Abstract
Background
The COVID-19 pandemic has forced the introduction of many changes into medical student education. The aim of the study was to evaluate medical students’ perceptions of a Pharmacology course delivered at a Polish medical university before and during the pandemic.
Materials and methods
A cross-sectional anonymous survey conducted among medical students.
Results
90 out 122 students participated in the study. The vast majority of students found pharmacology to be a difficult subject. The surveyed group of students preferred active methods of learning, including: teacher explanations (86.5%) and discussions (70.8%) during in-person classes, real-time student-teacher meetings via dedicated web-based platforms (73%) during online classes. Students most often described e-learning as interesting (58.9%) and timesaving (52.2%). Less than 30% described it as stressful, difficult, time-consuming and boring. The most commonly reported advantage was the possibility for students to adjust their pharmacology study-time to a more personalised schedule (82.5%). The main disadvantage included the loss of in-person face-to-face contact with the teacher (61.8%).
Conclusions
Overall, students held positive attitudes towards the new teaching format and adapted well to the new conditions. Modern innovations enabling medical students to continue their studies efficiently and effectively during the pandemic must be developed and introduced into practice.
Citation
Pawłowska I J, Pawłowski L, Krzyżaniak N, Kocić I. How to teach pharmacology to medical students during the COVID-19 pandemic?. Eur J Transl Clin Med. 2022;5(1):33-39Introduction
The World Health Organization’s (WHO) declaration of the coronavirus disease 2019 (COVID-19) outbreak as a pandemic had serious implications in all areas of human activity – health care systems, travel, employment etc. [1]. The spread of this virus also had significant consequences on higher education as universities were required to shift from in-person teaching to online education [2–6]. This new form of education had to be implemented immediately without any preparation from either the students or staff [7]. In Poland, the closure of all educational institutions, including universities, occurred in mid-March 2020, which was approximately halfway through the second semester of the academic year [8]. The closure of medical schools was considered particularly important, due to concerns around medical students being potential vectors for COVID-19 during their rotations between hospitals and health departments [9]. Thus, all courses taught within the Faculty of Medicine at Polish medical universities were shifted from the in-person modality to online.
Pharmacology is considered a core pre-clinical subject within the curriculum at the Medical University of Gdańsk. It is taught during the 3rd year of the medical studies and consists of 100 didactic hours comprising lectures, seminars and exercises. During this course, students gain basic knowledge about pharmacology, toxicology and prescribing medication. The classes are spread over two semesters and the course ends with a multiple-choice exam. From the beginning of the pandemic, all pharmacology classes, mid-semester exams, oral exams and the final exam were performed online. Since the change to the online modality, both the teaching and studying of pharmacology has been challenging for teachers and students. To achieve the highest standards of education the following methods were applied: individual consultations, classes conducted in real-time via specialised web-based platforms e.g. Zoom, self-directed work, teacher feedback and the delivery of pre-recorded materials. The examinations were held using the Moodle and Zoom platforms.
The aim of this study was to evaluate medical students’ perceptions of the delivery of the pharmacology course before and during the COVID-19 pandemic (academic year 2019/2020).
Material and methods
This was a cross-sectional survey that was distributed online (via Google Forms). Following the completion of the Pharmacology and Toxicology subject, medical students (from the English Division group) were asked to complete the survey. The link to the survey was made available to students on the online course learning portal, and each student was invited to provide their opinions on both the regular face-to-face and online pharmacology classes. In the introduction of the survey, it was explained that the obtained results will be used for practical and scientific purposes. Participation in the study was voluntary and the survey was anonymous. The respondents did not receive any incentives for participating in the research. The questionnaire was prepared in English and consisted of 12 items which were based on the authors’ didactic and research experience. A total of 11 questions were directly related to the examined problem and comprised: 6 multiple choice questions, 2 single answer questions, 2 VAS-scale questions and one open-ended question relating to students overall opinions on the e-learning format. The last question was related to the gender of the participants. The survey was conducted in June-July 2020.
Statistical Analysis
The responses for each question were collected and calculated (frequencies and percentages) using StatisticaTM (TIBCO Software Inc., Palo Alto, CA, USA). For the statistical analysis, the Chi-square test was applied to determine any correlation between the two selected variables, e.g. comparing difficulty of regular classes to that of e-learning (Statistica version 13).
Results
A total of 90 out of a possible 122 medical students participated in the study (response rate 73.8%), of whom 65.6% (n = 59) were female and 34.4% male (n = 31 male).
Perceived difficulty of subject
The first question concerned general information about the course. The intention of this question was to determine the perceived difficulty of pharmacology as a subject for the examined students. Overall, 71 students (78.9%) rated the subject ‘difficult’, 8 (8.9%) found it very difficult, 10 considered it to be ‘easy’ and no students rated it ‘very easy’. There were no statistically significant differences between the gender of the students and the perceived difficulty of the subject (p > 0.05).
Sources of information relied upon by students
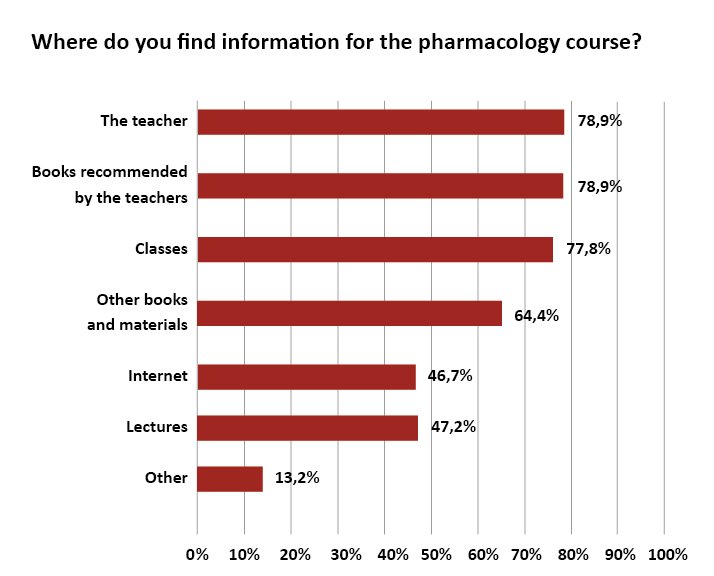
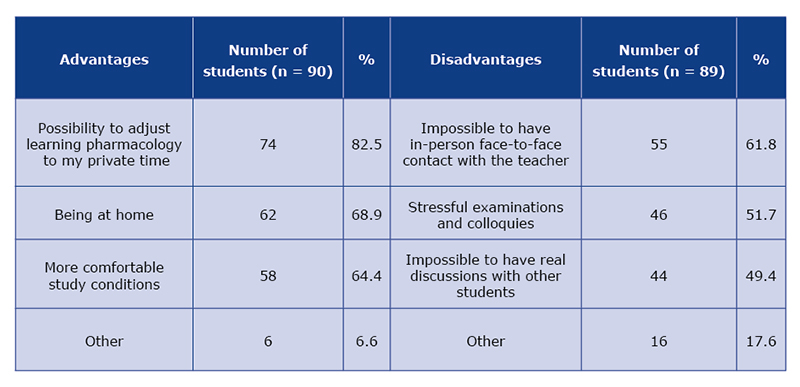
The most commonly identified sources of information relied on by students when studying the subject included: teachers, recommended books and classes. In their qualitative answers, 6 students listed the use of the Sketchy Pharmacology program (Fig. 1).
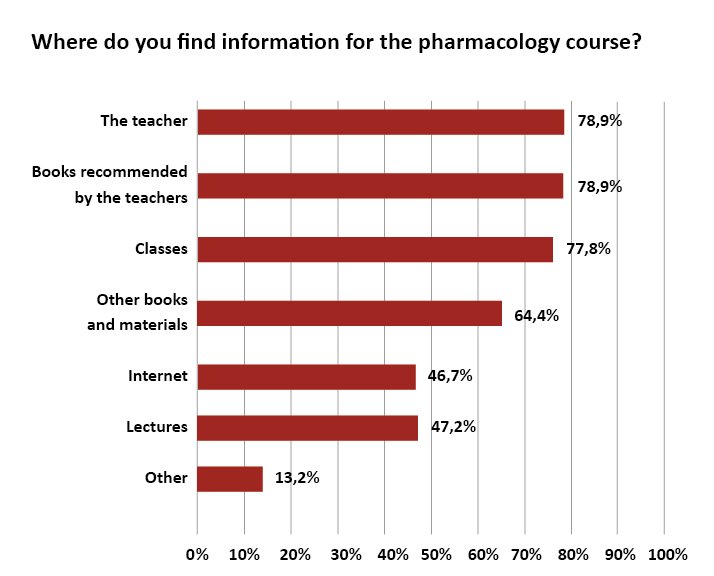
Figure 1. Sources of information used by students (several answers possible, n = 90)
Teaching practices utilised in the in-person and online teaching modalities
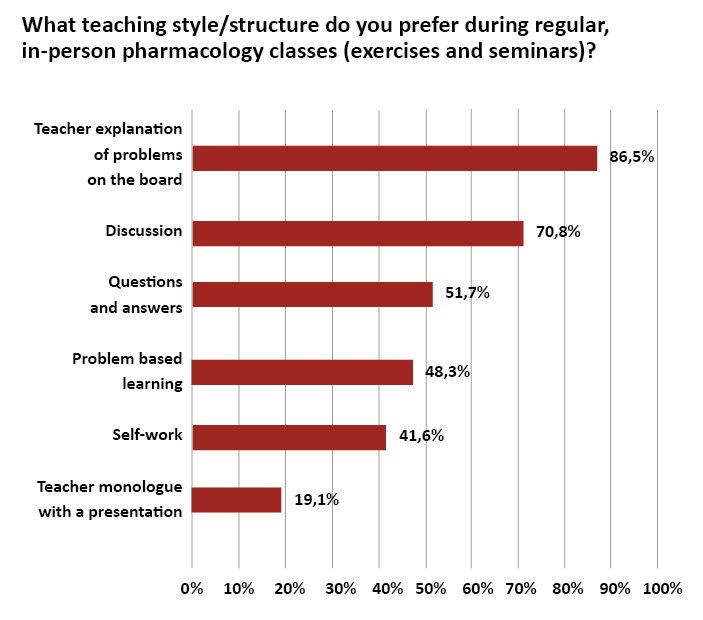
During the regular (pre-pandemic) classes various teaching methods were applied. Most students preferred active methods such as teacher explanations of problems on the white board (86.5%) and discussion (70.8%). Passive methods involving self-directed work (41.6%) and multimedia presentations (19.1%) were generally not considered to be interesting (Fig. 2).
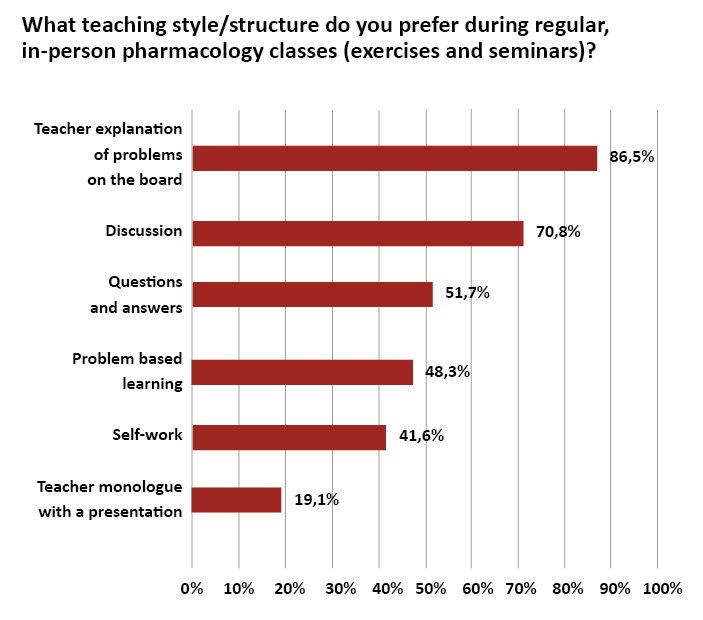
Figure 2. Students’ opinions on teaching methods applied during regular classes (n = 89)
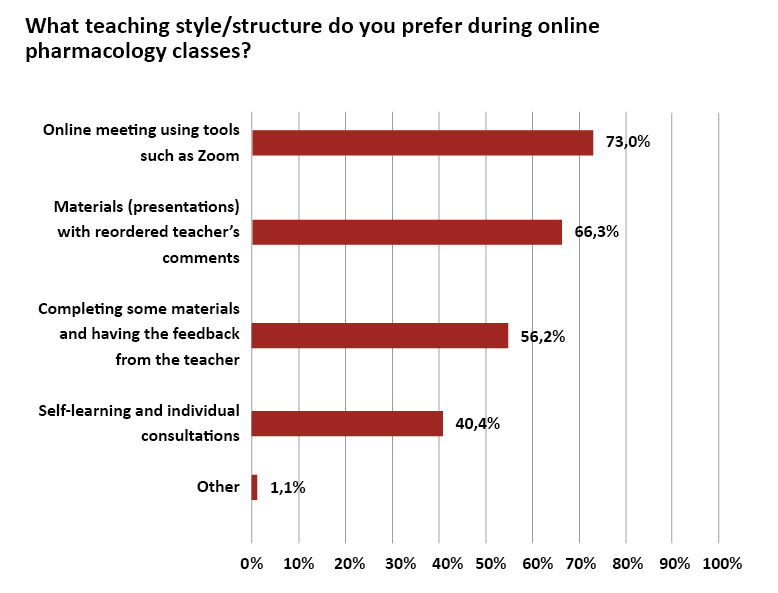
For online classes (during pandemic), teaching methods were modified and adjusted to the new circumstances. For the majority of students (73%) real-time meetings with the usage of special web-based communication software, e.g. Zoom, was considered the best teaching practice. Similarly, in comparison to the teaching-style/structure preferences of regular in-person classes, self-learning and individual consultations were favoured by less than half of participants (40.4%) (Fig. 3).
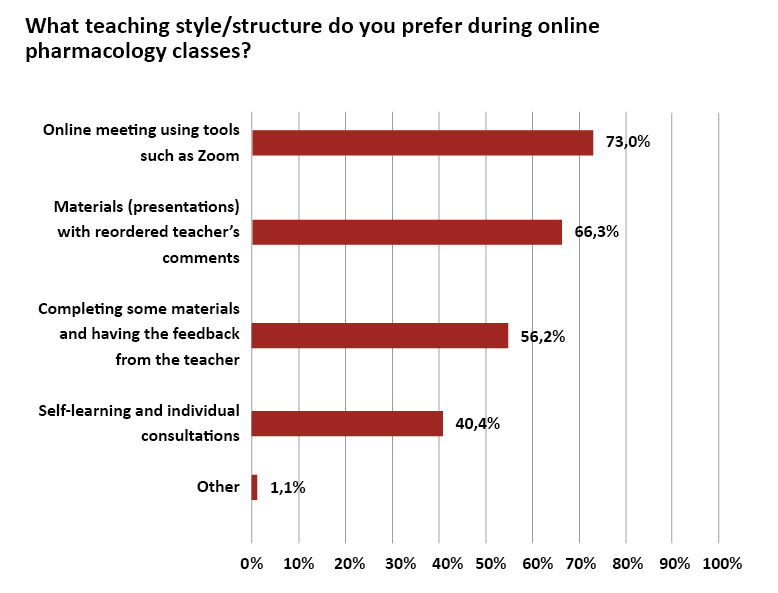
Figure 3. Students’ opinions on education methods applied during on-line classes (n = 89)
Student perceptions of e-learning
Students were asked to choose out of a selection of seven adjectives, which best described their perceptions of e-learning (several answers were possible). The students listed them in the following order: interesting (58.9%), time-saving (52.2%), stressful (27.8%), difficult (26.7%), time-consuming (21.1%), easy (14.4%) and boring (14.4%).
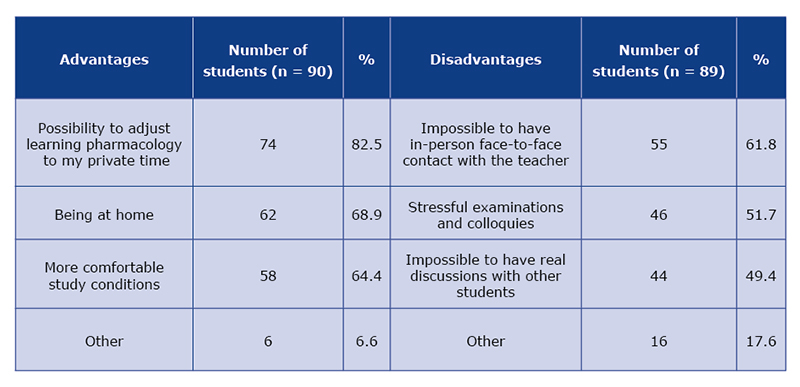
Students were also asked to describe the advantages and disadvantages of e-learning. The most commonly reported advantage related to the flexibility of the studying schedule. Students appreciated being able to adjust their pharmacology study-time to a more personalised timeframe (n = 74; 82.5%). On the other hand, the lack of in-person face-to-face contact with the teacher was the most commonly indicated disadvantage (n = 55; 61.2%). Other disadvantages included: increased stress due to having to do more studying alone, disruptions during class-time caused by family members, stress due to technical issues, perceived difficulties with student-teacher communication by e-mail and perceptions that they are learning less than what they would if they were attending normal classes in-person with the teacher. Two students reported no perceived advantages and a further two reported no perceived disadvantages (Table 1).
Table 1. Advantages and disadvantages of e-learning according to medical students
Student preferences for examinations
As far as the mid-semester tests and examinations are concerned, 84 out of 90 students (93.3%) preferred having a multiple choice question exam conducted on a virtual platform. Only a few students favoured undertaking an exam in an oral or written form.
Student perceptions of the difficulty of pharmacology learning based on the modality
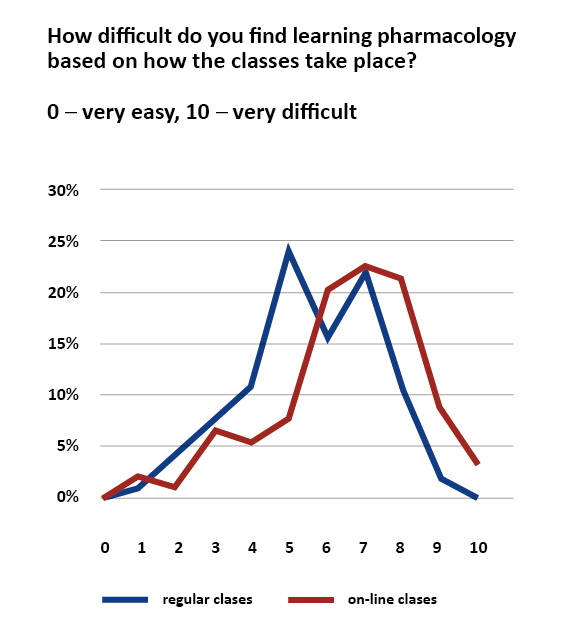
In the next pair of questions students were asked to assess the perceived level of difficulty in learning pharmacology based on the format in which it is delivered: in-person vs. online. A 10-point VAS scale was used with 0 indicating ‘very easy’ and 10 indicating ‘very difficult’. An overall range of 0-4 denoted 'easy’ and a range of 6-10 was ‘difficult’; 5 indicated the median, i.e. neither easy nor difficult. Overall, for the face-to-face format of teaching, 24.4% of students considered pharmacology to be easy and 51.1% found it difficult, with the remainder neutral (number 5). However, for the online classes, only 15.6% of students felt that learning pharmacology through a web-based format was easy and 76.4% found it difficult, the remaining 8% felt it was neither difficult nor easy. The mode answer value was calculated as 5 for regular classes (22 students, 24%) and 7 for online classes (20, 22.5%). For regular classes the mean was 5,6 and median 6, and in the case of face-to-face classes the values were 6,5 (mean) and 7 (median). The differences in the perceived levels of difficulty between the two formats was statistically significant (p = 0.03). The results are presented in Figure 4.
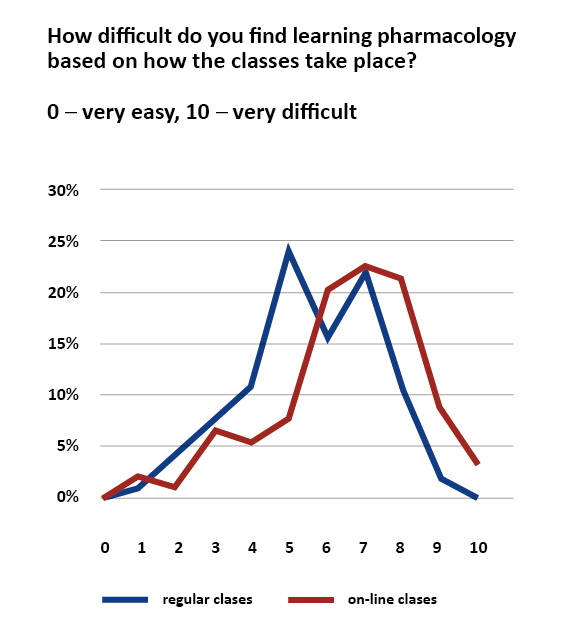
Figure 4. Students' opinions on level of difficulty of pharmacology classes based on how it is delivered: online vs. regular
Feedback from students
In the open-ended question students gave an overall evaluation of the online format of the classes. A total of 13 students reported that they were satisfied with e-learning and thanked the teachers for their good organization, and only two reported that they were dissatisfied, indicating that they preferred regular classes. A further nine students listed some improvements that could be made to the classes including better organization, less material to learn, better access to the information.
With reference to future classes, the majority of students (18) agreed that online meetings via a dedicated webbased platform (e.g. Zoom) were the best solution for conducting e-learning. Furthermore, 9 students indicated that pre-recorded lectures or seminars could be helpful in terms of allowing them to re-watch sessions, giving them the opportunity to learn the content at their own pace. A total of 12 students indicated that interactive discussions between teachers and students to solve case-based problems, as well as broader explanations of the material and interactive tasks, were essential for good e-learning. Individual work assignments and working in small groups was perceived as being beneficial for nine students.
Discussion
Our survey describes medical students’ perceptions of the differences in studying a pharmacology subject via two different modalities: e-learning during the COVID-19 pandemic vs. regular in-person classes. In general, the vast majority of surveyed students considered the pharmacology subject difficult. This indicates that students may have to put in a lot of effort to learn this subject.
Pharmacology is considered a cornerstone subject in tertiary education health science curricula [10]. Therefore, there is a growing need for the implementation of effective and efficient pharmacology education methods to obtain satisfactory learning outcomes. This challenge during the novel coronavirus pandemic took on a new form; since the start of the outbreak, the priority has been focused on ensuring the safety and well-being of students, patients and staff members. Thus, the universities were forced to introduce online learning, which required a prompt modification of the applied teaching methods and strategies.
When considering the teaching approaches, this study indicated that during face-to-face classes students favoured active forms involving both them and teachers. Similar answers were reported for online teaching – students singled out methods which mimic real-life meetings with teachers. i.e. live classes conducted on a platform that enabled direct communication. Furthermore, prescribed books as well the teachers’ own knowledge were considered the most relied upon resources whilst studying.
With respect to the examination methods, alarge number of students indicated that online tests with the usage of multiple-choice questions were the best tools for assessing knowledge. However, some students stressed that these examination formats may generate stress due to the potential for technical problems. Teachers from the King’s College London School of Medical Education proposed an open-book examination (OBE) instead of exam-hall settings, which was adopted by many schools [11]. Such approaches decrease student anxiety and may also have an impact on cheating and plagiarism.
The newly adopted online teaching format has many perceived advantages. Researchers from the UK claimed that the online classes allowed students to return to their homes and families where they felt more comfortable [11]. A study conducted among medical and surgery residents showed that this form of education is less time-consuming and therefore students could spend the time saved on reading academic journals, doing practice questions, completing other hospital work, working on research and volunteering [12]. Similar observations were made by medical students from the Kingdom of Saudi Arabia. Additionally, the authors agreed that online learning was more successful within basic medical sciences or preclinical subjects [13]. Moreover, online learning could decrease the absences of the students at the classes and reduce the pathologies related to their making up [14].
Other advantages listed by students in our survey included a flexible learning schedule as well as being able to study in a more comfortable setting at home. On the other hand, the major disadvantage was a lack of in-person contact with the teacher. Overall, students found online learning interesting and time-saving however, also perceived some aspects of it to be difficult. Similar results were found by researches from another Polish medical university. Medical students most frequently indicated the following advantages: access to online materials, learning on their own peace, ability to stay at home and comfortable surroundings. For these students the technical problems, lack of interactions with patients and decreased interaction with the teacher were the most common disadvantages [15].
A study of 1255 health care students from various countries, showed that positive perceptions and prior experiences of e-learning are closely related to the level of country development. The researchers also claimed that e-learning was more effective in acquiring theoretical knowledge in comparison to clinical and technical skills [16].
The preparation and adaptation of regular coursework to the online format may present a significant challenge for educators and requires comprehensive preparation to ensure that they are simple and uncomplicated for students. This shift to online learning became crucial during the COVID-19 pandemic and imposed on teachers practical and logistic hindrances. Therefore, medical schools and their staff must cooperate together to deliver transparency, communication and online resources for the new type of education [17]. Further research is needed to determine interesting and effective ways of delivery health-based content via online teaching. The implications of the current shift to e-learning for the future of medical education is difficult to predict, however it may change forever the education of subsequent generations of physicians [18].
Limitations
Our study has some limitations. It was conducted only at one medical university, however the study included a variety of participants from many countries, as the study sample comprised the English-language student group, and so none of the students were Polish nationals. Moreover, the study was conducted only among selected medical students from the 3rd year, which limits the generalisability of our findings.
Conclusions
The COVID-19 pandemic had a significant impact on the conditions of academic teaching. Teachers and students were required to shift immediately from in-person to online teaching. In general, pharmacology students at a Polish university were receptive to the new situation and adjusted to the extraordinary conditions. However, it required more effort from both the teaching staff and students themselves to continue with a consistent level of learning. The preferred methods for online learning were those that mimicked regular classes, i.e. student-oriented teaching, real-time classes and discussions. It must be emphasised that the teaching of a complicated subject, such as pharmacology, during this pandemic has been challenging and required the development of new methods of active learning/teaching. The far-reaching consequences of online learning have not yet been discussed and may become the subject of future studies.
Disclosure of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the article.
Acknowledgements
The authors would like to thank students from Medical University of Gdańsk who participated in the study. Also, we would like to thank dr Iwona Gągało for her valuable support in preparing the manuscript.
Funding
None.
Conflicts of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the article.
References
| 1. |
Ghebreyesus TA. WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020 [Internet]. WHO Director General’s speeches. 2020. p. 4. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
|
| 2. |
Ortiz PA. Teaching in the time of COVID‐19. Biochem Mol Biol Educ [Internet]. 2020 May 2;48(3):201–201. Available from: https://onlinelibrary.wiley.com/doi/10.1002/bmb.21348.
|
| 3. |
Kaup S, Jain R, Shivalli S, Pandey S, Kaup S. Sustaining academics during COVID-19 pandemic: The role of online teaching-learning. Indian J Ophthalmol [Internet]. 2020;68(6):1220. Available from: https://journals.lww.com/ijo/Fulltext/2020/68060/Sustaining_academics_during_COVID_19_pandemic__The.87.aspx.
|
| 4. |
Camargo CP, Tempski PZ, Busnardo FF, de Arruda Martins M, Gemperli R. Online learning and COVID-19: a meta-synthesis analysis. Clinics [Internet]. 2020 Nov 2;75. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7605278/.
|
| 5. |
Murphy MPA. COVID-19 and emergency eLearning: Consequences of the securitization of higher education for post-pandemic pedagogy. Contemp Secur Policy [Internet]. 2020 Jul 2;41(3):492–505. Available from: https://www.tandfonline.com/doi/full/10.1080/13523260.2020.1761749.
|
| 6. |
Cleland J, Tan ECP, Tham KY, Low-Beer N. How Covid-19 opened up questions of sociomateriality in healthcare education. Adv Heal Sci Educ [Internet]. 2020 May 6;25(2):479–82. Available from: https://link.springer.com/10.1007/s10459-020-09968-9.
|
| 7. |
Al Lily AE, Ismail AF, Abunasser FM, Alhajhoj Alqahtani RH. Distance education as a response to pandemics: Coronavirus and Arab culture. Technol Soc [Internet]. 2020 Nov;63:101317. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0160791X20303006.
|
| 8. |
Rozporządzenie Ministra Nauki i Szkolnictwa Wyższego z dnia 11 marca 2020 r. w sprawie czasowego ograniczenia funkcjonowania niektórych podmiotów systemu szkolnictwa wyższego i nauki w związku z zapobieganiem, przeciwdziałaniem i zwalczaniem COVID-19 [in [Internet]. Vol. Poz. 405, Dziennik Ustaw RP. 2020 [cited 2020 Aug 6]. Available from: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20200000405.
|
| 9. |
Ahmed H, Allaf M, Elghazaly H. COVID-19 and medical education. Lancet Infect Dis [Internet]. 2020 Jul;20(7):777–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1473309920302267.
|
| 10. |
Engels F. Pharmacology education: Reflections and challenges. Eur J Pharmacol [Internet]. 2018 Aug;833:392–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0014299918303625.
|
| 11. |
Sandhu P, de Wolf M. The impact of COVID-19 on the undergraduate medical curriculum. Med Educ Online [Internet]. 2020 Jan 1;25(1). Available from: https://www.tandfonline.com/doi/full/10.1080/10872981.2020.1764740.
|
| 12. |
Rana T, Hackett C, Quezada T, Chaturvedi A, Bakalov V, Leonardo J, et al. Medicine and surgery residents’ perspectives on the impact of COVID-19 on graduate medical education. Med Educ Online [Internet]. 2020 Jan 1;25(1). Available from: https://www.tandfonline.com/doi/full/10.1080/10872981.2020.1818439.
|
| 13. |
Khalil R, Mansour AE, Fadda WA, Almisnid K, Aldamegh M, Al-Nafeesah A, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students’ perspectives. BMC Med Educ [Internet]. 2020 Dec 28;20(1):285. Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02208-z.
|
| 14. |
Kaczmarek E, Makowska M. Wymaganie obecności na zajęciach w czasie choroby jako przykład ukrytego programu studiowania medycyny [in Polish]. Ann Etyka w Życiu Gospod [Internet]. 2020 Mar 30;23(1):67–81. Available from: https://czasopisma.uni.lodz.pl/annales/article/view/7336.
|
| 15. |
Bączek M, Zagańczyk-Bączek M, Szpringer M, Jaroszyński A, Wożakowska-Kapłon B. Students’ perception of online learning during the COVID-19 pandemic. Medicine (Baltimore) [Internet]. 2021 Feb 19;100(7):e24821. Available from: https://journals.lww.com/10.1097/MD.0000000000024821.
|
| 16. |
Abbasi MS, Ahmed N, Sajjad B, Alshahrani A, Saeed S, Sarfaraz S, et al. E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work [Internet]. 2020 Dec 1;67(3):549–56. Available from: https://www.medra.org/servlet/aliasResolver?alias=iospress&doi=10.3233/WOR-203308.
|
| 17. |
Tabari P, Amini M, Moosavi M. Lessons learned from COVID-19 epidemic in Iran: The role of medical education. Med Teach [Internet]. 2020 Jul 2;42(7):833–833. Available from: https://www.tandfonline.com/doi/full/10.1080/0142159X.2020.1754376.
|
| 18. |
Rose S. Medical Student Education in the Time of COVID-19. JAMA [Internet]. 2020 Jun 2;323(21):2131. Available from: https://jamanetwork.com/journals/jama/fullarticle/2764138.
|