Abstract
Background
The coronavirus pandemic has strongly affected health-care systems around the world, testing their patients’ care capacities. Admission restrictions, patients’ fear of hospitalization or other uncomprehended constraints has affected admissions to neurosurgery department.
Material and methods
The clinical data of admissions from March 1st to July 24th 2020, as well as data of the control group in relevant periods of time in 2019 was collected from the local hospital database and compared.
Results
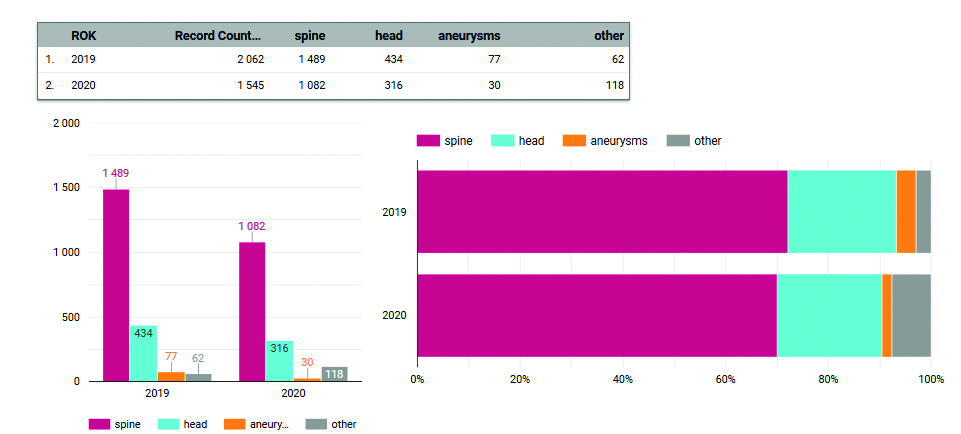
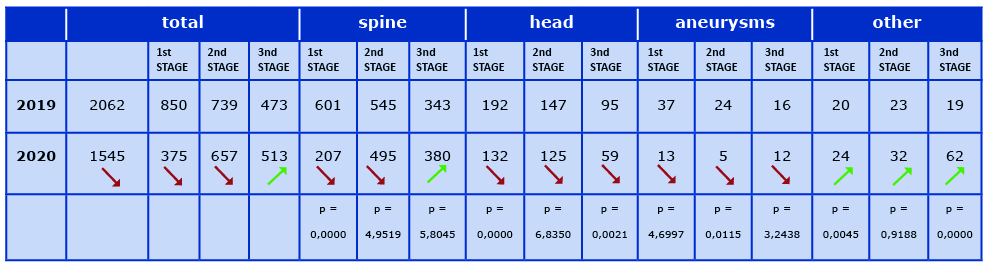
The total number of procedures performed between March and July 2020 is 1545, compared to the corresponding period of the previous year it was the number of 2062, indicating a decrease by about 25%. Both head and aneurysm procedures decreased over the entire analyzed period. The number of procedures classified as "other" was higher in each of the three stages. Between March 1st and April 30th (Phase 1) mainly younger male patients were admitted.
Conclusions
We demonstrated the impact of the COVID-19 pandemic on the work organization of our Neurosurgery Department. We report that after the introduction of appropriate solutions, it is possible to provide care to neurosurgical patients while ensuring the safety of patients and Staff during the pandemic.
Citation
Fercho J, Szmuda T, Ali S, Szplit D, Jurkiewicz A, Słoniewski P, Stefaniak T. Changes in the neurosurgical admissions during the COVID-19 pandemic – a comparison with 2019. Eur J Transl Clin Med. 2021;4(1):22-28Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first diagnosed in December 2019 in the city of Wuhan, Hubei Province in China. The disease caused by the virus, COVID-19, can lead to severe respiratory failure. Within a few months of the first reported case, SARS-CoV-2 spread throughout the world. It was designated by the World Health Organization (WHO) a pandemic on March 31, 2020. The non-specific symptomatology, high infectivity, inexistence of a vaccine and a lack of effective treatment hampered efforts to contain and manage patients infected by SARS-CoV-2. In Poland, the first case of a SARS-CoV-2 infection confirmed by laboratory test was announced officially on March 4th 2020. Since then, health care facilities started implemented a number of procedures and solutions aimed at reducing the number of COVID-19 cases. In particular, planned admissions and hospitalizations were severely limited. This challenged the health care staff to provide patient care, while ensuring safety amidst the patients’ fear of being infected with the novel virus.
In this paper, we highlight the specific conditions and efficient management methods that a neurosurgery department took in Poland. We present the pattern of neurosurgical patient admissions to a single center during 2020, depending on the phase of adaptation to the COVID-19 pandemic. We hope that this information may lead to a more calm and predictable response during any future pandemics.
Materials and Methods
We examined the admissions to the Neurosurgery Department at the University Clinical Center (UCC) of the Medical University of Gdańsk (a tertiary care, neurotrauma centre serving a population of 1 million). The study sample consisted of data about the number and types of procedures performed from March 1st to July 24th 2020. The control group consisted of procedures performed from March 1st to July 24th 2019. Simultaneously, we collected information about the changes in restrictions associated with patient care and hospital staff safety since the SARS-CoV-2 outbreak in Poland.
Data acquisition
The clinical data of were collected from the hospital’s patient record system (CLININET, CompuGroup Medical, Lublin, Poland) using the IT tool MedStream Designer (MSD, Transition Technologies Co., Warsaw, Poland). Data related to patients undergoing COVID-19 swabs before or during hospitalization were obtained from the hospital’s COVID-19 database which has been functioning since the in-house laboratory began testing for SARS-CoV-2.
We divided the neurosurgical procedures into four groups: spinal procedures, head surgeries (brain tumors, hematomas, ventriculoperitoneal shunt insertion), aneurysm-securing procedures and other miscellaneous procedures.
Phases of the pandemic
We divided the time from the study period into three stages based on the legal and organizational regulations implemented both at the national and hospital level. We attempted an overall quantitative and qualitative comparative analysis, considering both the type of procedures between and within the given stage of the pandemic.
Stage 1, which we will call “the Lockdown,” lasted from March 1st to April 30th when our hospital was in a state of high alert. During this time all planned admissions to the Neurosurgery Department were suspended and its function was limited to emergency admissions only. Throughout the hospital, numerous restrictions and strict guidelines were introduced for patient care, as well as to ensure the safety of all hospital employees. Furthermore, family visits, bedside teaching and internships for doctors were also suspended.
Stage 2, which we will call “Unlocking,” started on April 30th, when the planned procedures were gradually performed and the access to the operating room was increased. Numerous limitations and special guidelines were still in place, however they allowed somewhat flexibility and were adjusted to the patients' planned treatment options.
Stage 3, which we will call “riding out the storm,” started on June 22nd, when all newly admitted patients underwent SARS-CoV-2 testing and then waited at home under self-quarantine for their results. This was the so-called, “kiss and fly” system.
Supplementary figure 1. Pandemic milestones in Poland ‒ timeline. Abbreviations: UCC: University Clinical Centre. → https://ejtcm.gumed.edu.pl/files/62
Supplementary table 1. General rules for admissions during a pandemic by stage. → https://ejtcm.gumed.edu.pl/files/65
Comparative analysis
The overall number of procedures performed between March 1st and July 24th 2020 (both as a whole and in the individual stages of the pandemic) were compared with procedures performed in the corresponding time period in 2019. We took into account the type of procedure, the patients’ age and sex.
Statistical methods
Continuous variables were described by mean and standard deviation (SD) and were tested for normal distribution using the Shapiro-Wilk test. The differences between groups were identified respectively by means of a t-test, Mann-Whitney U test, chi square or two-tailed Fisher test using Statistica v. 12.0 (StatSoft, Inc., Tulsa, USA). We considered p values < 0.05 as statistically significant.
Results
Total procedures: 2019 versus 2020
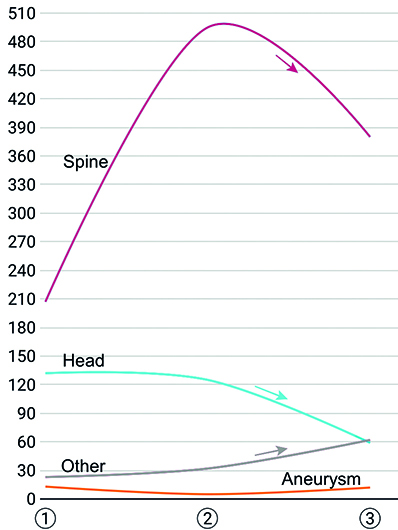
The total amount of procedures performed during the study period decreased by 25% (from 2062 to 1545) compared to the time time period in 2019 (Table 1). Both aneurysms and head procedures decreased throughout all three analyzed phases of the pandemic. Not only was there a smaller total number of aneurysms, but also they were a smaller portion of the procedures performed in 2020. We observed the highest decrease in spinal procedures during Phase 1. This was due to hospital-related restrictions, however during Phase 3 this number started to increase. Parallel to this drop, we observed that the number of “other” procedures grew steadily.
Table 1. The number of performed neurosurgical procedures - a comparison between March 1st to July 24th in 2019 and 2020
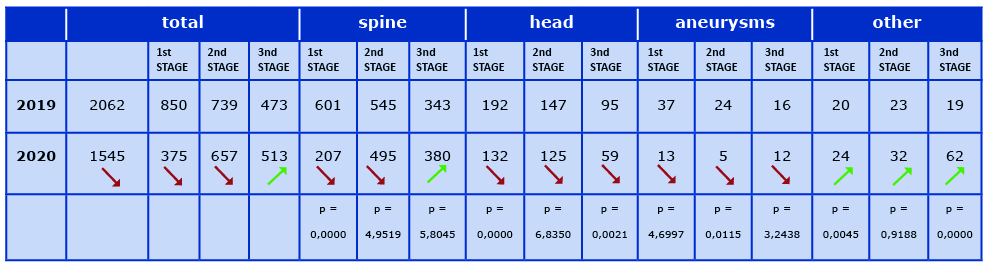
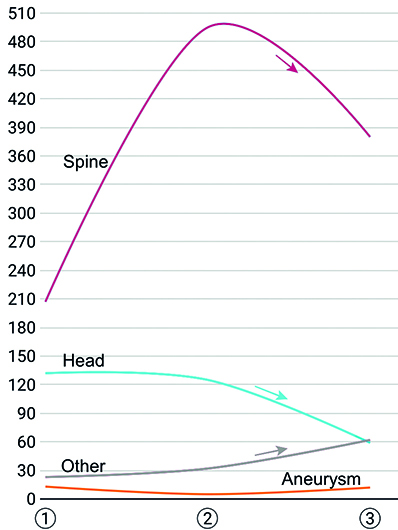
Figure 1. Average distribution of neurosurgery clinic admissions
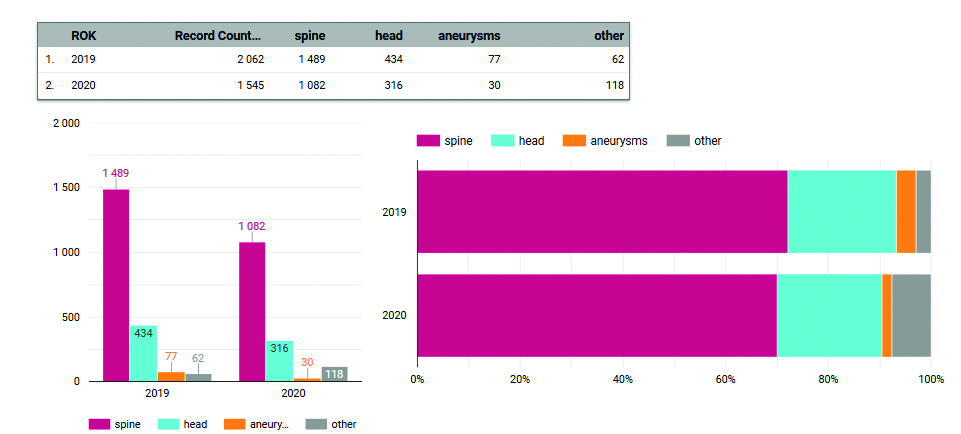
Figure 2. Qualitative distribution of performed procedures – comparison between 2019 and 2020
Supplementary figure 2. Waterfall-plot depicting admission changes in pandemic phases. Explaining how the number of each type of performed procedures changed from 2019 to 2020. The gray rectangle shows the deficit between these years. → https://ejtcm.gumed.edu.pl/files/63
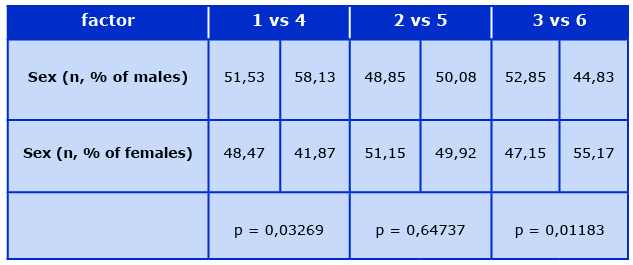
Age and sex of admitted patients
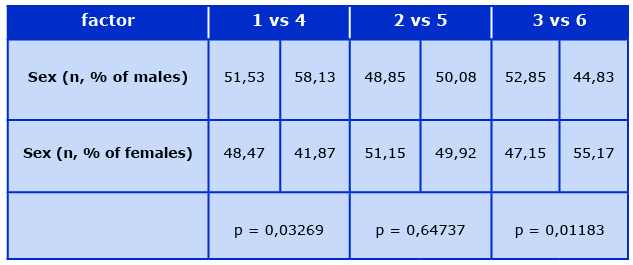
More younger patients were admitted during Phase 1 (March 1st – April 30th 2020) compared to the corresponding time the year before (P = 0.05). Since April 30, 2020, there were no differences in patient age compared to the same months in 2019. Significantly more males than females were admitted in Phase 1 of the pandemic (P = 0.03). On the contrary, since the beginning of Phase 3, we observed a greater proportion of female patients (P = 0.01). Details are presented in Table 2.
Supplementary figure 3. Age structure presentation between 2019 and 2020; The corresponding timeframes (1-4 ; 2-5; 3-6) were compared statistically. → https://ejtcm.gumed.edu.pl/files/64
Table 2. Hospital admissions by sex a comparison between the 3 phases of the pandemic
Stage 1, The Lockdown
We observed a significant decrease in the number of spine, head and aneurysm procedures during Phase 1. For the other procedures, a slight increase was observed.
Stage 2, Unlocking
During Phase 2, there was almost a complete equalization in the number of spine and head procedures. However, there was a dramatic decrease in aneurysm procedures compared to the same time period in 2019. During this phase, we observed a further increase in other procedures compared to the previous year.
Stage 3, Riding out the Storm
We observed an increase in spine procedures during Phase 3 as compared with the same time period in 2019. There was a decrease in the number of head and aneurysm procedures at that phase in 2020. An increase in, “other” procedures was observed.
Discussion
Despite the several changes to clinical practice due to the COVID-19 pandemic, we found that the total amount of performed procedures decreased only by 25%. Our comparison to the same time period in 2019 aimed to demonstrate to what extent neurosurgery practice during the pandemic differed from the usual.
Applied restrictions – a detailed historical account
“The Lockdown”
In March of 2020 the UCC in Gdańsk implemented a detailed action plan. First, patient visits were suspended at all departmentsalong with internships. On March 12th, the UCC was put on high alert in connection with the SARS-CoV-2 pandemic. Most scheduled admissions were suspended, with the exception of patients with oncological, transplantation, chemotherapy, ophthalmology, pregnancy and puerperium, pediatric-related needs or who were enrolled in special drug programs. SARS-CoV-2 risk was assessed via obligatory telephone epidemiological interview and body temperature measurement along with paper questionnaire upon arrival at the Scheduled Admission Center and Day Wards. Heads of Departments and other organizational units of UCK were obliged to ensure daily body temperature measurements of all employees at the start of each shift or working day. The activities of specialist clinics had to be carried out with the use of ICT systems [1]. Detailed patient management regimens were introduced at the emergency department. Stable patients had standard PCR tests for SARS-CoV-2, whereas Rapid-PCR was performed in urgent cases. If the patient's clinical condition could not afford any delays for the result of SARS-CoV-2 test, the operating procedure was performed using personal protective equipment, as if the patient had tested positive. During the complete “Lockdown” the number of performed procedures decreased dramatically, mainly due to the complete suspension of planned admissions. From March 12th, the department was limited to emergency admissions and on-call interventions. The number of spine and aneurysms procedures has decreased significantly, while the number of head interventions increased. This was probably due coding the admissions in the patient record system as emergencies and with the lack of planned spine surgeries. Moreover, there was a marked increase in “other” procedures. COVID-19 testing procedures were categorized under, “other” category. Therefore, this increase may have been related to the need for a SARS-CoV-2 swab before each admission. Notably, some of the testing-swabs were performed at the Emergency Department and therefore are not included in the presented data.
“The Unlocking”
On April 30th 2020, the admission and treatment of planned patients started gradually. For the Neurosurgery department this meant about 2 to 4 planned admissions per day, depending on the expected operating time. Each elective patient underwent a SARS-CoV-2 swab and awaited the result at a “buffer ward.” At that time, the physician conducted the epidemiological interview with the patient by phone. In the case of emergency admissions, the procedures were the same as during the “Lockdown” stage. This made it possible to almost equalize the number of emergency procedures performed in relation to the previous year. Both spine and head procedures constituted a fraction of treatments comparable to 2019. The number of aneurysm procedures had decreased, while “other” procedures still accounted for a noticeably higher proportion than previous years.
“Riding out the storm”
The “kiss and fly” system enabled complete unlocking of the Neurosurgery Department. The average waiting time for the SARS-CoV-2 result with a standard swab was about 3 to 5 hours depending on the laboratory workload, while the Rapid-PCR, in urgent situations, took about 1 hour. The above-mentioned solutions allowed not only to match, but also exceeded the number of procedures performed during typical clinical practice. Both spine and aneurysm procedures represented a fraction of treatments comparable to the pre-pandemic norm, while the fraction of head procedures decreased drastically. This is most likely due to a re-increase in elective procedures which, overall, reduces the percentage of urgent cases such as hematomas. As for the number of other procedures, it is still higher than typically. We assert that the obligation to test each patient for COVID-19 increases the number of this particular fraction.
Discussion with the main findings
Discussion with the main findings Older people have a worse prognosis and during the pandemic their hospitalization increased the threat to their health. The risk of serious comorbidities increases with age, as well as the severity of COVID-19. Older patients were not only less willingly hospitalized, but alsowere motivated by fear and may have decided to visit their doctor less often.
The male predominance in the admission profile could possibly result from hospital restrictions solely to emergency cases in the initial phase of the lock-up. Due to neurotrauma status of the hospital these were patients after head or back injuries.
It is worth noting that by the time this paper was written, none of the patients admitted to the neurosurgery department had a positive result for SARS-CoV-2. In the hospital’s pre-hospitalization screening, it was possible to capture 5 patients with a positive result (out of the total number of 11548 performed tests). According to the worldometer.com, at this time Poland was found at the 9th place worldwide in the ranking of the most infected cases per million people. Due to this, they were transferred to an infectious disease hospital or placed under home quarantine. However, for safety reasons, each patient admitted to the hospital was regarded as an asymptomatic infected patient as per previous recommendations [2].
Neurosurgical departments around the world
In India, the neurological and neurosurgical departments have categorized cases into three groups according to their priority: acute, sub-acute and chronic. Full personal protective equipment should be used during procedures involving a high risk of aerosol dispersion, i.e. those requiring intubation and procedures using drills or endoscopes [2].
Since most hospital visits in China are now performed remotely, there has been a significant decrease in reported physician-patient conflicts and cases of violence in hospitals, which have been of great concern so far [3].
In Lombardy (Italy), an internet platform for conference calls and radiographic image sharing was established and the patient waitlist was limited to oncological cases. Patients were categorized according to the severity of disease into 3 classes: A ++, A + and A [4]. An important educational step in response to the epidemiological situation was to increase cooperation between the centers, and thus the exchange and enrichment of surgical skills and experience [4-5].
In Bergamo (Italy), the regional neurosurgical network was concentrated at four hub hospitals. These hospitals were able to handle urgent surgical cases, so that the remaining centers focused on helping patients with COVID-19 [6].
At the University of Miami Jackson Memorial Hospital, all scheduled admissions were canceled and patients are admitted to the clinic after screening based on a survey and body temperature. Surgeons tried to use only dissolvable sutures so that they do not have to be removed later, allowing for a remote follow-up visit [7].
Elsewhere in the United States, the development of telehealth was also emphasized, proving its political, research and clinical application [8]. The authors emphasized that the provision of personal protection measures as well as broadly understood cooperation was critical during the pandemic [9].
In a survey conducted among 226 respondents around the world, all agreed that rapidly developing neurooncological conditions are non-emergency cases with the greatest risk associated with postponing treatment, however vascular events may be at high risk when delayed [10].
Any novel pandemic requires flexibility and deliberate compromises from everyone. The introduction of initial restrictions was necessary to reorganize the work of the hospital to ensure the safety of inpatients and staff [11]. However, since closures could not last indefinitely, solutions had to be found to enable the normal functioning of the hospital. Partial defrosting was a transitional stage designed to test the safety of new solutions. However, fast adaptation has been shown to be the most important step in fighting the pandemic [12].
Clinical Implications and Future Directions
Using the example of our center, we hope to show other health institutions that medical care delivery is possible with the introduction of appropriate system solutions. We assert that learning to adapt in the new COVID-19 pandemic is the only way to prevent paralysis and failure of the healthcare system. As we may face a new surge of COVID-19 cases, we encourage physicians to react with quick and prudent solutions to enable their clinic to function as normally as possible.
During the work on this article, the epidemiological situation in Poland changed dramatically. The sharp increase in the number of cases showed that the period between March and July 2020 was only a prelude to the first wave of the pandemic in Poland. As it turns out, this was crucial for the organization of the actions that are currently being undertake.
Conclusions
We demonstrated our department’s preparedness for admission of trauma cases despite the restrictions in place due to the COVID-19 pandemic. Stage 1 patients were predominantly younger males. In the early phase of any future epidemic we recommend disqualifying older patients from elective neurosurgery. The number of “other” non-surgical cases significantly increased. This may possibly be due to the additional procedures such as SARS-CoV-2 screening tests required prior to admission. Patients with spinal disorders suffered the most during the early phase of the COVID-19 pandemic. The reason is that these are usually life-enhancing, not life-saving procedures. In a pandemic, the admission profile changed and only urgent and life-saving neurosurgical interventions were undertaken.
References
| 1. |
Ozoner B, Gungor A, Hasanov T, Toktas ZO, Kilic T. Neurosurgical Practice During Coronavirus Disease 2019 (COVID-19) Pandemic. World Neurosurg [Internet]. 2020 Aug;140:198–207. Available from: https://doi.org/10.1016/j.wneu.2020.05.195.
|
| 2. |
Gupta P, Muthukumar N, Rajshekhar V, Tripathi M, Thomas S, Gupta S, et al. Neurosurgery and neurology practices during the novel COVID-19 Pandemic: A consensus statement from India. Neurol India [Internet]. 2020;68(2):246. Available from: https://doi.org/10.4103/0028-3886.283130.
|
| 3. |
Sun Y, Mao Y. Editorial. Response to COVID-19 in Chinese neurosurgery and beyond. J Neurosurg JNS. 2021;133(1):31–2.
|
| 4. |
Cenzato M, DiMeco F, Fontanella M, Locatelli D, Servadei F. Editorial. Neurosurgery in the storm of COVID-19: suggestions from the Lombardy region, Italy (ex malo bonum). J Neurosurg [Internet]. 2020 Jul;133(1):33–4. Available from: https://doi.org/10.3171/2020.3.JNS20960.
|
| 5. |
Zoia C, Bongetta D, Veiceschi P, Cenzato M, Di Meco F, Locatelli D, et al. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir (Wien) [Internet]. 2020;162(6):1221–2. Available from: https://doi.org/10.1007/s00701-020-04305-w.
|
| 6. |
Bernucci C, Brembilla C, Veiceschi P. Effects of the COVID-19 Outbreak in Northern Italy: Perspectives from the Bergamo Neurosurgery Department. World Neurosurg [Internet]. 2020 May;137:465-468.e1. Available from: https://doi.org/10.1016/j.wneu.2020.03.179.
|
| 7. |
Eichberg DG, Shah AH, Luther EM, Menendez I, Jimenez A, Perez-Dickens M, et al. Letter: Academic Neurosurgery Department Response to COVID-19 Pandemic: The University of Miami/Jackson Memorial Hospital Model. Neurosurgery [Internet]. 2020 Jul 1;87(1):E63–5. Available from: https://doi.org/10.1093/neuros/nyaa118.
|
| 8. |
Wright CH, Wright J, Shammassian B. COVID-19: Launching Neurosurgery into the Era of Telehealth in the United States. World Neurosurg [Internet]. 2020 Aug;140:54–5. Available from: https://doi.org/10.1016/j.wneu.2020.05.092.
|
| 9. |
Carter BS, Chiocca EA. Editorial. COVID-19 and academic neurosurgery. J Neurosurg [Internet]. 2020 Jul;133(1):8–9. Available from: https://doi.org/10.3171/2020.4.JNS201013.
|
| 10. |
Jean WC, Ironside NT, Sack KD, Felbaum DR, Syed HR. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien) [Internet]. 2020 Jun 21;162(6):1229–40. Available from: https://doi.org/10.1007/s00701-020-04342-5.
|
| 11. |
Khalafallah AM, Jimenez AE, Lee RP, Weingart JD, Theodore N, Cohen AR, et al. Impact of COVID-19 on an Academic Neurosurgery Department: The Johns Hopkins Experience. World Neurosurg [Internet]. 2020 Jul;139:e877–84. Available from: https://doi.org/10.1016/j.wneu.2020.05.167.
|
| 12. |
Pressman E, Noureldine MHA, Kumar JI, Krafft PR, Mantei B, Greenberg MS, et al. The Return Back to Typical Practice from the “Battle Plan” of the Coronavirus Disease 2019 (COVID-19).
|