Abstract
Background
The objective of this study was to evaluate the effectiveness of a biocide-based disinfectant against pathogenic flora on the skin of the hands.
Methods
This is a prospective study of 30 participants from the general population. The questionnaire, interview data and results of two swab analysis were collected. All the data were statistically analyzed.
Results
The results demonstrated that after using a biocide-based disinfectant, the number of bacteria colonies on the participants’ skin decreased or completely disappeared, and a significant correlation was found between the number of colonies before and after disinfection. In case of coagulase–negative staphylococcus the number of colony – forming units (CFU) significantly decreased [p < 0,001]. Also, Bacillus ssp. and Acinetobacter spp. were also found in 17.6% (n = 3) of the participants after the disinfection, however the number of the colonies was significantly smaller [p = 0,001; p = 0,008].
Conclusions
Our study demonstrates that a biocide-based disinfectant has high effectiveness against Gram-positive, Gram-negative, as well as fungal pathogens.
Citation
Viktorovs V, Romanova A, Azina I, Rozentale B. Efficacy of biocide-based sanitizer in daily use during the COVID-19 pandemic. Eur J Transl Clin Med. 2022;5(1):71-76Introduction
Biocides are chemical substances intended to kill or limit the growth of bacteria, fungi and viruses. Biocides are used worldwide as antimicrobials which can further be divided into oxidizing and non-oxidizing subtypes. The main difference between these two groups is a mechanism of action and activity against microorganisms. Oxidizing biocides tend to attack microorganisms by oxidizing cell structures causing an electron transfer reaction which then doesn't allow nutrients to cross the cell wall. The other type of the biocide action is a non-oxidizing pathway in which the microorganism’s respiratory reproductive processes are interrupted, in addition to damaging the cell wall [1-2].
Several factors can affect the activity of a biocide, e.g. pH, concentration, duration of exposure and temperature. Biocides can be divided in four groups. The first biocide group includes biocide-based disinfectants which are safe for humans or animals and are commonly used in public and private spaces or to disinfect food and water. The second group are preservatives which prevent bacteria biofilm formation and feeding on the organic plasticisers. Finally, there are pesticides and other selective biocides [3].
Disinfectant effectiveness is as important as skin health using disinfectants on daily basis. According to the National Health Service of the United Kingdom, one of the main causes for irritant contact dermatitis are disinfectants and antiseptics [4]. However, according to Slotosch et al., alcohol-based disinfectants are not the primary cause of irritant contact dermatitis. Instead, alcohol based disinfectants sting already damaged skin and develop first signs of the skin disease. In the ongoing COVID-19 pandemic, skin disinfection has become an element of our daily routine, which leads to development of different types of skin damage. Thus, disinfectants need to be equally effective and safe for the skin [5].
Material and methods
This is a prospective cross-sectional study. We collected data from 30 participants (n = 30). The eligibility criteria were age (> 18 years old), no history of active or acute contact dermatitis, hand eczema or other acute hand skin condition. The trial was performed in two centers: Jurmala Hospital (Jurmala, Latvia) and a private clinic in Riga, Latvia. We tested a biocide-based hand sanitizer gel, which contained Alkyl (C12-C16) Dimethylbenzylammoniumchloride (0,2%) and unknown concentrations of Aloe-Vera and D-panthenol.
To test action and effectiveness of the sanitizer we performed a microbiological analysis in accordance with the EN 1500 standard (a European Standard test method used to evaluate the efficacy of hand sanitizers and hand rubs). Microbiological swabs were taken from 5 cm x 5 cm large palmar and dorsal hand surfaces from one hand using the “Cliniswab TS” and the same technique was used to all participants. After the first swab, 5 ml of the tested hand sanitizer was placed on the participants’ skin using a pipette. Next, the participants disinfected their hands for 30 seconds and after finishing disinfection, the investigator waited for 30 seconds to take second swab (the exposition time to the disinfectant was 30 seconds). The sanitizer was dosed using a pipette and the same amount of the disinfector (5 ml) was placed to the participant’s skin. The participants disinfected their hands in accordance with the World Health Organization (WHO) recommendations: hands palm to palm, then left palm over right dorsum with interlaced fingers, continued with palm to palm with fingers interlaced, then backs of fingers to opposite palms with fingers interlocked, continued with rotational rubbing of left thumb clasped in right palm, then rotation rubbing, backwards and forwards with clasped fingers of right hand in left palm [6]. The hand disinfectant covered the entire hand surface.
Before taking the second swab, the participants’ hand surface was completely dry. After the exposition time, investigators repeated the microbiological swab from palmar and dorsal hand surfaces. All samoles were stored in room temperature (+23°C) and transported to the same clinically-accredited microbiological laboratory for culture and analysis.
For statistical analysis, the SPSS v.23 was used (IBM, Armonk, USA). Parametric statistical tests (Student’s t-test, ANOVA) were used to evaluate the microbiological culture results. Written informed consent was obtained from all the study participants before enrolment into the study. The Ethics Committee of the Faculty of Medicine at the University of Latvia approved the study protocol.
Results
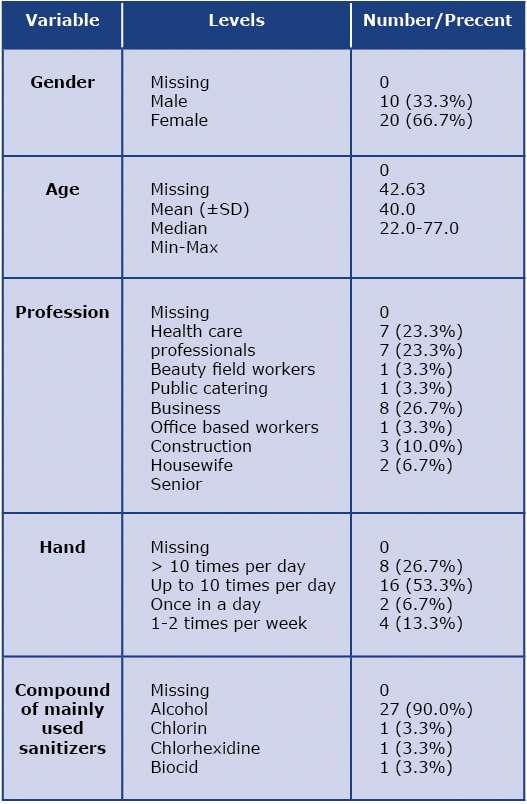
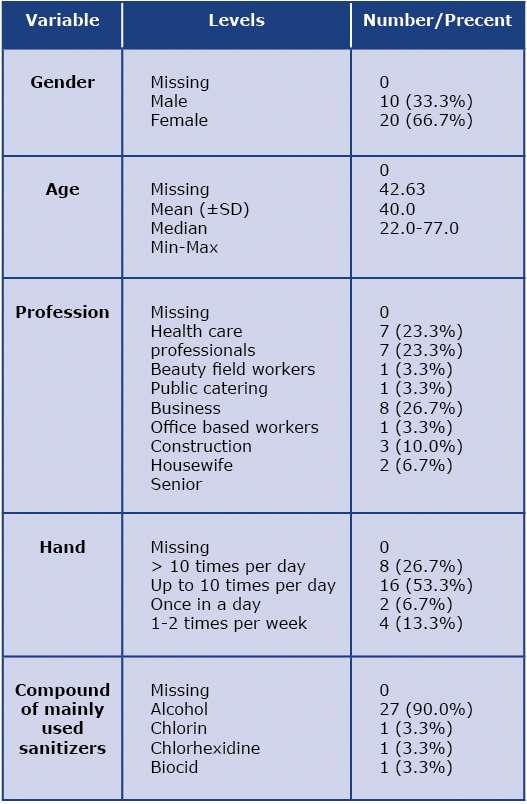
Table 1 illustrates demographic data of the trial population and hand disinfection habits. The study included data of 30 participants, of whom 66.7% (n = 20) were women. Majority of the participants were 40-49 years of age (n = 11) and reported that they disinfected their hands up to 10 times per day (36.6%, n = 8). An important data was collected about a type of an occupation. The field of work correlated with the frequency of hand disinfection on a daily basis. In majority of cases (66.7%, n = 20) the frequency of daily hand disinfection was influenced by work. Nearly the same number of participants worked in offices as in health care (respectively 26.7%, n = 8 vs 23.0%, n = 7) and 23.0% (n = 7) worked in the beauty industry. Participants expressed their opinion about the importance of basic chemicals contained in hand sanitizers and their influence on skin after frequent use. 98.7% (n = 29) of the participants stated that since the start of winter and the pandemic, they are using hand sanitizers everyday and 90.0% (n = 27) used alcohol-based sanitizer. Only one participant reported using a biocide-based hand sanitizer (Table 1).
Table 1. Socio – demographic characteristic of trial population
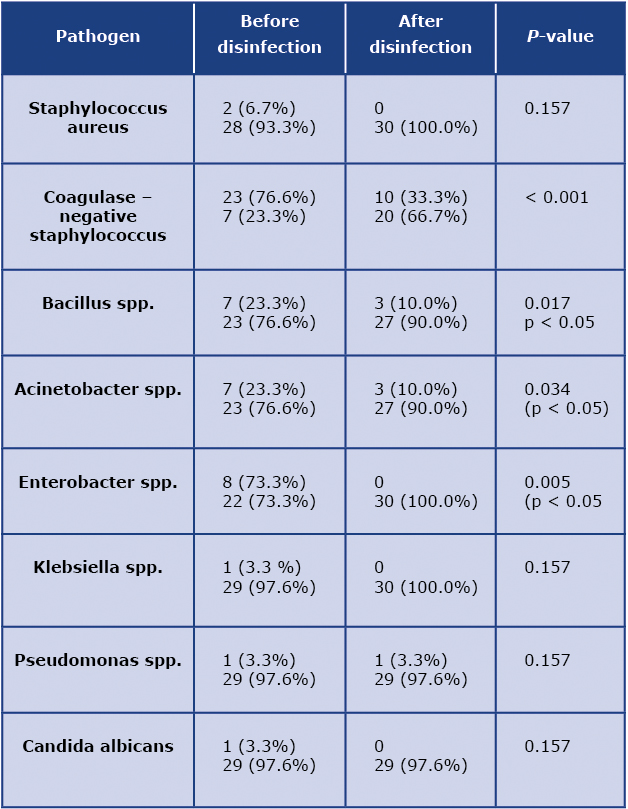
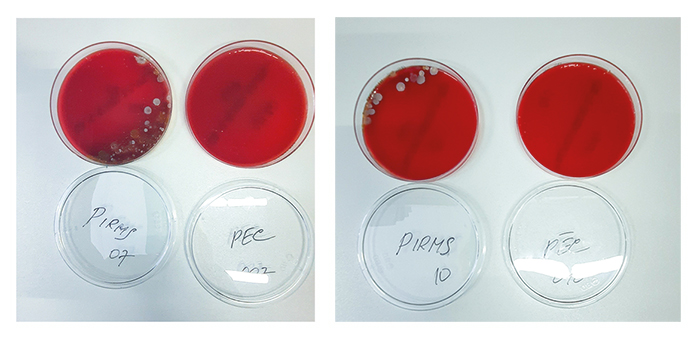
Microbiological cultures of the first swabs (before hand disinfection) were positive for coagulase-negative staphylococcus (CoNS, 46.0%, n = 23), Bacillus spp. (14.0%, n = 7), Acinetobacter spp. (14.0%, n = 7) and Enterobacter spp. in (16.0%, n = 8). Among the less commonly noted species were Staphylococcus aureus (4.0%) and Klebsiella spp., Pseudomonas spp. and Candida albicans (2.0% each). Whereas the cultures from the second swabs (after hand disinfection), significantly less microorganism colonies were detected. In 10 cases (58.8%) CoNS was still noted, however with significantly fewer colony-forming units (CFUs) [p < 0,001]. Also Bacillus spp. and Acinetobacter spp. were found in 17.6% (n = 3) of all cases [p = 0,001; p = 0,008], and similar to CoNS, the number of CFUs decreased (Table 2, Figure 1).
Table 2. Effectiveness of biocide based hand sanitizer is proven by colonies changes before and after disinfection
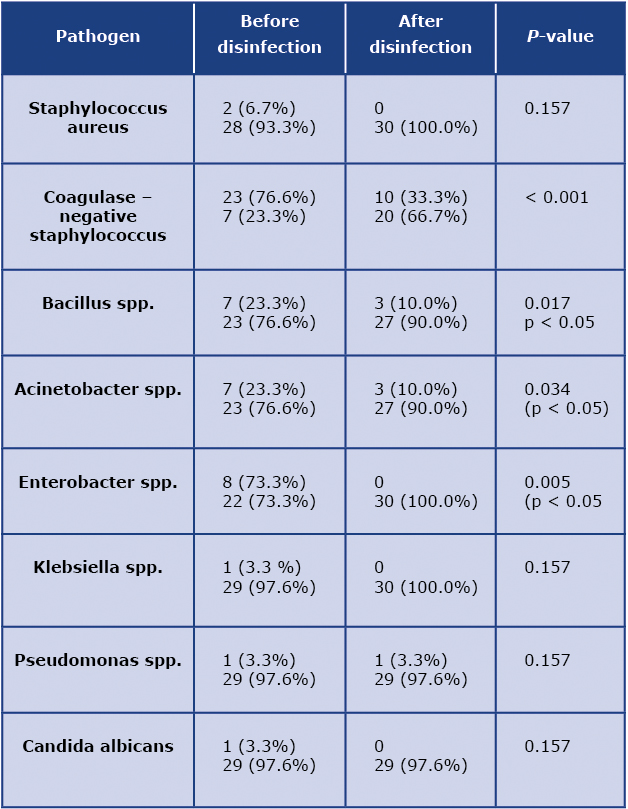
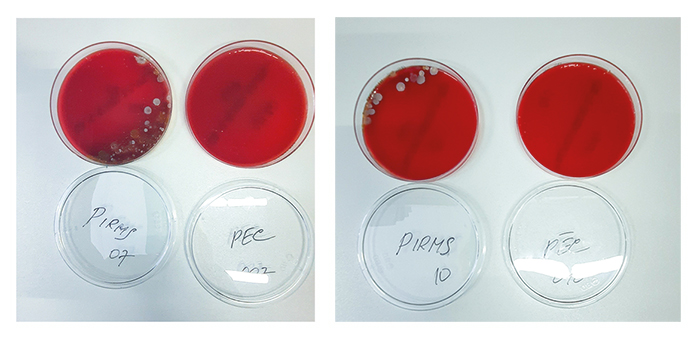
Fig. 1 (a) Colonies detected before hand disinfection in swab from a patient Nr 7; (b) Colonies detected after hand disinfection in swab from a patient Nr. 7. (c) Colonies detected before hand disinfection in swab from a patient Nr. 10; d) Colonies detected after hand disinfection in swab from a patient Nr. 10.
Discussion
In Majority of cases colonies of pathogenic microorganisms were either completely removed or there was a significantly decreased amount of CFUs. According to the literature the total bacteria count on hand surfaces of normal human skin ranges from 3.9 × 104 to 4.6 × 106 CFU/cm2 [7-10]. Hand disinfection is an important step in the prevention of infections and complicated diseases. One of the most common bacteria appearing in similar trials was CoNS (76.7% of cases). This gram-positive microorganism is a part of normal human skin flora but in some cases it can cause potentially life-threatening complications and infections, e.g. endocarditis, peritonitis, as well as complicated skin infections [11-13]. The commonly detected bacteria in our study were Bacillus spp. which is an aerobic or facultative anaerobic, endospore-forming, usually Gram-positive bacteria which can cause a wide range of infections including abscesses, bacteremia/septicemia, wound and burn infections, ear infections, endocarditis, meningitis, ophthalmitis, osteomyelitis, peritonitis and even cutaneous anthrax and a major risk factor is contact with animals [14-15].
We noted similar results about Acinetobacter spp. and Pseudomonas spp. Acinetobacter spp which are saprophytic organisms that can live in soil, water and food. Acinetobacter spp. is a Gram-negative, strictly aerobic bacteria. Frequently, these bacteria colonize the oral cavity, respiratory tract and gastrointestinal tract. Acinetobacter spp. very often cause nosocomial infections, mainly infections of blood, urinary tract, skin infections including wound infections, pneumonias and meningitis. Similar to Acinetobacter spp., Pseudomonas spp. also belong to Gram-negative bacteria. Under huge risk for Pseudomonas spp. infection development are immunosuppressive patients and cancer patients [16-17]. According our trial data, number of CFU decreased after skin disinfection with the biocide based skin sanitizer.
After disinfection the following colonies completely disappeared: Klebsiella spp., Enterobacter spp. and Candida albicans. Klebsiella spp. is Gram-negative rod shaped anaerobic bacteria. Klebsiella spp. cause urinary tract infections, as well as wound and skin infections and respiratory tract infections. Similar to Klebsiella spp., Enterobacter spp. belong to Gram-negative bacteria, theses bacteria can be isolated from water, soil, commensals. This bacteria is now emerging a pathogenic, under the risk are immunocompromised patients [18]. An opportunistic fungal pathogen was detected in our study: Candida albicans. This fungus has ability to colonize in almost all human body tissue and organ, which can cause serious and complicated infections [18]. In all the cases, when these three pathogens were detected before disinfection, after using the biocide-based disinfection all of the three were entirely killed and absent on hand skin surface.
During the COVID-19 pandemic hand disinfection became a part of many people’s daily routine. The main reason for choosing alcohol-based skin disinfectant is the cliché belief that ethanol is effective against most of microorganisms and viruses, despite the fact that ethanol has a negative in fluence on skin condition. Majority of our trial participants noted that after the use of the ethanol disinfectant, they feel dryness, itchiness and irritation on the surfaces of their hands. Additionally, there is a little research about alcohol’s influence on skin, however some sources report that allergic contact dermatitis to alcohol-based antiseptics is uncommon. The main ingredients in alcohol-based hand rubs are n-propanol and/or isopropanol. A systemic review showed that in majority of studies in the period from 2000 to 2019 n-propanol and isopropanol in different concentration were related to irritation. N-propanol caused significant skin barrier damage, however, studies showed that n-propanol alone has low irritation potential [19]. Most common local skin allergic reaction to alcohol-based formulations is a sign of allergy against an impurity or an aldehyde metabolite. An immediate allergic is mostly caused by ethanol or isopropanol, but Irritant contact dermatitis mostly is caused by chemical or physical agents and it increases with the duration, intensity and concentration of the substance [6, 20-22].
Use of the biocide-based gel disinfectant with Aloe Vera and D-panthenol, does not irritate or damage skin. Our trial proves that a biocide based disinfectant has high effectiveness against Gram positive, Gram negative, as well as fungal pathogens, and even more protects skin from developing allergic reactions and worsening of chronic skin diseases.
On the other hand, our study has some limitations due to the small amount of participants included. However, the study was performed in two centers in different cities, with randomly selected participants. Nevertheless, conventional microbiology methods have some limitations in detecting microorganisms. Microscopy with staining and detection of cultures allows identifying only a limited number of colonies and could not recognize the full spectrum of microbiota of human skin. For further investigation it will valuable to use polymerase chain reaction (PCR) and conduct a trial in a multiple medical centers and hospital departments. Unfortunately, in this study we did not test the biocide-based sanitizers’ efficacy against viruses, such as SARS-CoV-2 (causative pathogen of the COVID-19 disease). However, the United States Environmental Protection Agency (EPA) maintains a database of sanitizers which are effective against viruses, particularly SARS-CoV-2 [23]. This database contains information only about substances with proven efficacy and the criteria are as follows: substance is effective against SARS-CoV-2, demonstrates efficacy against any pathogen which is harder to kill than SARS-CoV-2 or shows efficacy to kill coronaviruses similar to SARS-CoV-2. Based on this database, the active substances of sanitizers with proven efficacy against SARS-CoV-2 or SARS-CoV-2-like viruses are: hydrogen peroxide, quaternary ammonium, tetraacetylethylenediamine, dodecylbenzenesulfonic acid and others.
Conclusions
Our study demonstrates that a biocide-based disinfectant has high effectiveness against Gram-positive, Gram-negative, as well as fungal pathogens. Further research should be done with the use of PCR and detection of viral particles to determine the significance of biocide use for all pathogens that can be transmitted through the skin directly or indirectly.
Conflict of interest
The authors do not have any conflicts of interests to report.
Funding
None.
Conflicts of interest
The authors do not have any conflicts of interests to report.
References
| 1. |
Tucker N. 6 - Clean production. In: Baillie C, Jayasinghe RBT-GC (Second E, editors. Woodhead Publishing Series in Composites Science and Engineering [Internet]. Woodhead Publishing; 2017. p. 95–121. Available from: https://www.sciencedirect.com/science/article/pii/B9780081007839000058.
|
| 2. |
Makhlouf ASH, Botello MA. Chapter 1 - Failure of the metallic structures due to microbiologically induced corrosion and the techniques for protection. In: Makhlouf ASH, Aliofkhazraei MBT-H of MFA, editors. Butterworth-Heinemann; 2018. p. 1–18. Available from: https://www.sciencedirect.com/science/article/pii/B978008101928300001X.
|
| 3. |
Michalak I, Chojnacka K. Biocides. In: Encyclopedia of Toxicology. Elsevier; 2014. p. 461–3.
|
| 4. |
Contact dermatitis - Causes - NHS [Internet]. [cited 2022 Apr 3]. Available from: https://www.nhs.uk/conditions/contact-dermatitis/causes/.
|
| 5. |
Slotosch CM, Kampf G, Löffler H. Effects of disinfectants and detergents on skin irritation. Contact Dermatitis [Internet]. 2007 Oct;57(4):235–41. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1600-0536.2007.01200.x.
|
| 6. |
World Health Organization. WHO guidelines on hand hygiene in health care: First Global Patient Safety Challenge Clean Care Is Safer Care [Internet]. Geneva: World Health Organization; 2009. Available from: https://apps.who.int/iris/bitstream/handle/10665/44102/978?sequence=1.
|
| 7. |
Price PB. The Bacteriology of Normal Skin; A New Quantitative Test Applied to a Study of the Bacterial Flora and the Disinfectant Action of Mechanical Cleansing. J Infect Dis [Internet]. 1938;63(3):301–18. Available from: http://www.jstor.org/stable/30088420.
|
| 8. |
Larson E. Effects of handwashing agent, handwashing frequency, and clinical area on hand flora. Am J Infect Control. 1984 Apr;12(2):76–82.
|
| 9. |
Maki DG. Control of colonization and transmission of pathogenic bacteria in the hospital. Ann Intern Med. 1978 Nov;89(5 Pt 2 Suppl):777–80.
|
| 10. |
Larson EL, Hughes CA, Pyrek JD, Sparks SM, Cagatay EU, Bartkus JM. Changes in bacterial flora associated with skin damage on hands of health care personnel. Am J Infect Control. 1998 Oct;26(5):513–21.
|
| 11. |
Baron S. Bacillus. In: Medical Microbiology [Internet]. University of Texas Medical Branch at Galveston; 1996. Available from: https://www.ncbi.nlm.nih.gov/books/NBK7627/.
|
| 12. |
Bissett L. Skin care: an essential component of hand hygiene and infection control. Br J Nurs. 2007 Sep;16(16):976–81.
|
| 13. |
Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014 Oct;27(4):870–926.
|
| 14. |
Du C, Webb C. 2.03 - Cellular Systems. In: Moo-Young MBT-CB (Second E, editor. Burlington: Academic Press; 2011. p. 11–23. Available from: https://www.sciencedirect.com/science/article/pii/B9780080885049000805.
|
| 15. |
Kämpfer P. Acinetobacter. In: Encyclopedia of food microbiology. Academic press; 2014. p. 11–7.
|
| 16. |
Baron S. Pseudomonas. In: Medical Microbiology. University of Texas Medical Branch at Galveston; 1996.
|
| 17. |
Buckle J. Infection. In: Clinical Aromatherapy [Internet]. Elsevier; 2003. Available from: https://linkinghub.elsevier.com/retrieve/pii/B9780443072369X50012.
|
| 18. |
Hernday AD, Noble SM, Mitrovich QM, Johnson AD. Genetics and molecular biology in Candida albicans. Methods Enzymol. 2010;470:737–58.
|
| 19. |
Tasar R, Wiegand C, Elsner P. How irritant are n‐propanol and isopropanol? – A systematic review. Contact Dermatitis [Internet]. 2021 Jan 11;84(1):1–14. Available from: https://onlinelibrary.wiley.com/doi/10.1111/cod.13722.
|
| 20. |
Ophaswongse S, Maibach HI. Alcohol dermatitis: allergic contact dermatitis and contact urticaria syndrome. A review. Contact Dermatitis. 1994 Jan;30(1):1–6.
|
| 21. |
Widmer AF. Replace hand washing with use of a waterless alcohol hand rub? Clin Infect Dis an Off Publ Infect Dis Soc Am. 2000 Jul;31(1):136–43.
|
| 22. |
Litchman G, Nair PA, Atwater AR, Bhutta BS. Contact Dermatitis [Internet]. StatPearls. 2022 [cited 2022 Apr 3]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459230/.
|
| 23. |
How does EPA know that the products on List N work on SARS-CoV-2? | US EPA [Internet]. [cited 2022 Apr 3]. Available from: https://www.epa.gov/coronavirus/how-does-epa-know-products-list-n-work-sars-cov-2.
|