Duodenal diverticulum perforation mimicking acute cholecystitis – case reports and a literature review
Abstract
Background
Duodenal diverticula affect a large part of the population. It is a congenital abnormality that develops over time. The incidence of duodenal diverticulum is estimated at 22% of the population in autopsies. Only 5% of patients present symptoms and of those only 1%-2% require surgery.
Material and methods
We describe two patients who underwent surgery due to duodenal diverticulum perforation mimicking acute cholecystitis.
Results
Perforation of the duodenal diverticulum, combined the difficulty of treatment and potential for complications, is a disease with a high mortality rate. It is a subtle and difficult diagnosis due to the unspecific symptoms and a lack of generalized peritonitis. The rarity and the wide spectrum of the disease, in combination with additional factors to be considered, mean there is no standard treatment. Depending on the patient's general condition, disease advancement, age and pathological findings observable only during surgery, we can choose between conservative treatment and a wide spectrum of surgical methods.
Conclusions
Duodenal diverticular disease rarely gives any symptoms. However, even after the onset of symptoms, only 1-2% of patients require surgery. Our work is unique because we present two cases, each treated via different approach, conservative and surgical.
Citation
Łącka M, Hać S. Duodenal diverticulum perforation mimicking acute cholecystitis – case reports and a literature review. Eur J Transl Clin Med. 2022;5(1):64-70Introduction
Duodenal diverticula are a congenital abnormality that develop over time and affect a large part of the population [1]. The incidence of duodenal diverticula is estimated at 22% of the population in autopsy[2,3], with only 5% of those presenting symptoms [3] and only 1-2% of patients requiring surgery [4]. Duodenal diverticula can demonstrate a wide spectrum of symptoms due to compression of the surrounding organs, cholestasis, haemorrhage, inflammation or perforation [3, 5-12]. Perforation is an extremely rare complication and until 2013 only 162 cases were described in the literature [3, 13]. Symptoms of perforated duodenal diverticulitis are non-specific with very subtle signs in the radiological images [14]. Uncharacteristic symptoms delay the diagnosis and appropriate treatment. Therefore, perforation of the duodenal diverticula, combined with the difficulty of treatment and potential for complications, is a disease with a high mortality rate. Due to above, the most serious complications of duodenal diverticular disease are associated with a mortality rate of up to 30% [15]. In this work we present 2 cases of perforation of the duodenal diverticulum mimicking acute cholecystitis.
Materials and methods
Two patients are described, who underwent surgery due to duodenal diverticulum perforation mimicking acute cholecystitis.
Case presentations
Patient 1
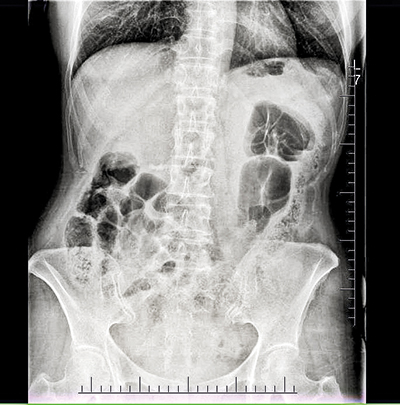
A 70-year-old woman arrived at the Emergency Department complaining of an abdominal colic pain lasting for two hours. Upon admission, the patient was in a good general condition, conscious, with effective breathing and circulation and respiratory efficiency. Her abdomen was tense, painful, with vivid peristalsis but without peritoneal symptoms. The patient did not take any medications on a daily basis and did not undergo appendectomy in the past. Her abdominal X-ray did not show any signs of perforation. See Fig 1. The gallbladder projection showed several calcified deposits of up to 8mm. The gallbladder lumen contained numerous concrements of up to 11 mm, with a normal gallbladder wall. An ultrasound examination showed no other pathological changes. The laboratory tests showed no deviations from the norm. The clinical picture suggested symptomatic biliary colic without signs of inflammation, probably due to wedging of the concrements in the neck of the follicle. Due to the persistence of the symptoms despite adequate analgesic and antispasmodics therapy, the patient was qualified for surgical treatment of acute cholecystitis and was admitted to the Department of General, Endocrine and Transplant Surgery. Less than 8 hours elapsed between the patient being admitted and the start of the surgery.
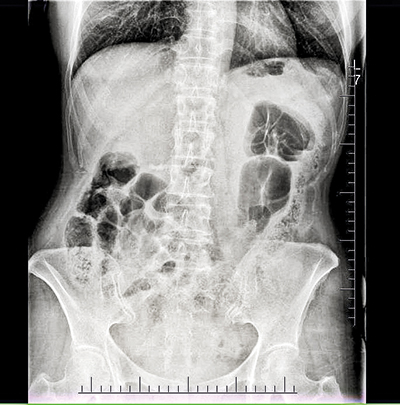
Fig 1. Patient 1 ‒ abdominal radiograph, no signs of perforation
Surgery
Laparoscopic cholecystectomy was performed. A large amount of purulent fluid in the upper abdominal cavity and an unchanged inflammation of the gallbladder was observed. Therefore, it was decided to convert from the laparoscopic to the open method. An unchanged gallbladder filled with stones was found. An inflammatory infiltration with a large amount of fibrin and a significant swelling of the duodenum, hepatic flexure of the transverse colon and mesentery of the large intestine were revealed. The retroperitoneal space was opened, Koher’s manoeuvre was performed, and the transverse hepatic ligament was cut. The pancreas and the posterior wall of the stomach were unchanged, with fibrous infiltration posterior to the head of the pancreas. After its removal, a fluid-filled reservoir (diameter ~3 cm) was visible, with a crackling sound during palpation. After opening it, a large amount of purulent content with an admixture of bile flowed out. The duodenal diverticulum in its further part was visible at the bottom of the reservoir. The perforated diverticulum was dissected. Good quality edges of perforated diverticulum, without inflammatory infiltration was observed. It was decided to perform primary suturing. Two layers of non-absorbable sutures were applied on the base of the diverticulum. A fragment of the tissue was collected for culturing and histopathological examination. A feeding probe was inserted posterior to the ligament of Treitz and a duodenostomy with a 14” Foley catheter was established. After isolating and cutting both the cystic artery and cystic duct, the gallbladder was removed subcapsularly. The peritoneal cavity was rinsed extensively. Redon drainage was placed in the right upper abdominal quadrant.
Hospitalization
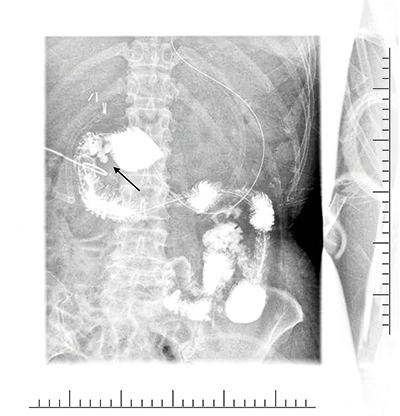
A gastrointestinal (GI) leakage test (administering contrast medium via the duodenostomy catheter) was performed 5 days after the procedure and no signs of gastrointestinal leakage were found and an undisturbed intestinal passage was shown. During the examination, a duodenal diverticulum, 23x20 mm in size, was found in the proximal duodenum. See Fig.2. During the hospitalization the inflammatory parameters decreased and the postoperative period was uneventful. The patient was discharged home after 9 days in good condition. Three days after the discharge the patient returned to the hospital due to fever and weakness. A fistulography by duodenostomy was performed. No signs of gastrointestinal tract perforation were shown. The drain was removed. Symptom relief was observed during the hospitalization. The patient was discharged home after 3 days in good condition.
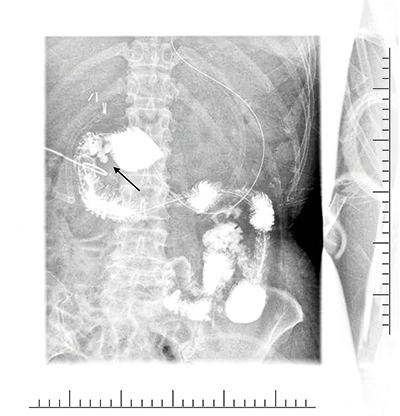
Fig. 2. Patient 1 ‒ abdominal radiograph with contrast, duodenal diverticulum marked with the arrow
Patient 2
A 77-year-old woman was admitted to the Department of General, Endocrine and Transplant Surgery for surgical treatment of acute cholecystitis. The patient presented with significant epigastric pain, positive peritoneal symptoms and vomiting. Abdominal ultrasound revealed fluid in the subhepatic region and the features of acute cholecystitis. The patient suffered from diabetes mellitus, hypertension and chronic renal failure.
Upon admission, the patient was in good general condition, conscious, with effective breathing and circulatory. The abdomen was tense, painful, with guarding over the entire surface. Peristalsis was reduced.
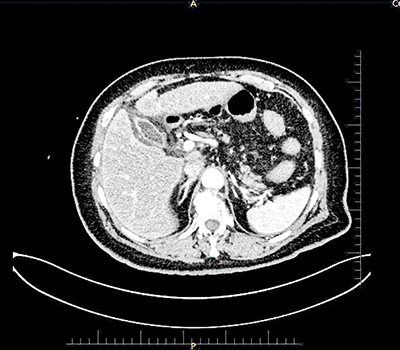
There were no radiological signs of GI obstruction or perforation in the X-ray examination. The CT scan revealed a non-dilated gallbladder, with wall thickening of up to 8 mm. There was a small amount of perivesicular fluid and obliteration of the fatty tissues around the liver cavity. The liver was not enlarged, without signs of cholestasis, without focal lesions and with features of steatosis. The pancreas was normal in size, lobular, without secreting lesions. A small amount of intrahepatic fluid (layer thickness of up to 1 cm) was observed, and a small amount of fluid was observed in the abdomen. The conclusion was that the CT image might correspond to cholecystitis. A small amount of fluid was observed in the abdomen and the small pelvis. See Fig. 3.
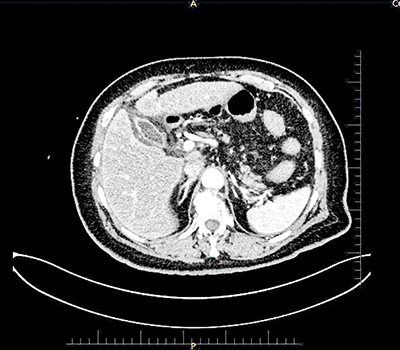
Fig. 3. Patient 2 ‒ computed tomography image
Surgery
Less than 8 hours elapsed between the patient's admission to the hospital and the start of the planned laparoscopic surgery. Large amount of purulent fluid with bile was found in the epigastric region. A thin-walled gallbladder with bile leakage from single point wall perforation was seen. Therefore, it was decided to convert to the open surgery method. No further changes were noted in the gallbladder, no stones were found. The appearance of fluid in the abdomen and the sequence of clinical symptoms indicated the possibility of GI perforation. Koher’s manoeuvre was performed, and a GI leak test was performed by injecting air into the nasogastric tube, with no GI leakage being found. The abdominal cavity was revised. Except the perforation of the gallbladder, no pathologies were seen. The gallbladder was removed, and underwent histopathological examination. The abdominal cavity was rinsed extensively, and peritoneal drainage was attached.
Hospitalization
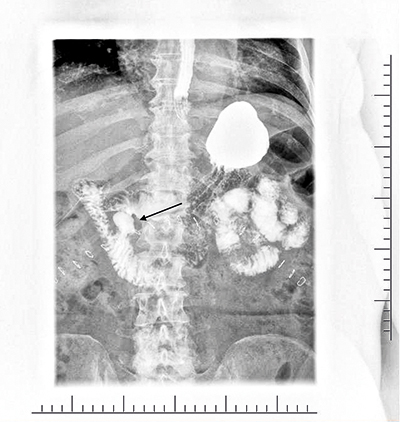
The histopathological examine showed Balser’s fat necrosis with an abscess that could be caused by pancreatic fluid. Due to not finding the site of the perforation during surgery, an upper GI X-ray with contrast was performed on the 5th post-operative day. A duodenal diverticulum, 27x17mm in size, with a 12mm wide base was seen on the medial part of the duodenum. See Fig. 4. No GI leakage was observed. Decreases in the inflammatory parameters were observed during hospitalization. The patient was discharged home in good condition after 8 days of hospitalization.
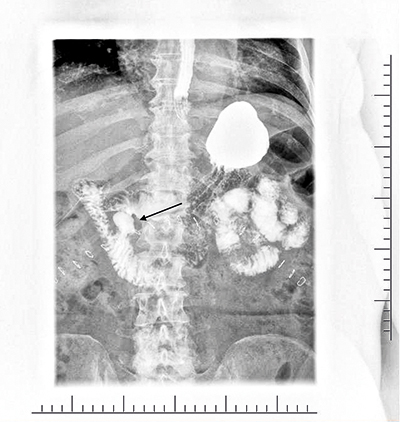
Fig. 4. Patient 2 ‒ abdominal radiograph with contrast, duodenal diverticulum marked with the arrow
In this case, the entire clinical picture supported the following sequence of events. First, perforation of the duodenal diverticulum caused the release of digestive fluids and pancreatic fluid into the peritoneal cavity. The pancreatic fluid later caused Balser’s necrosis within the omentum and necrotic gallbladder damage. Necrosis perforation also occurred on the gallbladder wall. Non-specific symptoms led to a misdiagnosis of acute cholecystitis. After opening the peritoneal cavity, perforation of non-inflamed gallbladder wall and symptoms of GI perforation were seen. At the same time, GI perforation was not confirmed during the radiological diagnosis nor during the laparotomy, which prompted the implementation of conservative treatment. The X-ray with contrast showed a duodenal diverticulum. It can therefore be assumed that the perforation of the duodenal diverticulum had been taped already during the surgery. Only the entire clinical picture, with observations from surgery combined with the CT scan and subsequent X-ray GI leakage test, allowed definitive diagnosis.
Surgical treatment did not concern the treatment of the perforation, but only its complications: damage of gallbladder wall and bile leakage. This seems to suggest that the problem of perforated diverticulum was successfully resolved by conservative treatment.
Discussion
Perforation of the duodenal diverticulum, combined with the difficulty of treatment and potential for complications, is a disease with a high mortality rate. It is a subtle and difficult diagnosis due to the unspecific symptoms and the lack of generalized peritonitis [16]. The diagnosis can be so difficult that, as in the case of our Patient 2, perforation of the duodenal diverticulum may not be diagnosed either in radiological imaging before surgery or even during laparotomy. Only the entire clinical picture, postoperative imaging examination and the presence of Balser’s fat necrosis in the histopathological examination of the gallbladder allowed the diagnosis of perforation of the duodenal diverticulum. In this case the only radiological examination that could facilitate the diagnosis before surgery was X-ray examination with a sip of contrast. This is a procedure that could be taken into account in the event of an atypical clinical picture. However, due to the rarity of the disease, it should not be a routine procedure.
These unique cases allowed us to collect material for this insidious and dangerous disease mimicking one of the most common diseases in the population – acute cholecystitis. Due to the rarity of the disease and the additional factors to be considered when treating this disease, there is no standard treatment protocol. Depending on the patient's general condition, disease advancement, age of the patient and changes often only seen during surgery, we can choose between conservative treatment or a wide spectrum of surgical methods.
Non-operative (conservative) management can be considered for carefully-selected, stable patients, after quick and accurate diagnosis of low disease severity [17]. In a 1992 review of the world literature on this subject, only 2 of the 101 published cases were managed by nonoperative methods [14, 18]. Conservative treatment consists of fasting, nasogastric tube, a wide spectrum antibiotic therapy, and parenteral nutrition combined with vigilant observation. The occurrence of complications, e.g. retroperitoneal abscess, requires intra-abdominal drainage [19-21].
Surgical intervention should be considered in unstable patients, in septic shock with haemorrhage. It is also optimal if the disease can be diagnosed only during laparotomy. The choice of the optimal surgical method depends on the local advancement of the disease. During the procedure, the surgeon must decide based on his/her experience whether local repair is possible by removing the diverticulum and suturing the duodenum or whether it is necessary to temporarily (or permanently) bypass the duodenum or even to remove it. A very wide spectrum of surgical procedures has been described in the literature that have been performed due to duodenal diverticulum perforation. These surgical treatments include bilio-enteric bypasses, Roux-Y choledochojejunostomy, duodenojejunostomy and even pancreatoduodenectomy [22-23]. Sometimes surgical treatment requires duodenal diversion: distal gastrectomy, truncal vagotomy or gastrojejunostomy [24]. The standard operative treatment option is diverticulectomy [16, 25]. If locally advanced inflammation permits, the treatment of choice is diverticulectomy with repairs to the defect involving two layers of sutures [19, 26]. Interestingly, although diverticulectomy is considered the procedure of choice, it carries a high risk of duodenal fistula formation, which is associated with a mortality rate of up to 30% [17].
In the literature, diverticulectomy is burdened with a high percentage of complications. In our case, there were no complications related to this procedure. It should be assumed that success in this case was a careful assessment of the healing of the edges of the duodenal wall, otherwise the seemingly simplest procedure for the surgeon (in that case diverticulotomy) should be abandoned. However, it should be remembered that the emergency laparotomy was performed due to suspected cholecystitis. Not every surgeon will take this step and remove the duodenum if necessary due to local advancement of the disease. Therefore, it cannot be ruled out that a large percentage of complications after diverticulectomy may be due to an over-optimistic assessment of the sutured tissue or lack of experience.
Patient 1 was in good general condition, with no comorbidities and no signs of malnutrition. Several hours had passed since the onset of the symptoms. This, combined with low local advancement of the inflammation, allowed the implementation of the standard treatment: diverticulectomy. In this case, it was correctly suspected during surgery that the cause of the symptoms was not gallbladder-related. After a thorough abdominal examination, the actual cause of the symptoms was revealed. Following careful assessment by the surgeon, it was decided to remove the diverticulum with initial duodenal wall suturing.
In Patient 2, even during the laparotomy and despite the leak test, the perforation site was not visible. This means that during the surgery the perforation site was already covered with adjacent tissues. As a result, only the gallbladder was removed. A subsequent histopathological examination showed that the perforation of the gallbladder wall was caused by the release of digestive fluids and pancreatic juice into the peritoneal cavity. In both cases, the further course of hospitalization was uncomplicated, with the patients discharged home in good general condition.
Conclusion
Our work is unique because we present two cases of duodenal diverticulum perforation treated via two different approaches: conservative and surgical. In nearly 90% of cases reported in the literature, the definitive diagnosis was not made until the operation. It can be seen, therefore, that the perforation of the duodenal diverticulum is such an insidious disease that even during laparotomy it can sometimes be impossible to make the final diagnosis. Doctors ordering and assessing the abdominal CT rarely suspect perforation of the duodenal diverticulum. This means it can be easy to overlook subtle symptoms that may be visible during the radiological examination. At the same time, we hope that after reading the description of the above cases, surgeons and radiologists will not be surprised by discovering perforation of the duodenal diverticula.
Funding
None.
Conflicts of interest
None.
References
| 1. |
Saavedra VL, Kane TD, Garrity SH. Surgical Management of Symptomatic Intraluminal Duodenal Diverticulum in an Adolescent. Glob Pediatr Heal [Internet]. 2018 Jan 1;5:2333794X1875524. Available from: http://journals.sagepub.com/doi/10.1177/2333794X18755240.
|
| 2. |
Ackermann W. Diverticula and variations of the duodenum. Ann Surg [Internet]. 1943 Mar;117(3):403-13. Available from: http://journals.lww.com/00000658-194303000-00007.
|
| 3. |
Andrea R. Perforated duodenal diverticulum, a rare complication of a common pathology: A seven-patient case series. World J Gastrointest Surg [Internet]. 2013;5(3):47. Available from: http://www.wjgnet.com/1948-9366/full/v5/i3/47.htm.
|
| 4. |
Bergman S, Koumanis DJ, Stein LA, Barkun JS, Paraskevas S. Duodenal diverticulum with retroperitoneal perforation. Can J Surg [Internet]. 2005 Aug 1;48(4):332 LP – 332. Available from: http://canjsurg.ca/content/48/4/332.abstract.
|
| 5. |
Rowlands BC, King PA. Duodenal diverticulum perforating into abdominal aorta causing fatal hæmorrhage. Br J Surg [Internet]. 2005 Dec 6;41(168):415–7. Available from: https://academic.oup.com/bjs/article/41/168/415/6193698.
|
| 6. |
Wijarnpreecha K, Panjawatanan P, Manatsathit W, Cheungpasitporn W, Pungpapong S, Lukens FJ, et al. Association Between Juxtapapillary Duodenal Diverticula and Risk of Choledocholithiasis: a Systematic Review and Meta-analysis. J Gastrointest Surg [Internet]. 2018 Dec 18;22(12):2167-76. Available from: http://link.springer.com/10.1007/s11605-018-3865-z.
|
| 7. |
Ko KS, Kim SH, Kim HC, Kim IH, Lee S-O. Juxtapapillary Duodenal Diverticula Risk Development and Recurrence of Biliary Stone. J Korean Med Sci [Internet]. 2012;27(7):772. Available from: https://jkms.org/DOIx.php?id=10.3346/jkms.2012.27.7.772.
|
| 8. |
Kennedy RH, Thompson MH. Are duodenal diverticula associated with choledocholithiasis? Gut [Internet]. 1988 Jul 1;29(7):1003-6. Available from: https://gut.bmj.com/lookup/doi/10.1136/gut.29.7.1003.
|
| 9. |
Tobin R, Barry N, Foley NM, Cooke F. A giant duodenal diverticulum causing Lemmel syndrome. J Surg Case Reports [Internet]. 2018 Oct 1;2018(10). Available from: https://academic.oup.com/jscr/article/doi/10.1093/jscr/rjy263/5132985.
|
| 10. |
Egawa N, Kamisawa T, Tu Y, Sakaki N, Tsuruta K, Okamoto A. The role of juxtapapillary duodenal diverticulum in the formation of gallbladder stones. Hepatogastroenterology [Internet]. 45(22):917-20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9755980.
|
| 11. |
Karagyozov P, Tishkov I, Georgieva Z, Boeva I, Tzankov D. Intraluminal duodenal (“windsock”) diverticulum: a rare cause of biliary obstruction and acute pancreatitis in the adult. Endosc Int Open [Internet]. 2019 Jan 15;07(01):E87-9. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/a-0808-3834.
|
| 12. |
Li X, Zhu K, Zhang L, Meng W, Zhou W, Zhu X, et al. Periampullary Diverticulum May Be an Important Factor for the Occurrence and Recurrence of Bile Duct Stones. World J Surg [Internet]. 2012 Nov 22;36(11):2666-9. Available from: http://link.springer.com/10.1007/s00268-012-1716-8.
|
| 13. |
Thorson CM. The Perforated Duodenal Diverticulum. Arch Surg [Internet]. 2012 Jan 1;147(1):81. Available from: http://archsurg.jamanetwork.com/article.aspx?doi=10.1001/archsurg.2011.821.
|
| 14. |
Duarte B, Nagy KK, Cintron J. Perforated duodenal diverticulum. Br J Surg [Internet]. 2005 Dec 8;79(9):877-81. Available from: https://academic.oup.com/bjs/article/79/9/877/6173422.
|
| 15. |
Bergman S, Koumanis J, Stein LA, Barkun JS, Paraskevas S. Duodenal diverticulum with retroperitoneal perforation. Can J Surg [Internet]. 2005 Aug;48(4):332. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16149371.
|
| 16. |
Kim KH, Park SH. Conservative treatment of duodenal diverticulitis perforation: A case report and literature review. Open Access Emerg Med [Internet]. 2018 Aug;Volume 10:101-4. Available from: https://www.dovepress.com/conservative-treatment-of-duodenal-diverticulitis-perforation-a-case-r-peer-reviewed-article-OAEM.
|
| 17. |
Oukachbi N, Brouzes S. Management of complicated duodenal diverticula. J Visc Surg [Internet]. 2013 Jun;150(3):173-9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1878788613000635.
|
| 18. |
Miller G, Mueller C, Yim D, Macari M, Liang H, Marcus S, et al. Perforated Duodenal Diverticulitis: A Report of Three Cases. Dig Surg [Internet]. 2005;22(3):198-202. Available from: https://www.karger.com/Article/FullText/87974.
|
| 19. |
Martínez-Cecilia D, Arjona-Sánchez A, Gómez-Álvarez M, Torres-Tordera E, Luque-Molina A, Valentí-Azcárate V, et al. Conservative management of perforated duodenal diverticulum: A case report and review of the literature. World J Gastroenterol [Internet]. 2008;14(12):1949. Available from: http://www.wjgnet.com/1007-9327/full/v14/i12/1949.htm.
|
| 20. |
Chen C-F, Wu D-C, Chen C-W, Hsieh J-S, Chen C-Y, Wang J-Y. Successful Management of Perforated Duodenal Diverticulitis With Intra-abdominal Drainage and Feeding Jejunostomy: A Case Report and Literature Review. Kaohsiung J Med Sci [Internet]. 2008 Aug;24(8):425-9. Available from: http://doi.wiley.com/10.1016/S1607-551X(08)70167-0.
|
| 21. |
Maghrebi H, Bensafta Z. Duodenal diverticulitis: a difficult clinical problem. Pan Afr Med J [Internet]. 2017;27. Available from: http://www.panafrican-med-journal.com/content/article/27/286/full/.
|
| 22. |
Philip J, Cocieru A. Pancreatoduodenectomy in patient with perforated duodenal diverticulum and peritonitis: Case report. Int J Surg Case Rep [Internet]. 2019;58:48-9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2210261219301993.
|
| 23. |
Vassilakis JS, Tzovaras G, Chrysos E, Mouzas I, Manousos O, Xynos E. Roux-Y choledochojejunostomy and duodenojejunostomy for the complicated duodenal diverticulum. Am J Surg [Internet]. 1997 Jul;174(1):45-8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0002961097000512.
|
| 24. |
Teven CM, Grossman E, Roggin KK, Matthews JB. Surgical Management of Pancreaticobiliary Disease associated with Juxtapapillary Duodenal Diverticula: Case Series and Review of the Literature. J Gastrointest Surg [Internet]. 2012 Jul 6;16(7):1436-41. Available from: http://link.springer.com/10.1007/s11605-012-1856-z.
|
| 25. |
Economides NG, McBurney RP, Hamilton FH. Intraluminal Duodenal Diverticulum in the Adult. Ann Surg [Internet]. 1977 Feb;185(2):147-52. Available from: http://journals.lww.com/00000658-197702000-00003.
|
| 26. |
Mackay AG, Pace HG. Diverticulitis of the Duodenum with Perforation. Ann Surg [Internet]. 1955 Dec;142(6):1034-7. Available from: http://journals.lww.com/00000658-195512000-00025.
|