass graft & open heart surgery. Eur J Transl Clin Med. 2022;5(2):75-81Introduction
Post-operative outcome improvement directly depends on fundamental alterations in anesthesia and surgery, extracorporeal perfusion methods and peri-operative care systems [1-2]. Fast‐track cardiac care, also called early extubation, has been first described by Prakash et al. in 1977 [3]. Fast-tracking in cardiac care refers to the complex intervention including early extubation, care during anesthesia, mobilization and hospital discharge to reduce perioperative morbidity, costs, and length of stay in the intensive care unit and the hospital. Efforts have continued to reduce the risk of respiratory complications due to tracheal intubation, mechanical ventilation and other risk factors including age and several thoracic surgical approaches [1, 4-8] The main goal of the majority of fast-track protocols was to optimize the length of patients’ stay (LOS) and to reduce total costs following the coronary artery bypass graft (CABG) surgery, by emphasizing on early and fast extubation at the surgical intensive care unit (SICU) [9-13].
Based on the Society of Thoracic Surgeons (STS) guidelines, a 6-hour time point is considered “early extubation” and “prolonged intubation” referred to the longer than 24 hours time points [14-17] There is an ongoing interest in early extubation due to prevent adverse effects associated with late extubation, as well as any extra costs [18-19] However, due to the heterogeneity in cardiac surgery patient populations, previously advocated practices and risk prediction protocols have not been very successful. There are some confusing points in terms of the increased complication rate time in CABG.
The aim of this review is to determine the effect of early intubation time on post-operative morbidity and mortality rate in patients undergoing general anesthesia following the valve and CABG surgery.
Material and methods
In this review study, we evaluated all articles published from the year 2000 to 2021 related to early extubation protocols post-coronary artery bypass graft and open-heart surgery. Articles were searched by one researcher in PubMed, Web of Science, Scopus, Google Scholar, Science Direct and Cochrane Library using the keywords “early extubation”, “early extubation protocol”, “coronary artery bypass graft” and “open heart surgery.”
Results
A total of 296 articles were extracted in the initial search. After reviewing the abstracts of these articles, 76 articles were selected and their full texts were included in the analysis.
History of early extubation following major surgery
Fast‐track cardiac care has been applied in most of the study population (123 of 142 adult patients) after or within 3 h following open-heart surgery [3]. The best candidates for this approach were the patients who have been given minimal fluids and had a decrease in the cardiac index and ventricular filling pressures [20]. They reported immediate extubation in 5/36 patients and an average time of 6 h for the remainder of that group. Other researchers presented successful extubation 8 hours after surgery [21-22]. In another article, the best candidates for early extubation were hemodynamically stable, had an alveolar-arterial gradient of < 150 mmHg, good donor liver function and no encephalopathy [23]. In a combined strategy including all levels of care for the early 48 h after liver transplantation, the time to extubation and LOS at ICU were shorter, without changes in staff and intraoperative protocols [24].
Fast-track in cardiac care
Fast-track cardiac care referred to the complex intervention including cardiac anesthesia care and the post-operative care with a special focus on early extubation after surgery to diminish hospital LOS and expenses [25-26] In conventional (not fast-track) care units, high-dose opioid-based anesthesia has been applied in cardiac surgery followed by overnight mechanical breathing support in ICU after cardiac surgery [25]. However, in the new fast-track care units mechanical breathing support is applied on the operating table or within hours after cardiac surgery via the time-directed protocols for breathing support removal [27]. A Cochrane review updated in 2016 included 28 trials with 4438 participants. Most participants have been considered to be at low to moderate risk of death after surgery. No differences in risk of mortality were observed between lowdose versus high-dose opioid-based general anesthesia groups (OR 0.53, 95% CI 0.25 to 1.12; 8 trials, 1994 participants, low level of evidence) within the first year of surgery. There were also no differences in risk of mortality between a time-directed extubation protocol versus conventional care (OR 0.80, 95% CI 0.45 to 1.45; 10 trials, 1802 participants, low level of evidence). They showed no significant differences in postoperative complications including myocardial infarction, stroke, and tracheal re-intubation between the mentioned study groups [27]. Application of low-dose opioid-based general anesthesia and time-directed extubation procedures using the fast-track method have major postoperative complications and mortality risk as well as conventional (not fast-track) method suggesting its safety for use in low to moderate risk patients [27].
Opinions for and against fast-track anesthesia
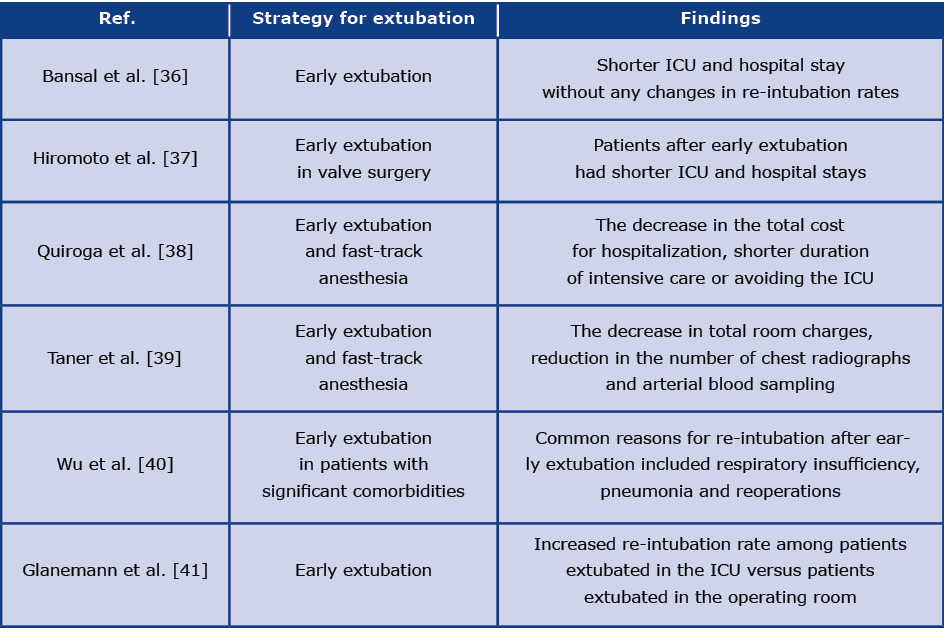
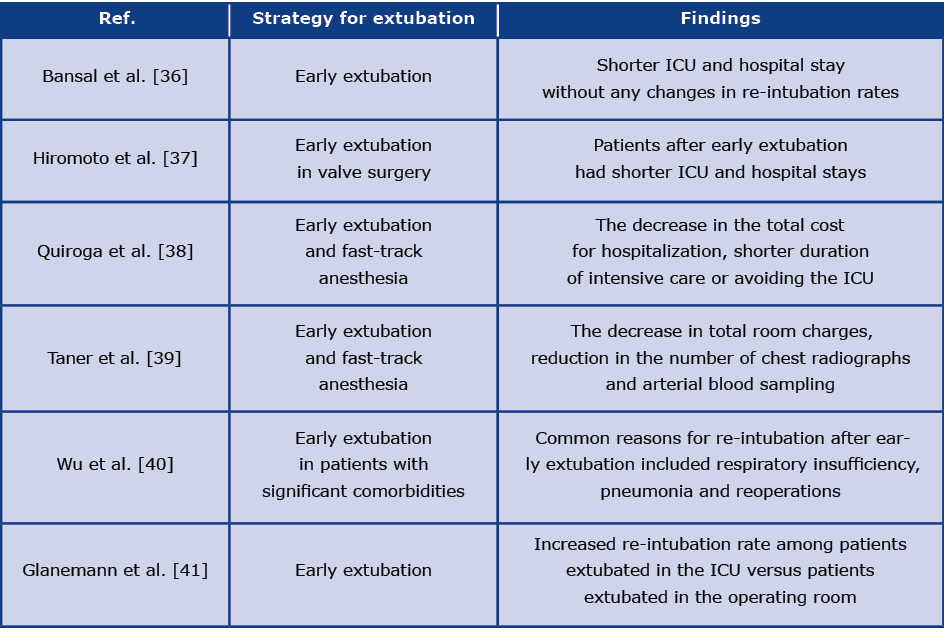
Among the advantages of fast-track anesthesia are improved graft blood flow, decreased complications from mechanical ventilation, fewer chest radiographs, improved resource utilization patient comfort, and cost containment [28]. Disadvantages include the chance of failed extubation and re-operation. In addition, there is a lack of large prospective studies regarding the benefits of the fast-track approach [28] (see Table 1).
Table 1. Summary of the pros and cons of the fast-track approaches
Some concerns have been reported regarding the increased rate of re-intubation and the risk for perioperative adverse effects after early extubation, particularly among old or high-risk patients [29-32]. The safety of early extubation after CABG has been shown in a community practice of 6446 CABG patients from 35 hospitals, aged 65 years and older with shorter hospital stays without any adverse effect on postoperative outcomes between 1995 to 1998 [33]. In a retrospective analysis of findings in 1,904 patients undergoing CABG with different intubation times after surgery including 0-6, 6-9, 9-12, 12-24, and over 24 hours, there was no increase in postoperative complications before 12 hours of intubation [34]. It has been reported that prolonged intubation time can be increased mortality and morbidity rate in CABG patients [25] [27, 35]. Shorter ICU and hospital LOS were observed in patients who extubated earlier after the operation.
Feasibility of fast-track approach in cardiac surgery
It has been reported that the fast-track approach could be feasible in both simple and complex surgical procedures in all age groups [26]. Although early extubation is a fundamental part of the fast-track approach, there is no universal definition of ”early” and currently it is referred to as 6-8 hours post-cardiac surgery) [26]. In a study of 197 pediatric patients the successful extubation rate was 61% in the operating room (OR) [42]. In another study, 67% of children were extubated in the OR following surgery for congenital heart disease or within 6 hours of admission to the ICU without complications [43]. The patient/parent satisfaction, the feasibility, and safety of the fast-track approach in cardiac surgery have been found in large-scale series of patients undergoing adult cardiac surgery [44]. In a retrospective study, the extubation rate of 73% was observed in the OR of 901 patients [45]. The findings of another study showed the extubation rate of 87% in OR as an ultra-fast track method in elective congenital cardiac surgery [46]. Mittnacht et al. showed 79% extubation rate in OR of 224 patients [47].
Discussion
There is considerable disagreement regarding the classification of fast-track and ultrafast-track techniques. Several time points between 1 and 24 hours are considered for extubation following cardiac surgery [48]. However, careful patient selection is considered a critical aspect of fast-tracking in many patients undergoing cardiac surgery [49-50]. Early or fast extubation could be lessened the length of ICU and hospital stays [51-52]. However, multidisciplinary and coordinated approaches seem necessary to safely accomplish fast-tracking. The benefits of fast-tracking in cardiac surgery have been proven by mostly retrospective analyses compared to prospective randomized studies [1, 30-31, 38, 48, 51] In a survey of 10 randomized clinical trials, early extubation compared to late extubation after cardiac surgery and the beneficial effect of fast-tracking as a reduced time of mechanical ventilation, shorter times of ICU and hospital stay, and resource usage was observed between the studies [53]. Hiromoto et al. evaluated the benefits and predictive value of early extubation in valve surgery needing long cardiopulmonary bypass and reported that early extubation was achieved in 44.3% of patients without increasing adverse events. Patients with early extubation had shorter ICU and hospital stays [37]. Ellis et al. demonstrated that after implementing a fast-track extubation protocol, the number of early extubations after cardiac surgery was successfully improved and fast-track extubation did not increase the re- -intubation risk and other adverse events [54].
To prevent major cardiorespiratory complications, it is important to shorten the duration of intensive hemodynamic monitoring and endotracheal intubation after cardiac surgery, particularly in some higher-risk patients [55-56]. On the other hand, there is wide heterogeneity in pre-and intra-operative risk factors of fast-tracking and prolonged mechanical ventilation observed in developing countries [57]. In addition, the application of low-dose anesthesia following the early cessation method combined with the rapid reversal of muscle paralysis is considered the main aspect of intervention in some RCTs [49, 58-59]. Bansal et al. showed that early extubation could be associated with a shorter ICU and hospital stay with any changes in re-intubation rates [36]. Findings obtained from six clinical trials in a Cochrane Review showed no differences in the re-intubation rate, 30- day mortality and intensive care mortality in patients who were extubated within 8 hours after cardiac surgery [60]. Factors such as higher body surface space and extended ischemic times are considered prognostics of longer extubation times [61-62]. Other published studies did not display the relation between early extubation and higher rates of re-intubation [60, 63].
Conclusion
In conclusion, early extubation after cardiac surgeries reduces the length of ICU and hospital stay, reduces the total cost of care as well as the number of blood sampling and chest radiographs, however, it may increase the risk of re-intubation. No difference in mortality rate was observed due early extubation after cardiac surgeries.
References
| 1. |
Reis J, Mota J., Ponce P, Costa-Pereira A, Guerreiro M. Early extubation does not increase complication rates after coronary artery bypass graft surgery with cardiopulmonary bypass. Eur J Cardio-Thoracic Surg [Internet]. 2002 Jun;21(6):1026–30. Available from: https://academic.oup.com/ejcts/article-lookup/doi/10.1016/S1010-7940(02)00121-5.
|
| 2. |
Grocott HP. Early extubation after cardiac surgery: The evolution continues. J Thorac Cardiovasc Surg [Internet]. 2017 Nov;154(5):1654–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022522317315659.
|
| 3. |
Prakash O, Jonson B, Meij S, Bos E, Hugenholtz P, Nauta J, et al. Criteria for Early Extubation After Intracardiac Surgery in Adults. Anesth Analg [Internet]. 1977 Sep;56(5):703-708. Available from: http://journals.lww.com/00000539-197709000-00019.
|
| 4. |
Kastanos N, Estopá Miró R, Marín Perez A, Xaubet Mir A, Agustí-Vidal A. Laryngotracheal injury due to endotracheal intubation: incidence, evolution, and predisposing factors. A prospective long-term study. Crit Care Med [Internet]. 1983 May;11(5):362–7. Available from: http://journals.lww.com/00003246-198305000-00009.
|
| 5. |
Quasha AL, Loeber N, Feeley TW, Ullyot DJ, Roizen MF. Postoperative respiratory care: a controlled trial of early and late extubation following coronary-artery bypass grafting. In: The Journal of the American Society of Anesthesiologists [Internet]. The American Society of Anesthesiologists; 1980. p. 142–8. Available from: https://watermark.silverchair.com/0000542-198002000-00007.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAv8wggL7BgkqhkiG9w0BBwagggLsMIIC6AIBADCCAuEGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMowsNxcHhrsVS5ahDAgEQgIICsmPZ7fNFnW5AM-mI3w18wqbiy2M63yZ.
|
| 6. |
Gammon RB, Shin MS, Buchalter SE. Pulmonary Barotrauma in Mechanical Ventilation. Chest [Internet]. 1992 Aug;102(2):568–72. Available from: https://linkinghub.elsevier.com/retrieve/pii/S001236921634065X.
|
| 7. |
Gibney RTN, Wilson RS, Pontoppidan H. Comparison of Work of Breathing on High Gas Flow and Demand Valve Continuous Positive Airway Pressure Systems. Chest [Internet]. 1982 Dec;82(6):692–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0012369215369300.
|
| 8. |
Fagon J-Y, Chastre J, Domart Y, Trouillet J-L, Pierre J, Darne C, et al. Nosocomial Pneumonia in Patients Receiving Continuous Mechanical Ventilation: Prospective Analysis of 52 Episodes with Use of a Protected Specimen Brush and Quantitative Culture Techniques. Am Rev Respir Dis [Internet]. 1989 Apr;139(4):877–84. Available from: http://www.atsjournals.org/doi/abs/10.1164/ajrccm/139.4.877.
|
| 9. |
Higgins TL. Pro: early endotracheal extubation is preferable to late extubation in patients following coronary artery surgery. J Cardiothorac Vasc Anesth [Internet]. 1992 Aug;6(4):488–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1498307.
|
| 10. |
Engelman RM, Rousou JA, Flack JE, Deaton DW, Humphrey CB, Ellison LH, et al. Fast-track recovery of the coronary bypass patient. Ann Thorac Surg [Internet]. 1994 Dec;58(6):1742–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/0003497594916748.
|
| 11. |
Arom K V., Emery RW, Petersen RJ, Schwartz M. Cost-effectiveness and predictors of early extubation. Ann Thorac Surg [Internet]. 1995 Jul;60(1):127–32. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0003497595003568.
|
| 12. |
Lee JH, Kim KH, VanHeeckeren DW, Murrell HK, Cmolik BL, Graber R, et al. Cost analysis of early extubation after coronary bypass surgery. Surgery [Internet]. 1996 Oct;120(4):611–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0039606096800079.
|
| 13. |
Konstantakos AK, Lee JH. Optimizing timing of early extubation in coronary artery bypass surgery patients. Ann Thorac Surg [Internet]. 2000 Jun;69(6):1842–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0003497500012480.
|
| 14. |
Trouillet J-L, Combes A, Vaissier E, Luyt C-E, Ouattara A, Pavie A, et al. Prolonged mechanical ventilation after cardiac surgery: Outcome and predictors. J Thorac Cardiovasc Surg [Internet]. 2009 Oct;138(4):948–53. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022522309008125.
|
| 15. |
Canver CC, Chanda J. Intraoperative and postoperative risk factors for respiratory failure after coronary bypass. Ann Thorac Surg [Internet]. 2003 Mar;75(3):853–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0003497502044934.
|
| 16. |
Edwards FH, Clark RE, Schwartz M. Coronary artery bypass grafting: The Society of Thoracic Surgeons National Database experience. Ann Thorac Surg [Internet]. 1994 Jan;57(1):12–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/0003497594903581.
|
| 17. |
Edwards FH, Grover FL, Shroyer ALW, Schwartz M, Bero J. The Society of Thoracic Surgeons National Cardiac Surgery Database: Current Risk Assessment. Ann Thorac Surg [Internet]. 1997 Mar;63(3):903–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0003497597000179.
|
| 18. |
Moran JL, Peisach AR, Solomon PJ, Martin J. Cost Calculation and Prediction in Adult Intensive Care: A Ground-up Utilization Study. Anaesth Intensive Care [Internet]. 2004 Dec 14;32(6):787–97. Available from: http://journals.sagepub.com/doi/10.1177/0310057X0403200610.
|
| 19. |
Cheng DCH, Karski J, Peniston C, Raveendran G, Asokumar B, Carroll J, et al. Early Tracheal Extubation after Coronary Artery Bypass Graft Surgery Reduces Costs and Improves Resource Use. Anesthesiology [Internet]. 1996 Dec 1;85(6):1300-1310. Available from: https://pubs.asahq.org/anesthesiology/article/85/6/1300/35963/Early-Tracheal-Extubation-after-Coronary-Artery.
|
| 20. |
Rossaint R, Slama K, Jaeger M, Konrad M, Pappert D. Fluid restriction and early extubation for successful liver transplantation. In: Transplantation proceedings. 1990. p. 1533–4.
|
| 21. |
Mandell MS, Lockrem J, Kelley SD. Immediate Tracheal Extubation After Liver Transplantation: Experience of Two Transplant Centers. Anesth Analg [Internet]. 1997;84(2). Available from: https://journals.lww.com/anesthesia-analgesia/Fulltext/1997/02000/Immediate_Tracheal_Extubation_After_Liver.3.aspx.
|
| 22. |
Mandell MS, Lockrem J, Kelley SD. Immediate Tracheal Extubation After Liver Transplantation: Experience of Two Transplant Centers. Surv Anesthesiol [Internet]. 1998;42(1). Available from: https://journals.lww.com/surveyanesthesiology/Fulltext/1998/02000/Immediate_Tracheal_Extubation_After_Liver.18.aspx.
|
| 23. |
Neelakanta G, Sopher M, Chan S, Pregler J, Steadman R, Braunfeld M, et al. Early tracheal extubation after liver transplantation. J Cardiothorac Vasc Anesth [Internet]. 1997;11(2):165–7. Available from: https://www.sciencedirect.com/science/article/pii/S105307709790207X.
|
| 24. |
Plevak DJ, Torsher LC. Fast tracking in liver transplantation. Liver Transplant Surg [Internet]. 1997 Jul;3(4):447–8. Available from: https://onlinelibrary.wiley.com/doi/10.1002/lt.500030419.
|
| 25. |
Zhu F, Lee A, Chee Y. Fast‐track cardiac care for adult cardiac surgical patients. Cochrane Database Syst Rev [Internet]. 2012;10. Available from: https://www.annals.in/text.asp?2010/13/2/92/62930.
|
| 26. |
Mittnacht AJC, Hollinger I. Fast-tracking in pediatric cardiac surgery-the current standing. Ann Card Anaesth [Internet]. 2010;13(2):92. Available from: https://www.annals.in/text.asp?2010/13/2/92/62930.
|
| 27. |
Wong W-T, Lai VK, Chee YE, Lee A. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst Rev [Internet]. 2016 Sep 12;2016(9). Available from: http://doi.wiley.com/10.1002/14651858.CD003587.pub3.
|
| 28. |
Aniskevich S. Fast track anesthesia for liver transplantation: Review of the current practice. World J Hepatol [Internet]. 2015;7(20):2303. Available from: http://www.wjgnet.com/1948-5182/full/v7/i20/2303.htm.
|
| 29. |
Gravlee GP. On aging, fast-tracking, and derailment in CABG patients. J Cardiothorac Vasc Anesth [Internet]. 1998 Aug;12(4):379–80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9713721.
|
| 30. |
London MJ, Shroyer LA, Coll JR, MaWhinney S, Fullerton DA, Hammermeister KE, et al. Early Extubation following Cardiac Surgery in a Veterans Population. Anesthesiology [Internet]. 1998 Jun 1;88(6):1447–58. Available from: https://pubs.asahq.org/anesthesiology/article/88/6/1447/36924/Early-Extubation-following-Cardiac-Surgery-in-a.
|
| 31. |
London MJ, Shroyer LA, Coll JR, MaWhinney S, Fullerton DA, Hammermeister KE, et al. Early Extubation Following Cardiac Surgery in a Veterans Population. Surv Anesthesiol [Internet]. 1999;43(3). Available from: https://journals.lww.com/surveyanesthesiology/Fulltext/1999/06000/Early_Extubation_Following_Cardiac_Surgery_in_a.4.aspx.
|
| 32. |
Higgins TL. Safety issues regarding early extubation after coronary artery bypass surgery. J Cardiothorac Vasc Anesth [Internet]. 1995 Oct;9(5 Suppl 1):24–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8562899.
|
| 33. |
Guller U, Anstrom KJ, Holman WL, Allman RM, Sansom M, Peterson ED. Outcomes of early extubation after bypass surgery in the elderly. Ann Thorac Surg [Internet]. 2004 Mar;77(3):781–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0003497503019015.
|
| 34. |
Kotfis K, Szylińska A, Listewnik M, Lechowicz K, Kosiorowska M, Drożdżal S, et al. Balancing intubation time with postoperative risk in cardiac surgery patients – a retrospective cohort analysis. Ther Clin Risk Manag [Internet]. 2018 Nov;Volume 14:2203–12. Available from: https://www.dovepress.com/balancing-intubation-time-with-postoperative-risk-in-cardiac-surgery-p-peer-reviewed-article-TCRM.
|
| 35. |
Walthall H, Robson D, Ray S. Do any preoperative variables affect extubation time after coronary artery bypass graft surgery? Hear Lung [Internet]. 2001 May;30(3):216–24. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0147956301125641.
|
| 36. |
Bansal S, Thai HM, Hsu CH, Sai-Sudhakar CB, Goldman S, Rhenman BE. Fast Track Extubation Post Coronary Artery Bypass Graft: A Retrospective Review of Predictors of Clinical Outcomes. World J Cardiovasc Surg [Internet]. 2013;03(02):81–6. Available from: http://www.scirp.org/journal/doi.aspx?DOI=10.4236/wjcs.2013.32014.
|
| 37. |
Hiromoto A, Maeda M, Murata T, Shirakawa M, Okamoto J, Maruyama Y, et al. Early extubation in current valve surgery requiring long cardiopulmonary bypass: Benefits and predictive value of preoperative spirometry. Hear Lung [Internet]. 2020 Nov;49(6):709–15. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0147956320303137.
|
| 38. |
Quiroga M, Rodríguez MG, Montalván C, Abarca J, Viñuela M, Cavallieri S, et al. Trends in mechanical ventilation and immediate extubation after liver transplantation in a single center in Chile. Transplant Proc [Internet]. 2004 Jul;36(6):1683–4. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0041134504007493.
|
| 39. |
Taner CB, Willingham DL, Bulatao IG, Shine TS, Peiris P, Torp KD, et al. Is a mandatory intensive care unit stay needed after liver transplantation? Feasibility of fast-tracking to the surgical ward after liver transplantation. Liver Transplant [Internet]. 2012 Mar;18(3):361–9. Available from: https://onlinelibrary.wiley.com/doi/10.1002/lt.22459.
|
| 40. |
Wu J, Rastogi V, Zheng S-S. Clinical practice of early extubation after liver transplantation. Hepatobiliary Pancreat Dis Int [Internet]. 2012 Dec;11(6):577–85. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1499387212602288.
|
| 41. |
Glanemann M, Langrehr J, Kaisers U, Schenk R, Müller A, Stange B, et al. Postoperative tracheal extubation after orthotopic liver transplantation. Acta Anaesthesiol Scand [Internet]. 2001 Mar;45(3):333–9. Available from: http://doi.wiley.com/10.1034/j.1399-6576.2001.045003333.x.
|
| 42. |
Barash PG, Lescovich F, D. Katz J, Talner NS, Stansel HC. Early Extubation Following Pediatric Cardiothoracic Operation: A Viable Alternative. Ann Thorac Surg [Internet]. 1980;29(3):228–33. Available from: https://www.sciencedirect.com/science/article/pii/S0003497510618723.
|
| 43. |
Heard GG, Lamberti JJ, Park SM, Waldman JD, Waldman J. Early extubation after surgical repair of congenital heart disease. Crit Care Med [Internet]. 1985;13(10):830–2. Available from: http://europepmc.org/abstract/MED/4028752.
|
| 44. |
Cheng DCH, Karski J, Peniston C, Asokumar B, Raveendran G, Carroll J, et al. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: A prospective randomized controlled trial. J Thorac Cardiovasc Surg [Internet]. 1996;112(3):755–64. Available from: https://www.sciencedirect.com/science/article/pii/S0022522396700624.
|
| 45. |
Neirotti RA, Jones D, Hackbarth R, Paxson Fosse G. Early extubation in congenital heart surgery. Hear Lung Circ [Internet]. 2002;11(3):157–61. Available from: https://www.sciencedirect.com/science/article/pii/S1443950602901411.
|
| 46. |
Vricella LA, Dearani JA, Gundry SR, Razzouk AJ, Brauer SD, Bailey LL. Ultra fast track in elective congenital cardiac surgery. Ann Thorac Surg [Internet]. 2000;69(3):865–71. Available from: https://www.sciencedirect.com/science/article/pii/S0003497599013065.
|
| 47. |
Mittnacht AJC, Thanjan M, Srivastava S, Joashi U, Bodian C, Hossain S, et al. Extubation in the operating room after congenital heart surgery in children. J Thorac Cardiovasc Surg [Internet]. 2008;136(1):88–93. Available from: https://www.sciencedirect.com/science/article/pii/S0022522307020338.
|
| 48. |
Totonchi Z, Azarfarin R, Jafari L, Alizadeh Ghavidel A, Baharestani B, Alizadehasl A, et al. Feasibility of On-table Extubation After Cardiac Surgery with Cardiopulmonary Bypass: A Randomized Clinical Trial. Anesthesiol Pain Med [Internet]. 2018 Sep 24;In Press(In Press). Available from: https://brief.land/aapm/articles/80158.html.
|
| 49. |
Sullivan BL. Con: Early Extubation in the Operating Room Following Cardiac Surgery. Semin Cardiothorac Vasc Anesth [Internet]. 2012 Jul 22;16(4):187–9. Available from: https://doi.org/10.1177/1089253212452343.
|
| 50. |
Serrano N, García C, Villegas J, Huidobro S, Henry CC, Santacreu R, et al. Prolonged Intubation Rates After Coronary Artery Bypass Surgery and ICU Risk Stratification Score. Chest [Internet]. 2005;128(2):595–601. Available from: https://www.sciencedirect.com/science/article/pii/S0012369215504017.
|
| 51. |
Singh KE, Baum VC. Pro: Early Extubation in the Operating Room Following Cardiac Surgery in Adults. Semin Cardiothorac Vasc Anesth [Internet]. 2012 Jul 13;16(4):182–6. Available from: https://doi.org/10.1177/1089253212451150.
|
| 52. |
Bainbridge D, Cheng D. Current evidence on fast track cardiac recovery management. Eur Hear J Suppl [Internet]. 2017 Jan 1;19(suppl_A):A3–7. Available from: https://doi.org/10.1093/eurheartj/suw053.
|
| 53. |
Meade MO, Guyatt G, Butler R, Elms B, Hand L, Ingram A, et al. Trials Comparing Early vs Late Extubation Following Cardiovascular Surgery. Chest [Internet]. 2001;120(6, Supplement):445S-453S. Available from: https://www.sciencedirect.com/science/article/pii/S0012369215500020.
|
| 54. |
Ellis MF, Pena H, Cadavero A, Farrell D, Kettle M, Kaatz AR, et al. Reducing Intubation Time in Adult Cardiothoracic Surgery Patients With a Fast-track Extubation Protocol. Crit Care Nurse [Internet]. 2021 Jun 1;41(3):14–24. Available from: https://doi.org/10.4037/ccn2021189.
|
| 55. |
Mirinejad M, Azarfarin R, Asl AA. Cisatracurium in cardiac surgery - continuous infusion vs. bolus administration. Middle East J Anaesthesiol [Internet]. 2007;19(3):563–72. Available from: http://europepmc.org/abstract/MED/18044284.
|
| 56. |
Svircevic V, Nierich AP, Moons KGM, Brandon Bravo Bruinsma GJ, Kalkman CJ, van Dijk D. Fast-Track Anesthesia and Cardiac Surgery: A Retrospective Cohort Study of 7989 Patients. Anesth Analg [Internet]. 2009;108(3). Available from: https://journals.lww.com/anesthesia-analgesia/Fulltext/2009/03000/Fast_Track_Anesthesia_and_Cardiac_Surgery__A.12.aspx.
|
| 57. |
Iezzi F, di Summa M, Del Sarto P, Munene J. Fast-Track Extubation in Pediatric Cardiothoracic Surgery in Developing Countries. J Card Crit Care TSS [Internet]. 2017 Aug 29;01(01):021–3. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0037-1604334.
|
| 58. |
Bajwa SJS, Kaur J, Khanna M. Changing anesthesia trends in cardiothoracic surgeries: A fast changing perspective. Anaesthesia, Pain Intensive Care [Internet]. 2016;20. Available from: http://www.apicareonline.com/wordpress/wp-content/uploads/2016/Oct/25A==RA-Changing anaesthesia trends in cardiothoracic surgeries-1.pdf.
|
| 59. |
van Mastrigt GAPG, Joore MA, Nieman FHM, Severens JL, Maessen JG. Health-related quality of life after fast-track treatment results from a randomized controlled clinical equivalence trial. Qual Life Res [Internet]. 2010;19(5):631–42. Available from: https://doi.org/10.1007/s11136-010-9625-5.
|
| 60. |
Hawkes CA, Dhileepan S, Foxcroft DR. Early extubation for adult cardiac surgical patients. Cochrane Database Syst Rev [Internet]. 2003;(4). Available from: https://doi.org//10.1002/14651858.CD003587.
|
| 61. |
El Solh AA, Aquilina A, Pineda L, Dhanvantri V, Grant B, Bouquin P. Noninvasive ventilation for prevention of post-extubation respiratory failure in obese patients. Eur Respir J [Internet]. 2006 Sep 1;28(3):588 LP – 595. Available from: http://erj.ersjournals.com/content/28/3/588.abstract.
|
| 62. |
Parlow JL, Ahn R, Milne B. Ľobésité est un facteur de risque ďéchec de ľextubation «précoce» à la suite ďun pontage aortocoronarien. Can J Anesth [Internet]. 2006;53(3):288–94. Available from: https://doi.org/10.1007/BF03022217.
|
| 63. |
Butler J, Chong GL, Pillai R, Westaby S, Rocker GM. Early extubation after coronary artery bypass surgery: effects on oxygen flux and haemodynamic variables. J Cardiovasc Surg (Torino) [Internet]. 1992;33(3):276–80. Available from: http://europepmc.org/abstract/MED/1601908.
|